For decades, managing diabetes meant pricking your finger multiple times a day-sometimes up to eight or more-to check blood sugar. You’d scribble numbers in a notebook, guess at insulin doses, and hope for the best. Today, that’s changing. CGMs are no longer a luxury for Type 1 diabetes patients. They’re now a standard tool recommended for nearly everyone on insulin, including older adults, pregnant people, and kids. And it’s not just about the device. Smart pens, apps, and predictive algorithms are turning diabetes from a daily chore into a manageable, even predictable, part of life.
How CGMs Changed Everything
Before continuous glucose monitors (CGMs), your only real-time data came from fingersticks. HbA1c tests gave you a three-month average, but they couldn’t tell you if your sugar crashed at 3 a.m. or spiked after lunch. CGMs changed that. They measure glucose in your interstitial fluid every five minutes, 24/7. That means you see trends, not just numbers.
The latest models-like the Abbott FreeStyle Libre 3, Dexcom G7, and Medtronic Guardian 4-have accuracy levels that rival lab tests. The Libre 3 has a MARD score of 8.1%, meaning its readings are, on average, just 8.1% off from a blood test. The Glucotrack implantable sensor, still in trials, is hitting 7.7%. That’s better than most fingerstick meters.
But accuracy isn’t the only win. CGMs show you time in range-how long your glucose stays between 70 and 180 mg/dL. Studies show that for every 10% increase in time in range, your risk of eye, kidney, and nerve damage drops by 64%. Users of CGMs spend an average of 3.2 more hours per day in range than those still using fingersticks. That’s not just a number-it’s fewer hospital visits, fewer panic moments, and better sleep.
Who Should Use a CGM?
The American Diabetes Association’s 2025 guidelines say CGMs should be used by:
- Everyone with Type 1 diabetes
- People with Type 2 diabetes who take insulin
- Pregnant women with diabetes
- Older adults at risk for low blood sugar
- Children from the moment they’re diagnosed
That’s a huge shift. Just five years ago, CGMs were mostly for Type 1 patients. Now, if you’re on insulin, your doctor should be talking to you about it. Even people not on insulin are starting to use them-especially those with prediabetes or who are trying GLP-1 medications like Ozempic. Why? Because those drugs can cause unpredictable drops in blood sugar. CGMs help catch them before they become dangerous.
Smart Pens: The Missing Link
CGMs tell you your glucose level. But they don’t tell you how much insulin you took-or when. That’s where smart insulin pens come in. The InPen by Medtronic connects to your CGM and remembers every dose you give. It can even suggest how much insulin you should take based on your current glucose, recent meals, and insulin on board.
Yet adoption is low. Only 15% of insulin users use smart pens, according to 2025 data from ADCES. Why? Cost. Many aren’t covered by insurance. Others find them bulky or don’t realize they can sync with apps like mySugr or One Drop. But for people who forget doses or overcorrect, they’re a game-changer. One user on Reddit said his A1c dropped from 9.8% to 7.1% in six months after using InPen with his Dexcom. He didn’t change his diet. He just stopped guessing.
Apps That Actually Work
There are hundreds of diabetes apps. Most are cluttered, slow, or don’t talk to your CGM. But the good ones? They’re powerful. mySugr, One Drop, and Glucose Buddy sync with Dexcom, Libre, and Medtronic systems. They log meals, exercise, stress, and insulin. They generate reports for your doctor. Some even use AI to predict your next spike or drop.
But here’s the catch: only 43% of third-party apps work with all major CGMs. If you buy a Libre 3, make sure your app supports it. Otherwise, you’re stuck manually entering data-defeating the whole point.
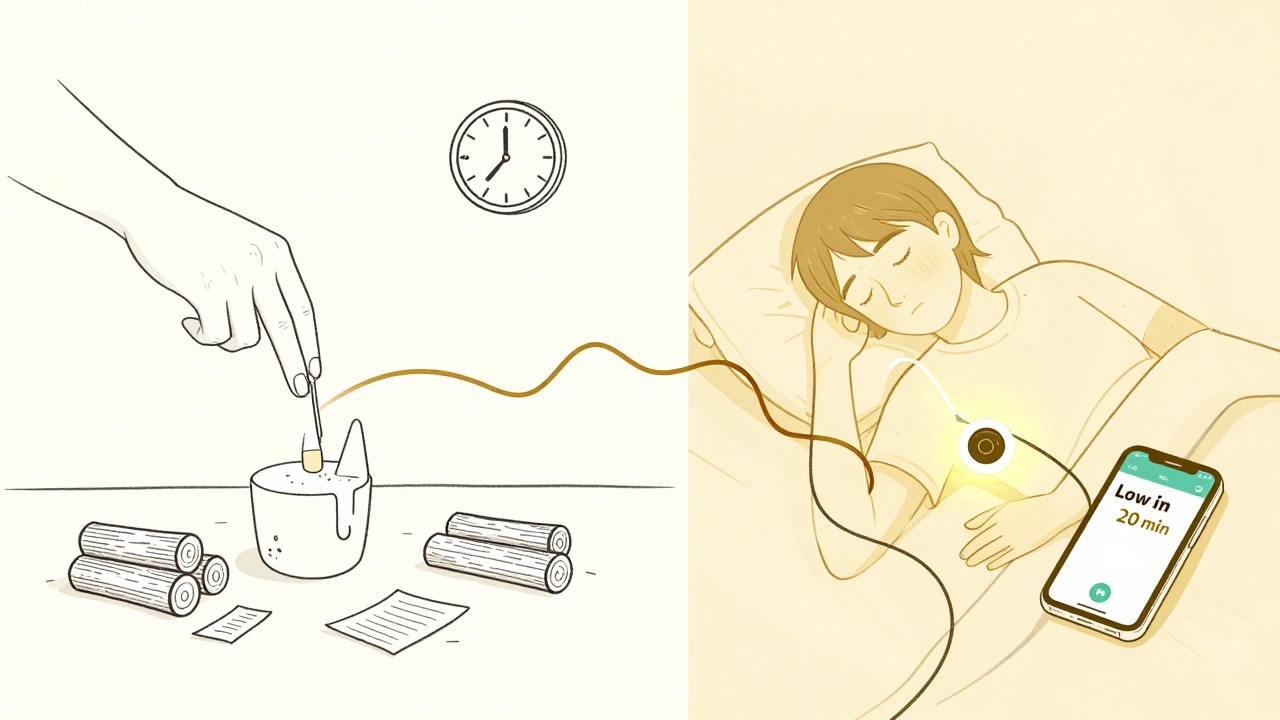
One standout feature? Nighttime alerts. A 2025 survey of 1,243 CGM users on Reddit found that 78% slept better because their app woke them up before a low. Another 63% said they felt less anxious about their sugar levels. That’s not just convenience-it’s mental health.
Implantable CGMs: The Next Leap
Right now, CGMs sit on your skin. They stick on with adhesive, can fall off during exercise or swimming, and need replacing every 10 to 14 days. Glucotrack is changing that. It’s a tiny sensor-about the size of three nickels-implanted under the skin by a doctor. It measures glucose directly from blood, not interstitial fluid. That means no lag. No delay. Real-time readings.
It’s designed to last up to three years. No external transmitter. No charging. Just a small reader app on your phone. The company expects U.S. approval in 2028. If it works as claimed, it could prevent 12,000 to 15,000 severe low-blood-sugar events each year in the U.S. alone.
And it’s not alone. Senseonics’ Eversense E3 lasts six months. Biolinq is working on sensors that track muscle loss in people taking GLP-1 drugs. The future isn’t just about monitoring-it’s about understanding how your body responds to everything you do.

The Hidden Problems
None of this is perfect.
Cost is the biggest barrier. Uninsured patients pay around $300 a month for sensors. Even with insurance, 37% report prior authorization denials. Medicare expanded coverage in 2024, and usage jumped from 2.1% to 28.7% among seniors with Type 2 diabetes. But Medicaid and private insurers still lag.
Data security is another issue. A 2025 JAMA study found that 63% of CGM systems had vulnerabilities that could let someone manipulate glucose readings. Imagine a hacker changing your numbers to make you think you’re low-then giving you too much insulin. It’s rare, but it’s possible.
And then there’s alert fatigue. Sixty-eight percent of new users get overwhelmed by beeping alarms. The ADA now recommends personalized alerts. A night-shift worker needs different settings than a teacher. A teenager needs different alerts than a grandparent. Customization isn’t optional-it’s essential.
Getting Started
If you’re considering a CGM, here’s what works:
- Ask your doctor for a prescription. Even if you’re on oral meds, if you’ve had lows, ask.
- Check insurance coverage. Medicare covers CGMs for Type 2 patients on insulin. Some private insurers do too.
- Choose a system that works with your phone and preferred app. Libre 3 works with Apple Health and Google Fit. Dexcom works with most third-party apps.
- Sign up for training. 78% of people who stick with CGMs get formal education. Don’t skip it.
- Set your alerts. Start with conservative low/high alarms. Adjust after a week.
It takes 2 to 4 weeks to feel comfortable. But once you do? You’ll wonder how you ever managed without it.
What’s Next?
The next big thing isn’t just better sensors. It’s prediction. Dexcom and EarlySense are rolling out AI that forecasts glucose changes up to 30 minutes ahead. That means your phone could warn you: "Your sugar will drop in 20 minutes. Eat 15g of carbs."
Vaxess Technologies is testing a needle-free patch for semaglutide. If it works, you won’t need to inject at all. And automated insulin delivery systems-like Tandem’s Control-IQ-are now combining CGMs with insulin pumps and even GLP-1 drugs. One study showed patients lost 18 pounds in six months without more lows.
The goal isn’t just control. It’s freedom. Freedom from constant checking. Freedom from fear. Freedom to live without diabetes running your life.
Are CGMs covered by insurance?
Yes, for many people. Medicare covers CGMs for Type 2 diabetes patients on insulin. Most private insurers cover them for Type 1 diabetes. Coverage for Type 2 patients not on insulin varies. Always check with your provider and ask about prior authorization. Out-of-pocket costs can range from $0 to $300 per month depending on your plan.
Can I use a CGM if I don’t take insulin?
Absolutely. While CGMs were originally for insulin users, they’re now recommended for anyone with Type 2 diabetes, prediabetes, or those on GLP-1 medications like Ozempic or Wegovy. These drugs can cause unexpected drops in blood sugar. A CGM helps you catch them before they become dangerous. Even non-diabetic people use them to track how food and stress affect their glucose.
Do smart pens really help with insulin dosing?
Yes-if you use them correctly. Smart pens like InPen track every dose, calculate insulin on board, and suggest corrections based on your CGM data. They reduce dosing errors and help prevent highs and lows. But they’re only useful if they’re synced with your CGM and app. Many people buy them but don’t connect them, so they miss the benefits.
How long do CGM sensors last?
It depends on the brand. Dexcom G7 lasts 10 days. Abbott FreeStyle Libre 3 lasts 14 days. Medtronic Guardian 4 sensors last 7 days. The Eversense E3 implant lasts 6 months. Glucotrack, still in development, aims for up to three years. Replacement frequency affects cost, so factor that in when choosing a system.
Why do CGMs sometimes feel inaccurate?
CGMs measure glucose in interstitial fluid, not blood. There’s a natural 5-15 minute lag, especially after eating, exercising, or taking insulin. That’s why your CGM might show 70 while your fingerstick says 90. It’s not broken-it’s delayed. Implantable sensors like Glucotrack aim to fix this by measuring directly from blood. For now, calibrate your device after meals or when you feel symptoms, and trust trends over single numbers.
Can CGMs help with weight loss?
Indirectly, yes. When you see how carbs, stress, or sleep affect your glucose, you naturally make better choices. One study found that combining CGMs with semaglutide helped Type 1 patients lose 18 pounds in six months-without increasing low blood sugar. CGMs don’t cause weight loss, but they give you the data to make decisions that support it.





Kidar Saleh
CGMs are the single biggest leap in diabetes care since insulin itself. The fact that we can now see trends instead of snapshots changes everything-sleep, anxiety, even relationships. I’ve watched my sister go from terrified to empowered, and it’s all because she stopped guessing.
Vincent Soldja
Cost is still a joke.
Chloe Madison
Just wanted to say-this is exactly why I started teaching diabetes tech workshops at my clinic. People think it’s complicated, but once they see how the data links to their real life-meals, sleep, stress-they get it. One patient told me she finally stopped crying before bed because her CGM warned her about a drop. That’s not tech. That’s peace.
Katherine Gianelli
My grandma got her Libre 3 last year and now she texts me every morning with her time in range percentage like it’s a game. She used to hide her lows because she was scared. Now she laughs when the alarm goes off at 3 a.m. and says, ‘Oh honey, I’m just having a little dance with my glucose.’ It’s not just medical-it’s emotional liberation.
parth pandya
smart pens r great but i got a dexpcom and myinsulin app just dont sync right like half the time and i end up typing it in anyway lol
Albert Essel
There’s a quiet revolution happening here. We’re not just managing a disease-we’re redefining autonomy. The data isn’t just numbers; it’s a conversation between the body and the individual. And that conversation, when properly facilitated, restores dignity.
Joykrishna Banerjee
Let’s be real-CGMs are just a Band-Aid on a broken healthcare system. You’re telling me a 70-year-old on Medicaid is supposed to afford $300/month sensors while Big Pharma profits? This isn’t innovation-it’s exploitation dressed in beta-glucose.
Jim Schultz
Oh wow, you’re telling me that after 30 years of fingersticks, we finally have tech that doesn’t suck? Shocking. I mean, sure, the Libre 3 has an 8.1% MARD-but did you account for the 14% variance in interstitial fluid lag? And don’t get me started on the fact that 63% of CGM systems have exploitable API vulnerabilities-because apparently, we’re all just supposed to trust the cloud with our glucose levels? The ADA recommends this like it’s gospel, but the real question is: who’s auditing the auditors? And why is nobody talking about the fact that 43% of apps don’t support Libre 3? This isn’t progress-it’s a marketing brochure with a pulse oximeter.
Gavin Boyne
So we’ve turned a chronic condition into a Silicon Valley dashboard. Brilliant. Next up: AI that tells you when to feel guilty about eating bread. At this point, I’m just waiting for the subscription model for ‘emotional glucose support.’ $9.99/month to stop crying over a 120 reading. Truly, we’ve arrived.
Myson Jones
My doctor didn’t mention CGMs until I asked. Then she handed me a pamphlet. No demo. No trial. No follow-up. I bought one anyway. It took me three weeks to stop treating every beep like a crisis. Now I use it like a compass-not a dictator. The tech works. The system? Still broken.
Makenzie Keely
Can we talk about how the ADA guidelines now include children from diagnosis? That’s not just clinical-it’s cultural. For the first time, a kid with Type 1 doesn’t have to grow up feeling like a walking lab rat. They get to live. They get to play. They get to forget, sometimes, that they have diabetes. That’s not a device. That’s a promise kept.
Francine Phillips
my phone beeps too much
Charles Moore
Jim, your critique is valid-but what you’re calling exploitation, others are calling empowerment. The real failure isn’t the tech. It’s that we still treat access as a privilege instead of a right. Maybe the answer isn’t to reject CGMs, but to fight harder for universal coverage. The tool is good. The system just needs a heart.