Medical Term Translator
Your medical records often contain terms like DM or HTN that doctors use for efficiency. This tool translates those terms into language you can understand.
Try "DM," "E11.9," or "HTN" for examples from the article
Enter a medical term to see its patient-friendly translation
Why Your Doctor’s Notes Don’t Match How You Feel
You walk out of the appointment with a piece of paper that says "Type 2 Diabetes Mellitus, E11.9". You nod, smile, and thank your doctor. But inside, you’re thinking: "What does that even mean? I just feel tired all the time and I’m always thirsty."
This gap isn’t just confusing-it’s dangerous. Studies show that 68% of patients misunderstand common medical terms like "hypertension" or "colitis." And when patients don’t understand what’s written about them, they skip meds, miss follow-ups, or worse-blame themselves.
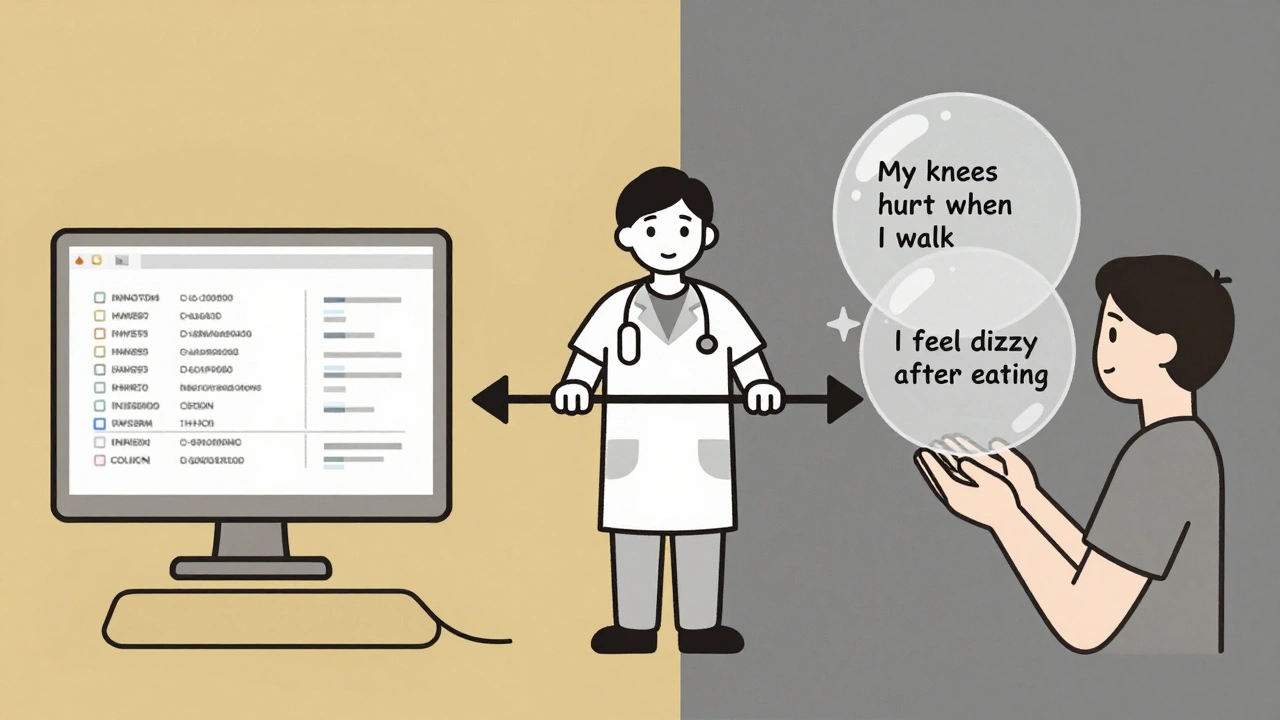
Doctors Use Codes. Patients Use Stories
Healthcare providers don’t write notes for patients. They write them for billing, insurance, and legal records. That’s why you see codes like ICD-10 and CPT in your chart. There are over 70,000 diagnosis codes and 10,000+ procedure codes. These aren’t meant to be read by you. They’re meant to be read by computers and billing departments.
But you? You don’t care about codes. You care about what’s happening in your body. You say: "My knees ache when I walk," not "osteoarthritis of the bilateral knees." You say: "I feel like I’m drowning after eating," not "gastroesophageal reflux disease."
This isn’t a coincidence. It’s a system designed for efficiency, not understanding. The same EHRs that power 50% of U.S. hospitals-like Epic and Cerner-were built to speed up paperwork, not improve communication.
What Happens When Labels Don’t Connect
One patient on PatientsLikeMe wrote: "My doctor wrote 'poorly controlled DM' in my chart. I thought it meant I was a bad person, not that my blood sugar was high."
That’s not an outlier. A 2022 survey found 57% of patients felt confused by the terms in their medical records. And 32% of them avoided going back to the doctor because of it.
Doctors aren’t trying to confuse you. But they’re trained to speak in shorthand. "DM" for diabetes. "HTN" for high blood pressure. "COPD" for lung disease. To them, it’s faster. To you, it’s a foreign language.
And the consequences? A 2021 study found that language mismatches contribute to 30-40% of medication errors. That’s not a small number. That’s thousands of people taking the wrong dose-or the wrong pill-because they didn’t understand what was written.
Who’s Trying to Fix This?
Some people are stepping in. Health Information Management (HIM) professionals-certified coders and data specialists-are the bridge between these two worlds. They’re trained to translate clinical jargon into something that can be understood by both computers and humans.
They don’t just code your visit into ICD-10. They make sure your story isn’t lost in the process. They ensure your records are complete, accurate, and protected under HIPAA. And they’re the ones pushing for change.
Organizations like Kaiser Permanente and Mayo Clinic have started using "plain language" templates in their EHRs. Instead of "myocardial infarction," the patient-facing version says "heart attack." Instead of "hyperlipidemia," it says "high cholesterol." In Mayo’s pilot, patient confusion dropped by 38%.
Open Notes Are Changing the Game
Before 2021, most patients couldn’t even see what their doctors wrote about them. Then the 21st Century Cures Act forced hospitals to give you access to your clinical notes-no filters, no edits.
Now, 89% of U.S. hospitals let you read your chart online. That’s up from just 15% in 2010. And it’s forcing a shift.
Doctors can’t just write "non-compliant" anymore. They know you’ll read it. So they’re changing how they talk. Some now write: "You mentioned you’ve been having trouble taking your pills because of the side effects. Let’s talk about options."
This is called the OpenNotes movement. It’s grown to include over 55 million patients across 350+ health systems. And early results are clear: patients who read their notes understand their conditions better. They take their meds more often. And they have fewer arguments with their doctors.

What’s Next? AI That Speaks Your Language
The next big step? Machines learning to translate doctor-speak into human-speak.
Google’s Med-PaLM 2, released in 2023, can convert clinical notes into plain language with 72.3% accuracy. That’s good-but not good enough. For medical use, we need 95% accuracy. We’re not there yet.
But the direction is clear. By 2027, experts predict 60% of EHR systems will have real-time translation built in. Imagine typing your symptoms into a portal, and the system automatically updates your chart with both the medical term and your own words side by side.
The World Health Organization’s ICD-11, launched in 2022, already includes patient-friendly descriptions alongside clinical codes. That’s the first time a global medical classification system has tried to speak to both sides at once.
What You Can Do Right Now
- Ask your doctor: "Can you explain that in simpler terms?" No shame in it. Most doctors expect it now.
- Use the "teach-back" method: After they explain something, say, "So if I understand right, you’re saying..." Then repeat it back. Studies show this cuts miscommunication by 45%.
- Read your notes. If you see something confusing, write it down and ask next time. You have a right to understand what’s written about you.
- Ask if your clinic uses plain language in patient portals. If not, suggest it. Patient demand drives change.
Why This Matters More Than You Think
This isn’t just about words. It’s about power. For decades, medical knowledge was locked behind jargon. The patient was the receiver. The doctor was the expert. That’s changing.
When you understand your own health data, you become part of the team. You’re not just a case number. You’re a person with a story. And your story matters just as much as the code.
Healthcare is finally waking up to that. But it’s not happening fast enough. And until it does, you’ll keep walking out of appointments feeling lost-even when you’re told you’re "doing fine."
Why do doctors use codes instead of plain language in medical records?
Doctors use codes like ICD-10 and CPT because they’re required for billing, insurance claims, and legal documentation. These standardized codes help hospitals get paid and ensure consistency across systems. But they weren’t designed for patients. The same codes that help a billing clerk process a claim can confuse someone trying to understand their own diagnosis.
Can I ask my doctor to write my chart in plain language?
Yes, and more doctors are doing it now. Since the 21st Century Cures Act required patients to see their notes, many clinics have started using plain language templates. You can ask your provider to explain terms in simple words and even request that they use those words in your chart. Many are open to it-especially if you say you want to understand your care better.
What’s the difference between ICD-10 and patient-friendly labels?
ICD-10 uses technical, standardized codes like "E11.9" for Type 2 Diabetes. Patient-friendly labels use everyday words like "high blood sugar" or "diabetes." The code helps with billing and data tracking. The plain language helps you understand your condition. New systems like ICD-11 now include both side by side.
How does reading my medical notes help me?
Reading your notes reduces confusion, improves medication adherence, and helps you spot errors. Studies show patients who read their notes understand their diagnoses better and are 19% more likely to take their medicines as prescribed. It also builds trust-you see what your doctor actually wrote, not what you imagine they wrote.
Are there tools that translate medical jargon into simple language?
Yes. Some hospitals use plain-language templates in their patient portals. Tools like Google’s Med-PaLM 2 can automatically convert clinical notes into everyday language, though they’re still being tested for accuracy. The OpenNotes movement and new EHR updates are making these tools more common. You can also ask your clinic if they offer a simplified version of your records.






Charlotte Collins
The way medical records are written feels like being handed a cryptic poem after a heart attack. You’re told you’re ‘stable’ while your body screams for help. I once saw ‘non-compliant’ next to my name because I couldn’t afford the meds. No one asked why. Just labeled me. That’s not medicine. That’s punishment wrapped in bureaucracy.
ariel nicholas
This is why America's healthcare system is a joke. You want plain language? Fine. But then who's going to pay for it? Insurance companies need codes-because they're not paying for your feelings, they're paying for a procedure. Stop blaming doctors for following the rules. Blame the system that forces them to be code-wielding automatons. Also, 'E11.9' isn't confusing-it's precise. Your feelings are not data.
Lauryn Smith
I used to dread doctor visits until I started reading my notes. One time I saw 'mild anxiety' and thought I was losing my mind. Then I realized-oh, that's just what they call stress that won't go away. I started asking for plain language. My doctor laughed, then wrote 'you're overwhelmed and tired' next to 'GAD.' I cried. It felt like someone finally saw me.
Bonnie Youn
YES. This is the change we need. Stop hiding behind jargon. I had a friend who skipped her insulin because she thought 'DM' meant 'diabetic monster' and felt guilty. That's not her fault. That's the system's failure. We can fix this. Ask your clinic for plain-language summaries. Share this post. Demand better. You're not being difficult-you're being human.
Edward Hyde
Let’s be real-doctors are lazy. They copy-paste the same note for every patient. 'HTN' 'DM' 'COPD'-it’s like they’re texting in 2008. I once got a note that said 'patient appears disinterested.' I was exhausted from working two jobs and raising a kid alone. They didn’t ask. They just labeled me. Now I bring a printed list of symptoms. They hate it. Good.
elizabeth muzichuk
This is how they control us. Plain language? Open notes? It’s all a trap. They’re giving you just enough information to make you feel empowered-so you don’t demand real change. Meanwhile, the same EHRs that show you 'high cholesterol' are still selling your data to pharma. Don’t be fooled. This isn’t transparency. It’s distraction.
Karandeep Singh
u r right but also doctors r overworked. they have 10 mins per patient. they use codes because its faster. not to confuse u. just say it in simple words next time. problem solved
Mary Ngo
It is not merely a linguistic disparity-it is an epistemological hegemony. The medical-industrial complex has codified the body into a transactional ontology, stripping phenomenological experience of its ontological weight. The ICD-10 code is not a symbol-it is a silencing mechanism. To demand plain language is to demand the dissolution of institutional power. And yet, the OpenNotes movement, while well-intentioned, remains a neoliberal co-optation: it gives the illusion of agency while preserving the underlying structure of control.