Only 42% of gout patients hit their serum urate targets within a year. Why? Because gout isn’t just about pain-it’s about controlling uric acid levels to stop crystals from forming. This is where urate targets come in: precise blood uric acid levels that prevent flares and dissolve existing crystals. Let’s break down how allopurinol and febuxostat strategies work to hit these targets.
What Are Urate Targets?
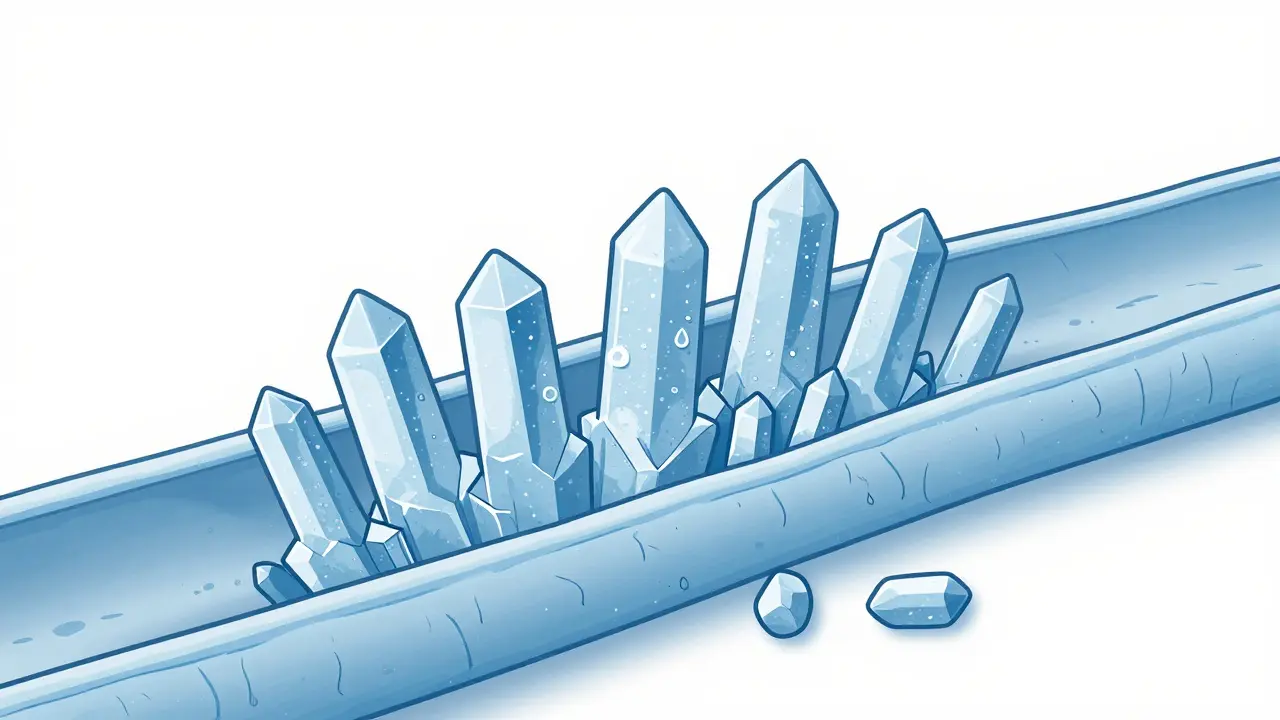
Serum urate is the amount of uric acid in your blood, measured in milligrams per deciliter (mg/dL). The goal for most gout patients is to keep it below 6 mg/dL (360 micromol/L). Why? Because above 6.8 mg/dL, uric acid turns into sharp crystals that lodge in joints, causing severe pain. For severe cases with tophi (white lumps under the skin) or frequent flares, doctors aim lower-below 5 mg/dL (300 micromol/L). This isn’t arbitrary. Studies show maintaining levels below 6 mg/dL reduces flare frequency by 74% compared to higher levels.
Think of it like a thermostat. If your blood uric acid is too high, your body keeps making crystals. Keep it below 6 mg/dL, and those crystals slowly dissolve. But going too low-below 3 mg/dL-has no extra benefit and might cause problems. All major guidelines agree: treat-to-target is non-negotiable for gout management.
Allopurinol vs Febuxostat: How They Compare
| Aspect | Allopurinol | Febuxostat |
|---|---|---|
| Mechanism | Xanthine oxidase inhibitor | Xanthine oxidase inhibitor |
| Starting dose | 100 mg/day (50 mg/day for CKD stage ≥3) | 40 mg/day |
| Max dose | 800 mg/day | 120 mg/day |
| Cost (US) | $4-$12/month (generic) | $30-$50/month |
| Best for | Most patients, especially with normal kidney function | Severe CKD or allopurinol intolerance |
| Key considerations | HLA-B*5801 testing recommended before starting | Higher cardiovascular risk in some studies |
Allopurinol has been the go-to drug for decades. It blocks uric acid production in the liver. Doctors start low-100 mg daily-and bump the dose monthly until serum urate hits target. Most people need 300-600 mg/day, but some require up to 800 mg. It’s cheap and works well for most, but 0.1-0.4% of patients develop a dangerous skin reaction called allopurinol hypersensitivity syndrome. That’s why testing for HLA-B*5801 gene variant is recommended before starting.
Febuxostat is a newer option. It also blocks uric acid production but works differently. It starts at 40 mg/day and can go up to 80 mg/day. It’s often chosen for patients with kidney disease or those who can’t tolerate allopurinol. However, it’s pricier and carries a higher risk of heart-related issues in some studies. The FDA requires a black box warning about cardiovascular risks for patients with existing heart problems.
Guideline Differences: ACR, NICE, EULAR
Doctors follow different guidelines, but they all agree on core principles. The 2020 American College of Rheumatology (ACR) Guideline strongly recommends allopurinol as first-line treatment regardless of kidney function. They also say ULT (urate-lowering therapy) is mandatory for everyone with tophi or frequent flares.
The NICE Guideline NG219 (UK) takes a more flexible approach. It says either allopurinol or febuxostat can be first-line, depending on patient preferences and comorbidities. NICE also emphasizes patient education-many don’t realize gout requires lifelong management.
EULAR 2023 recommendations (European) align closely with ACR but stress allopurinol for patients with normal kidney function. They also introduce "treat-to-dissolve" for severe cases: keep serum urate below 5 mg/dL until tophi disappear, confirmed by imaging.
One key difference? Asymptomatic hyperuricemia (high uric acid without gout symptoms). ACR says no treatment needed, while NICE doesn’t address it. This shows why personalized care matters-what works for one patient might not for another.
Real-World Challenges in Gout Management
Even with clear guidelines, hitting urate targets is tough. In New Zealand, Māori and Pacific populations get urate-lowering drugs more often but achieve targets 23% less frequently than European patients. Why? Systemic barriers like limited healthcare access and cultural mistrust play a role.
Doctors often miss the mark too. Only 54% of patients get monthly serum urate tests during dose adjustments, even though monthly monitoring boosts target achievement by 31%. Many patients stop taking meds because they fear side effects. For example, 68% of dose escalation failures stem from worries about allopurinol reactions. Some experience "flare paradox"-initially more pain when starting treatment-without understanding it’s temporary.
And it’s not just about pills. A 2023 study found 37% of guideline recommendations rely on low-quality evidence due to limited long-term trials. That’s why doctors must balance science with real-world experience.

Recent Advances in Urate Target Therapy
Genetics is changing the game. The GOUT-PRO study (2024) tested genotype-guided dosing. By checking ABCG2 and SLC22A12 gene variants, doctors could adjust allopurinol doses more precisely. Results? Target achievement jumped from 61% to 83% in six months. This could soon become standard practice.
New drugs are also emerging. Verinurad, a novel uricosuric, helps the kidneys excrete more uric acid. Early trials show it achieves targets with fewer dose escalations. Meanwhile, the ULTRA-GOUT trial (NCT04923178) is comparing fixed-dose versus treat-to-target strategies-results expected late 2025.
Value-based care models are making progress too. Kaiser Permanente’s 2023 initiative used protocol-driven management, hitting targets in 67% of patients versus 39% in standard care. This proves structured approaches work when implemented well.
What Patients Can Do to Reach Urate Targets
Getting to your urate target takes teamwork. First, ask for regular serum urate tests. Don’t wait for pain-monitor levels monthly during dose adjustments. Second, stick to your meds. Skipping doses is the #1 reason treatment fails. Third, discuss side effects openly. Many fears are unfounded; for example, allopurinol reactions are rare with proper testing.
Also, track your diet. While food isn’t the main cause of gout, some triggers like beer and red meat can worsen flares. Stay hydrated and maintain a healthy weight. And remember: gout management is a marathon, not a sprint. It takes 6-12 months to dissolve crystals fully. Be patient, stay consistent, and partner with your doctor.
Why do I need to keep my serum urate below 6 mg/dL if I’m not in pain?
Pain isn’t the only sign of gout. Even when you feel fine, high uric acid keeps forming crystals in your joints. These crystals cause long-term damage and set the stage for future flares. Keeping levels below 6 mg/dL stops new crystals from forming and slowly dissolves existing ones. Studies show this reduces flare frequency by 74% compared to higher levels. It’s like cleaning up a mess before it gets worse.
Is allopurinol safe if I have kidney disease?
Yes, but dosing matters. For chronic kidney disease (CKD) stage 3 or higher, doctors start allopurinol at 50 mg/day instead of 100 mg. They monitor serum urate closely and adjust slowly. Allopurinol is still preferred over febuxostat for most CKD patients because it’s safer long-term. However, if you have severe CKD (stage 4-5), your doctor might choose febuxostat or another option. Always discuss kidney function with your rheumatologist before starting treatment.
What if I experience a flare when starting urate-lowering therapy?
This is called "flare paradox" and is common. When uric acid drops quickly, crystals shift and trigger inflammation. The good news? It’s temporary. Your doctor will usually prescribe low-dose colchicine or NSAIDs for 3-6 months to prevent flares during treatment. Never stop your urate-lowering drug-this is the time to stick with it. Flares typically subside within 3-6 months as crystals dissolve. If they persist, your dose may need adjustment.
How often should I get my serum urate tested?
During dose adjustments, test monthly until you hit target. Once stable, test every 3-6 months. The ACR recommends two consecutive measurements below 6 mg/dL at least 30 days apart before considering treatment goals met. Skipping tests is risky-many patients think they’re on track when they’re not. For example, a 2023 Medicare study found only 54% of patients got monthly tests during titration. Don’t be one of them-ask for regular blood work.
Can I stop taking allopurinol once my urate targets are hit?
No. Gout is a chronic condition requiring lifelong management. Stopping treatment lets uric acid rise again, causing crystals to reform. Studies show 90% of patients relapse within a year of stopping urate-lowering therapy. Even if you feel fine, keep taking your meds. Your doctor might adjust the dose over time, but discontinuation isn’t an option. Think of it like high blood pressure medication-you don’t stop after feeling better.



Kate Gile
Sticking to your urate targets is crucial even when you're not in pain.
It's the only way to stop crystals from forming and dissolve existing ones.
Consistency is key.
anjar maike
I've been on allopurinol for years and it works great just need to stay hydrated and get regular blood tests 🌟
Arjun Paul
Most patients don't realize that allopurinol dosing must be adjusted monthly. Many stop too soon causing relapses.
Nancy Maneely
The FDA should ban febuxostat its way too dangerous. Only in America do we have safe options. All other countries are clueless.
Phoebe Norman
Urate targets are critical for preventing crystal formation Serum uric acid levels must remain below six mg/dL Long-term management requires strict adherence No exceptions
Albert Lua
In India we often use turmeric for inflammation but it doesn't replace urate-lowering meds. Still diet matters. Stay active and manage weight.
Carl Crista
Big Pharma controls the guidelines. They want you on meds forever. Allopurinol is safe but they hide the risks. Always question authority.
Joyce cuypers
Don't worry you can do this! Just take your meds and stay hydrated. Your doctor is there to help. Keep going!
Georgeana Chantie
Only US doctors know how to treat gout right. Other countries are behind. 🇺🇸
Carol Woulfe
The current guidelines lack rigorous scientific validation. They are based on flawed studies funded by pharmaceutical companies. True management requires personalized care.
Kieran Griffiths
Consistency is key. Many patients stop treatment too early. Keep taking your meds even when you feel better. Your doctor can adjust doses as needed.
Lisa Scott
The studies are all biased. Pharma funds everything. Urate targets are a scam to sell drugs. Don't trust the system.
Tehya Wilson
The evidence base for urate targets is insufficient. More research is needed before implementing widespread protocols.
Brendan Ferguson
Both allopurinol and febuxostat have their place. It's about finding the right fit for each patient. Always discuss options with your doctor.
jan civil
Staying hydrated is key for managing uric acid levels.