Steroid-Induced Osteoporosis Risk Calculator
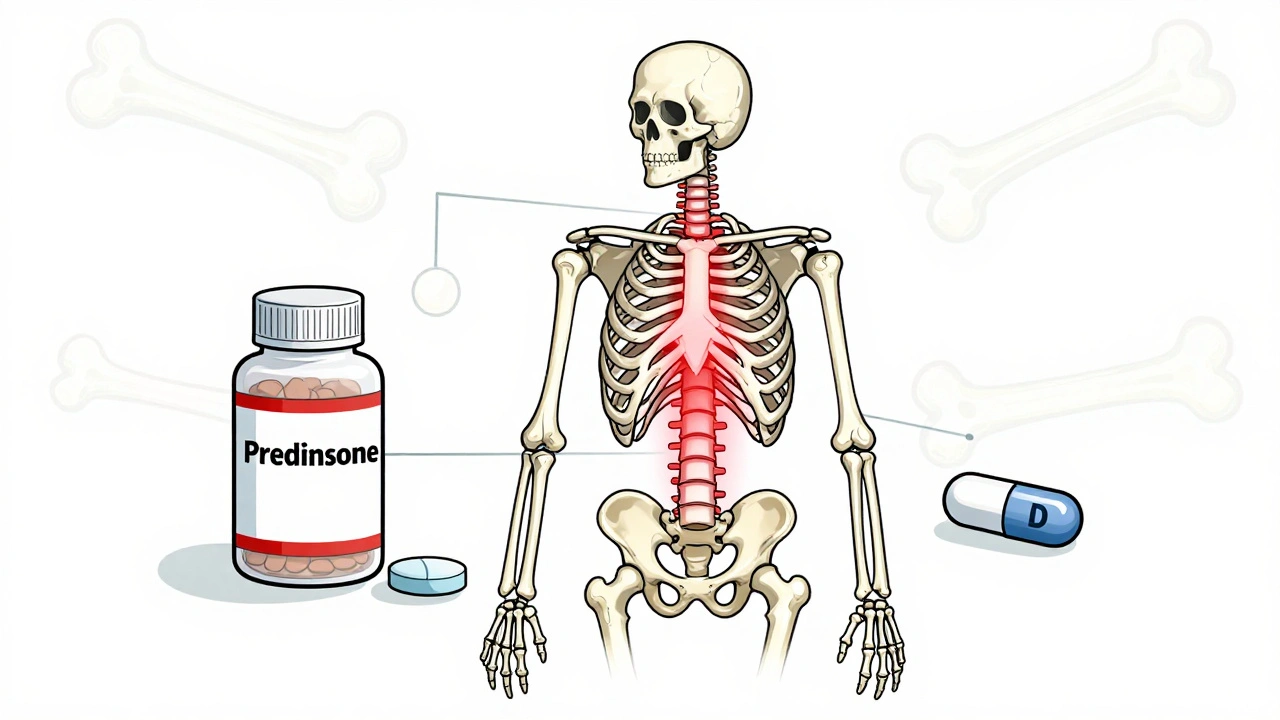
When you start taking steroids-whether for asthma, rheumatoid arthritis, or an autoimmune condition-you’re not just fighting inflammation. You’re also quietly putting your bones at risk. Glucocorticoid-induced osteoporosis (GIOP) is the most common type of secondary osteoporosis, and it doesn’t wait years to strike. Bone loss can begin in as little as three to six months after starting treatment, especially if you’re on a daily dose of 5 mg or more of prednisone. By the end of the first year, up to 12% of people on these doses will suffer a vertebral fracture. That’s not a small risk. It’s a silent epidemic, and most people don’t even know it’s happening until they break a bone.
Why Steroids Attack Your Bones
Steroids don’t just weaken bones-they reprogram how they’re built. Your skeleton is always renewing itself: old bone is broken down by cells called osteoclasts, and new bone is made by osteoblasts. Steroids mess with both sides of this balance. They shut down osteoblasts, cutting bone formation by up to 70%. At the same time, they wake up osteoclasts, speeding up bone breakdown by 30%. The result? Your bones lose density fast, and they don’t rebuild well enough to catch up.This isn’t just about older people. Even young adults on long-term steroids can develop severe bone loss. The damage shows up first in the spine and hips-areas that bear weight and are most vulnerable to fractures. And unlike age-related osteoporosis, GIOP doesn’t wait for menopause or aging. It hits hard and fast.
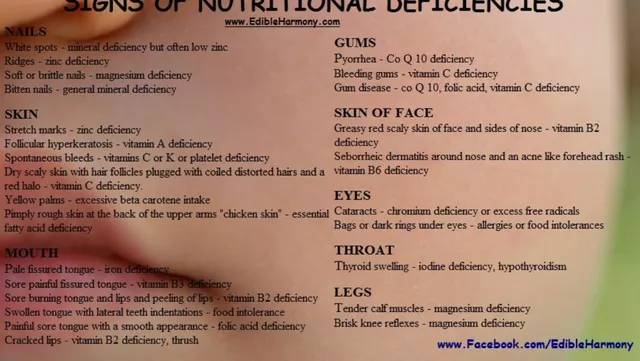
Calcium and Vitamin D: The Foundation
Before you even think about pills that stop bone loss, you need the basics: calcium and vitamin D. These aren’t optional extras-they’re the building blocks. The American College of Rheumatology says everyone starting long-term steroid therapy should get 1,000 to 1,200 mg of calcium daily and 600 to 800 IU of vitamin D. If your blood levels are low (under 30 ng/mL), bump vitamin D up to 800-1,000 IU.Calcium keeps your bones dense. Vitamin D helps your body absorb that calcium. Without enough vitamin D, even the most expensive calcium supplement won’t help. Studies show that people who take both have significantly slower bone loss than those who don’t. But here’s the catch: most people don’t get enough from diet alone. A glass of milk has about 300 mg of calcium. You’d need four glasses a day to hit the target. That’s why supplements are usually necessary.
Don’t just grab any supplement. Look for calcium citrate if you have low stomach acid-it’s better absorbed. Take calcium in doses of 500 mg or less at a time; your body can’t absorb more than that at once. And always take vitamin D with a meal that has fat. It’s a fat-soluble vitamin, so it needs fat to work.
Bisphosphonates: The First-Line Defense
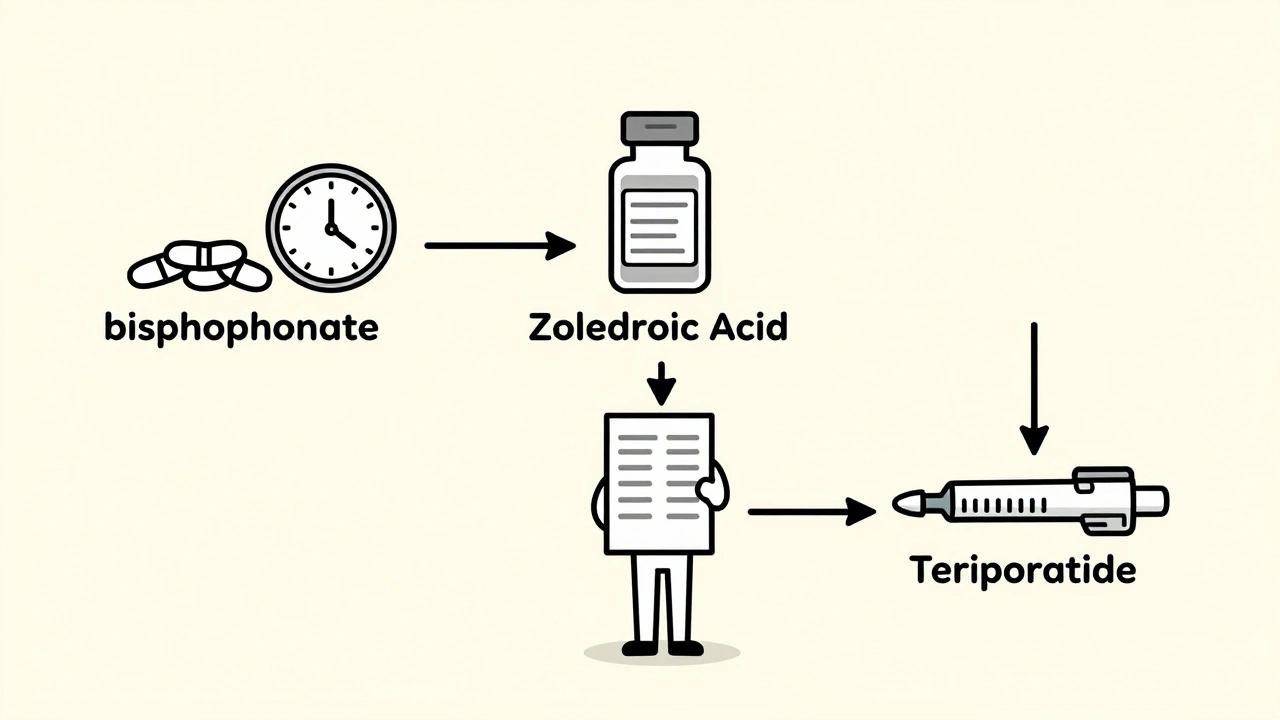
If you’re on steroids for more than three months and you’re over 40, or if you’ve had a fracture before, you need more than calcium and vitamin D. You need a bisphosphonate. These are the most studied, most effective drugs for preventing steroid-induced bone loss. The two most common are alendronate (Fosamax) and risedronate (Actonel), both taken once a week.Here’s what they do: they stick to bone surfaces and slow down osteoclasts-the cells that chew up bone. They don’t build new bone, but they stop the destruction. In clinical trials, alendronate increased spine bone density by 3.7% in one year, while people on placebo lost bone. Risedronate cut vertebral fracture risk by 70% in the first year of steroid use.
These drugs aren’t perfect. You have to take them right. Take them first thing in the morning, on an empty stomach, with a full glass of water. Stay upright for at least 30 minutes. Lie down too soon, and you risk serious irritation to your esophagus. About 15-25% of people have stomach upset or heartburn. If that happens, talk to your doctor. There are alternatives.
When Bisphosphonates Aren’t Enough
Some people need stronger options. If you’ve already had a fracture, your bone density is below -2.5 T-score, or you’re under 40 with multiple risk factors, bisphosphonates might not be enough. That’s where teriparatide (Forteo) comes in. Unlike bisphosphonates, teriparatide doesn’t just slow bone loss-it builds new bone. It’s a synthetic version of parathyroid hormone, given as a daily injection.In a major study, teriparatide reduced new vertebral fractures to just 0.6% over 18 months, compared to 6.1% with alendronate. That’s a massive difference. But it comes with a price tag: around $2,500 a month, versus $250 for generic bisphosphonates. It’s also only approved for two years of use. After that, you usually switch to a bisphosphonate to hold onto the gains.
Another option is zoledronic acid (Reclast), given as an IV infusion once a year. It’s more effective than oral bisphosphonates at improving hip bone density and cuts hip fracture risk by 41%. It’s also easier to stick with-no daily pills, no upright waiting. For people who struggle with adherence, this is often the best choice.
Who Should Get What?
There’s no one-size-fits-all. Here’s how doctors decide:- Everyone on steroids for 3+ months at ≥2.5 mg prednisone/day: start calcium and vitamin D immediately.
- Age 40+ with the same steroid dose: add a bisphosphonate (alendronate or risedronate).
- Age under 40 with prior fracture or T-score ≤-2.5: consider teriparatide.
- Can’t tolerate oral bisphosphonates? Try zoledronic acid or denosumab (injected every 6 months).
- Severe kidney problems? Avoid oral bisphosphonates. Use teriparatide or denosumab instead.
Doctors also use tools like FRAX to calculate your 10-year fracture risk. If it’s over 20%, pharmacological treatment is strongly recommended.
Monitoring and Long-Term Care
You can’t just start treatment and forget it. You need to track your progress. A bone density scan (DXA) should be done at the start of steroid therapy, then again at 12 months. If your bone density drops more than 5% in a year, your treatment plan needs to change.Also, watch for side effects. Bisphosphonates carry a small risk of atypical femur fractures and osteonecrosis of the jaw-especially after five years of use. That’s why many doctors recommend a “drug holiday” after 3-5 years if your bone density has stabilized and your fracture risk is low.
Teriparatide has a black box warning for bone cancer in rats, but no increased risk has been found in humans after 15+ years of use. The FDA still considers it safe for adults.
The Big Problem: Under-Treatment
Here’s the shocking truth: despite clear guidelines, only about 1 in 5 people on long-term steroids get their bone density checked within the first year. Less than 20% get the right medications. That’s not because doctors don’t know-it’s because the system is broken. Patients forget. Doctors get busy. Pharmacies don’t remind.One study of over 150,000 patients found that only 19.3% received any osteoporosis treatment within three months of starting steroids. That’s unacceptable. Bone loss from steroids is preventable. Fractures are not.
What’s Next?
New drugs are coming. Abaloparatide, a newer version of teriparatide, shows even better bone-building results. Researchers are now testing whether starting with teriparatide and switching to zoledronic acid gives better long-term results than using either alone. Early data suggests a 25% greater gain in bone density with this approach.But for now, the best strategy is simple: know your risk, get tested, take your calcium and vitamin D, and if you need it, take the right medication. Don’t wait for a fracture to wake you up. Steroids can save your life. But they shouldn’t steal your mobility.
How soon do steroids start affecting bone density?
Bone loss from steroids can begin within 3 to 6 months of starting treatment, especially at doses of 5 mg or more of prednisone per day. The most rapid loss happens in the first year, which is why prevention should start immediately.
Can I get enough calcium and vitamin D from food alone?
It’s very hard. You’d need about four glasses of fortified milk, three servings of fatty fish, and daily sunlight exposure to hit the recommended daily amounts. Most people on steroids need supplements to reach the target levels, especially vitamin D, which is hard to get from diet alone.
Are bisphosphonates safe for long-term use?
They’re generally safe for 3-5 years. After that, your doctor may pause treatment for a while (a “drug holiday”) if your bone density is stable and your fracture risk is low. Long-term use carries small risks like atypical femur fractures and jaw bone issues, but these are rare-about 1 in 10,000 to 1 in 100,000 users per year.
What if I can’t swallow pills or have stomach problems?
You have options. Zoledronic acid is given as a yearly IV infusion and avoids the stomach entirely. Denosumab is a twice-yearly injection. Both are effective alternatives for people who can’t tolerate oral bisphosphonates.
Do I still need to exercise if I’m on these medications?
Yes. Weight-bearing exercise like walking, stair climbing, or resistance training helps stimulate bone growth and improves balance to prevent falls. Medications slow bone loss, but exercise helps rebuild strength. Even 30 minutes a day makes a difference.
Can I stop steroids to protect my bones?
Never stop steroids without your doctor’s guidance. For many conditions, steroids are life-saving. The goal isn’t to stop them-it’s to protect your bones while you’re on them. That’s why prevention strategies are so critical.


Noah Raines
I started prednisone last year for my RA and didn't know about any of this until I fractured my wrist. My doctor never mentioned bone loss. Seriously, why isn't this standard info? I'm lucky I didn't break my spine.
Now I'm on alendronate and taking calcium like my life depends on it. Which, honestly, it kinda does.
Ruth Witte
OMG YES 💪钙 + D3 is NON-NEGOTIABLE. I was doing the bare minimum until I saw my DXA scan. Bone density dropped 8% in 6 months. Now I take my supplements with avocado toast and feel like a bone warrior 🦴✨
Katherine Rodgers
soooo... let me get this straight. you're telling me i have to take pills at 6am, stay upright for 30 mins, and still get a fracture? and this is the 'best' solution? wow. just wow. my bones are basically just a buffet for osteoclasts now. thanks, medicine.
Delaine Kiara
I've been on steroids for 11 years. I've had three vertebral fractures. I’ve tried every bisphosphonate. I’ve done the IVs. I’ve taken the injections. I’ve tracked my calcium like it’s my job. And still, my spine looks like a collapsed accordion. This isn't prevention. This is damage control. And honestly? The system is designed to fail you. Doctors are overworked. Patients are overwhelmed. And the pharmaceutical companies? They're just happy you're still taking pills. You think teriparatide is expensive? Try living with chronic pain and a 30% height loss. The real cost isn't in the prescription. It's in your dignity.
And don't even get me started on the 'drug holiday'. What happens when you go off and your bones say 'nope, we're not coming back'? You get a new fracture. Again. Because the system doesn't care about long-term outcomes. It cares about quarterly reports.
Lauren Dare
The FRAX tool is statistically valid, but in practice, it’s a glorified lottery ticket. I’ve seen patients with T-scores of -3.2 who didn’t qualify for meds because their ‘10-year risk’ was 19.8%. Meanwhile, the guy with a T-score of -1.8 got bisphosphonates because he’s 67 and ‘has risk factors’. It’s not medicine. It’s algorithmic bias wrapped in clinical jargon.
Gilbert Lacasandile
I appreciate this post so much. I’ve been on low-dose prednisone for lupus for 5 years and never knew bone loss could happen this fast. I just started calcium and D3 this week. I’m also asking my rheum about a DXA scan. I didn’t realize I was already behind. Thanks for the clarity.
Taya Rtichsheva
why do they make you take bisphosphonates on an empty stomach like its some kind of ritual? i just drink coffee and lie back down and hope for the best
Christian Landry
i took zoledronic acid last year. no pills. no waiting. just a 15-min infusion. felt weird for a day like i had the flu but honestly? worth it. my bones are holding up. my doctor said i'm one of the few who actually stuck with it. most people bail after the first infusion cause they're scared of the 'flu-like symptoms'. but it's just your body reacting. not dying. you're not dying. you're getting stronger.
Katie Harrison
I'm Canadian, and here, denosumab is covered under our provincial plan for steroid-induced osteoporosis - but only if you’ve had a prior fracture. I had to appeal. Took three months. I had to submit three letters from specialists, a copy of my DXA scan, and a notarized statement about my daily prednisone dose. They approved it. But I cried in the pharmacy line. Because I shouldn’t have had to fight to protect my bones. I should’ve been offered this from day one.
Andrea DeWinter
Exercise is the unsung hero here. I started weight training 3x a week after my diagnosis. Not to build muscle - to remind my bones they still matter. Walking, squats, resistance bands. It’s not glamorous. But my last DXA showed a 2% gain. I didn’t just stop the loss. I reversed it. You don’t need a gym. You need consistency. And maybe a friend to yell at you to show up.
Steve Sullivan
It’s funny. We treat cancer with chemotherapy that makes you vomit for weeks, and we call it bravery. But when you need to take a pill every week and stay upright for 30 minutes to save your bones? People call it ‘annoying’. We’ve normalized fragility. We’ve turned prevention into a chore. And we wonder why people break. It’s not just the steroids. It’s the culture that says, ‘Just live with it.’
George Taylor
So... let me get this straight. I have to take calcium, vitamin D, a bisphosphonate, maybe an IV, maybe an injection, do weight-bearing exercise, get scanned every year, and still, I might break a bone? And if I do, I get a 'drug holiday'? What is this, a horror movie? Who designed this system? A sadist with a medical degree?
ian septian
Calcium + D3 + exercise. That's it. Don't overcomplicate it.
Steve Sullivan
You said it, Ian. But for people who’ve already fractured? That’s not enough. You can’t just ‘do the basics’ when your spine’s collapsing. That’s like saying ‘just eat vegetables’ to someone with stage 4 cancer. Some of us need more than basics. We need weapons.