Transplant Rejection: What It Is, How It Happens, and How to Prevent It
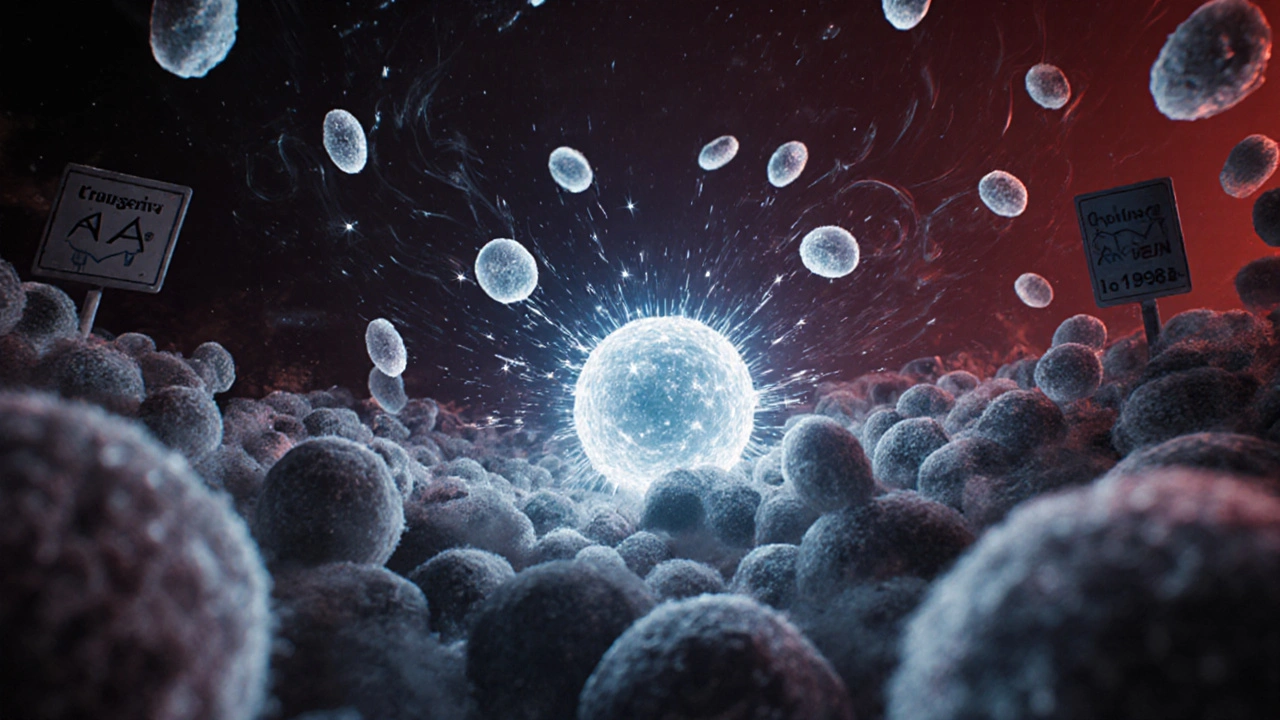
When your body receives a new organ, it doesn’t always see it as a gift. Sometimes, it sees it as an invader. This is called transplant rejection, the immune system’s attack on a transplanted organ because it recognizes it as foreign. Also known as graft rejection, it’s one of the biggest threats to the long-term success of any organ transplant. Whether it’s a kidney, liver, heart, or lung, your immune system is designed to fight off anything that doesn’t belong — and a donated organ, no matter how well-matched, still triggers that response.
That’s where immunosuppressants, medications that weaken the immune system to prevent it from attacking the transplanted organ come in. These aren’t optional. Skipping a dose, running out of pills, or ignoring side effects can lead to acute rejection — sometimes within weeks. Chronic rejection, which builds slowly over years, is harder to detect but just as dangerous. It’s not just about taking pills. It’s about regular blood tests, monitoring for fever or swelling, and knowing when something feels off. Many people think rejection means sudden failure, but often it’s a quiet process. Fatigue, mild pain, or unexplained weight gain can be early signs.
Managing transplant care, the ongoing medical and lifestyle routine after receiving a transplanted organ isn’t just about drugs. It’s about avoiding infections that can trigger immune flare-ups, staying on top of vaccinations (without live vaccines), and understanding how other medications — even over-the-counter ones — can interfere with your immunosuppressants. A simple ibuprofen or herbal supplement could throw your whole system off balance. Your care team will guide you, but you’re the one who has to remember the schedule, track symptoms, and speak up when something doesn’t feel right.
There’s no one-size-fits-all plan. A kidney transplant patient’s risks look different from someone with a heart transplant. Some people need stronger drugs. Others can reduce doses over time. But everyone shares the same goal: keep the organ working and stay alive. That’s why the posts below cover real-world stories and science-backed advice — from spotting early rejection signs to handling drug interactions, managing side effects like high blood pressure or diabetes from immunosuppressants, and what to do when you feel overwhelmed. You’re not alone in this. These are the tools, warnings, and strategies that actually help people live longer, healthier lives after a transplant.