Chronic pain affects more than 50 million adults in the U.S. And for many, opioids aren’t a sustainable solution. That’s why so many people are turning to cannabinoids-CBD, THC, CBG-to manage their pain. But does it actually work? And if it does, how much should you take without risking side effects or wasting your money?
What Are Cannabinoids, and How Do They Relate to Pain?
Cannabinoids are natural compounds found in the cannabis plant. The most studied ones for pain are tetrahydrocannabinol (THC), cannabidiol (CBD), cannabigerol (CBG), and cannabinol (CBN). They work by interacting with your body’s endocannabinoid system, which helps regulate pain, inflammation, mood, and sleep. Unlike opioids that block pain signals in the brain, cannabinoids seem to calm the nervous system at the source. A January 2025 study from Yale School of Medicine found that CBD, CBG, and CBN all reduced activity in a key protein involved in peripheral nerve pain. CBG stood out-it showed the strongest effect in lab tests. That’s important because CBG doesn’t cause a high, making it a potential candidate for pain relief without psychoactive side effects. But here’s the catch: most of what you see on store shelves isn’t what’s used in these studies. The Yale research used pure, pharmaceutical-grade compounds. The CBD oil you buy online? It might not even contain what’s on the label.The Evidence Is Mixed-And Often Contradictory
You’ll find conflicting claims everywhere. One study says cannabinoids work. Another says they’re no better than placebo. Why? The Journal of Pain published a 2023 review of 16 high-quality clinical trials using pharmaceutical-grade CBD. Fifteen of them found no significant pain relief compared to placebo. That’s not a small sample-it’s a solid body of evidence. Meanwhile, a 2015 JAMA meta-analysis concluded there’s moderate-quality evidence supporting cannabinoids for chronic pain, especially neuropathic pain. The difference? The JAMA study included products with THC. The 2023 study looked at CBD alone. Harvard Medical School put it bluntly: “There is currently no high-quality research study that supports the use of CBD alone for the treatment of pain.” The FDA has only approved CBD for two rare forms of epilepsy-not for any type of pain. But then there’s Sativex, a 1:1 THC:CBD spray approved by Health Canada for multiple sclerosis pain and cancer-related pain. Patients using it reported better pain control and lower opioid use. That’s not anecdotal-it’s FDA-regulated, double-blind trial data. So what’s the real story? CBD by itself? Probably not effective for most pain. But THC-containing products, especially in controlled ratios, show real promise-especially for nerve pain.Who Benefits the Most? Neuropathic Pain
Not all pain is the same. Osteoarthritis? Fibromyalgia? Back pain? The evidence doesn’t treat them equally. The CDC acknowledges that cannabis may help with neuropathic pain-the kind caused by damaged nerves. Think diabetic neuropathy, shingles pain, or chemotherapy-induced nerve pain. In these cases, cannabinoids appear to reduce burning, tingling, and shooting sensations better than they do for dull, aching pain. Why? Nerve pain involves overactive signaling in the peripheral nervous system. Cannabinoids, especially THC and CBG, seem to quiet that noise. A 2023 Sage Publications review found that medical cannabis improved both pain severity and quality of life for patients with neuropathic conditions. For other types-like muscle pain or joint inflammation-the data is thin. Some people swear by CBD gummies for arthritis. Others report zero change. The difference? Placebo effect, product quality, or individual biology. Reddit threads from chronic pain communities reflect this split. One user said CBD reduced fibromyalgia pain by 30%. Another spent $400 on gummies and felt nothing. The same product. Two completely different outcomes.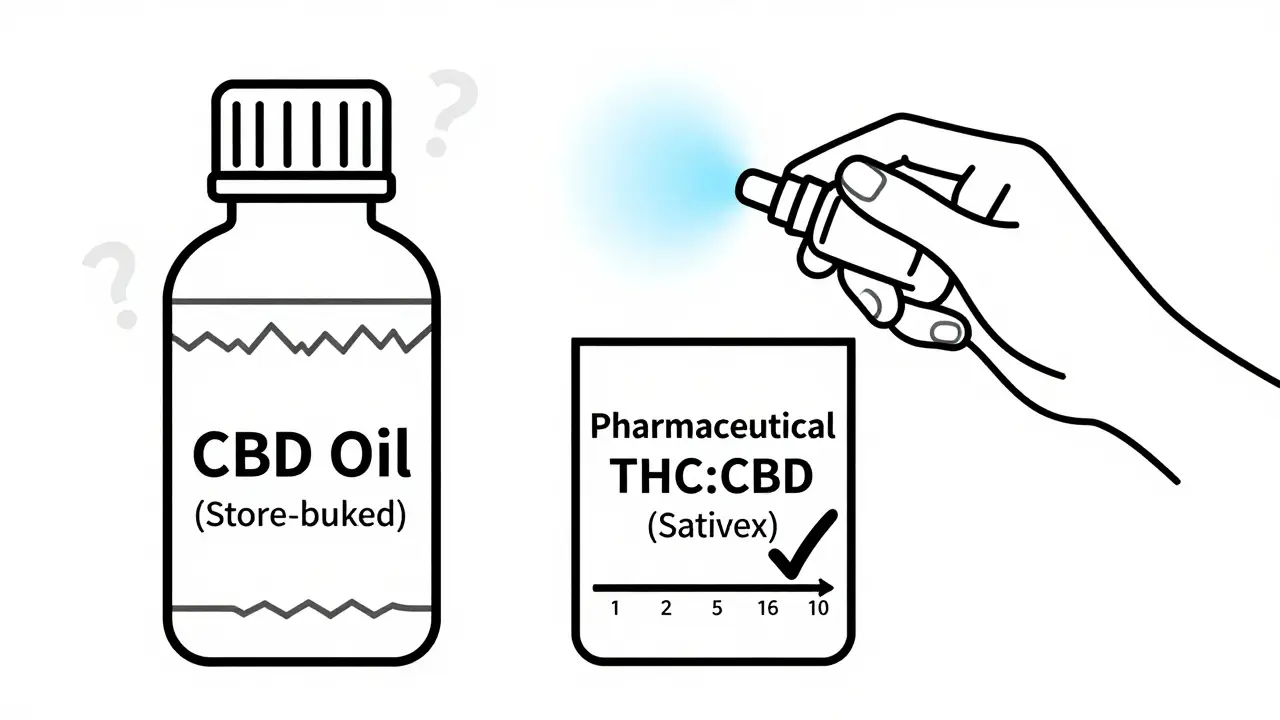
Dosing: No Standard Rules-But Here’s What Clinicians Recommend
There’s no official dosing guideline for cannabinoids and pain. That’s because the FDA hasn’t approved any for this use. But pain clinics and doctors who prescribe medical cannabis have developed practical starting points. For THC-dominant products (like tinctures or capsules):- Start with 2.5 mg THC
- Wait 2-3 hours before taking more
- Increase by 2.5 mg every few days if needed
- Most patients find relief between 5-15 mg THC per dose For CBD-only products (even though evidence is weak):
- Start with 10-20 mg CBD
- Take twice daily
- Give it at least 2-4 weeks to assess effect
- Don’t exceed 100 mg/day without medical supervision For 1:1 THC:CBD products (like Sativex):
- Start with 1 spray under the tongue
- Wait 30 minutes
- Increase by 1 spray every 2-3 days
- Max usually 12 sprays per day The biggest mistake? Taking too much too soon. High doses of CBD can cause liver enzyme changes. THC can cause dizziness, anxiety, or impaired coordination. Always start low and go slow.
Safety Risks: What No One Tells You
Cannabinoids aren’t risk-free. And the biggest danger isn’t the compound itself-it’s the product. A University of Bath study tested 25 over-the-counter CBD products. Half contained less CBD than labeled. Some had none at all. A few had illegal levels of THC. Others had heavy metals, pesticides, or synthetic cannabinoids. That’s why people get false results. You think CBD isn’t working. But you’re not even getting the dose you paid for. Other risks:- Liver toxicity at high CBD doses (above 100-200 mg/day)
- Drug interactions with blood thinners, antidepressants, and seizure meds (CBD affects liver enzymes that break down these drugs)
- Psychoactive effects from hidden THC
- Positive drug tests, even with “THC-free” products
- Withdrawal symptoms if stopping after long-term use The CDC warns that long-term safety data is still lacking. We don’t know what happens if you take CBD daily for 10 years.
Real-World Outcomes: Hope vs. Reality
The market for CBD is booming. The U.S. CBD industry hit $4.3 billion in 2022. Yet, most of those sales are based on claims no science backs. Amazon reviews for top-selling CBD oils show a pattern: 41% of negative reviews say “no pain relief.” Only 22% mention improved sleep. 28% say it helped with anxiety. That’s telling. It suggests people are using CBD for pain, but getting relaxation instead. One patient on Leafly described switching from 120 mg of oxycodone daily to a 1:1 THC:CBD tincture. She got the same pain control with fewer side effects and no risk of overdose. That’s the kind of story that matters. But it’s not the norm. It’s the exception. And it only happened because she used a regulated, pharmaceutical-grade product under medical guidance.What’s Next? The Future of Cannabinoid Pain Treatment
Research is shifting. The focus is no longer on CBD alone. Scientists are now testing CBG, CBN, and balanced THC:CBD formulas. Phase III trials are underway for cancer pain and chronic low back pain, with results expected by 2025. The FDA is reviewing whether to reschedule cannabis from Schedule I. If that happens, research funding will surge. We could see the first FDA-approved cannabinoid pain drug by 2027. Until then, the message is clear: don’t trust the internet. Don’t believe the hype. And don’t replace your current pain treatment without talking to your doctor. If you’re considering cannabinoids for pain:- Only use products from licensed medical cannabis dispensaries (not gas stations or Amazon)
- Ask for lab reports (COAs) showing exact cannabinoid content and absence of contaminants
- Start with low-dose THC:CBD combinations if allowed in your state
- Track your pain levels daily with a simple 1-10 scale
- Give it 4-6 weeks before deciding if it works



veronica guillen giles
Oh wow, another article that says 'CBD doesn't work' like we didn't already know that from the 47 gummy boxes gathering dust under my sink. 🙄 I spent $200 on 'premium' CBD for my sciatica and ended up just really relaxed while watching Netflix. Turns out my nerves needed a nap, not a miracle. But hey-at least I didn't get arrested for buying something that's technically illegal in 12 states but sold next to beef jerky at 7-Eleven.
Ian Ring
Thank you for this thoughtful, well-referenced breakdown. 🙏 It's frustrating how the market has exploded without regulation-people are literally gambling with their health on Amazon. I've seen patients on my caseload spend hundreds on CBD tinctures that tested at 0.2% CBD. The science is nuanced, yes-but the marketing is predatory. Always ask for COAs. Always. And if your dispensary can't produce one, walk out. No exceptions.
erica yabut
Let’s be brutally honest: the CBD industry is a postmodern capitalist fever dream-part wellness cult, part Ponzi scheme disguised as a wellness brand. We’ve elevated a plant compound to the status of a spiritual talisman while ignoring the actual pharmacology. It’s not ‘natural’ if it’s laced with synthetic cannabinoids and sold in a glittery bottle with a yoga instructor smiling on the label. The FDA hasn’t approved it for pain because it doesn’t work as advertised. And yet, here we are, worshipping at the altar of alkaloids while ignoring proven modalities like physical therapy, acupuncture, or even cognitive behavioral therapy. Pathetic.
Tru Vista
THC works for nerve pain. CBD? Nope. Studies show it. Sativex is legit. OTC CBD? Scam. Lab reports? Rare. Liver tox? Real. Dosing? No clue. Just start low. Don't be dumb. Also, stop buying it on Amazon. 😴
Vincent Sunio
It is both intellectually dishonest and professionally irresponsible to conflate anecdotal testimonials with clinical evidence. The preponderance of peer-reviewed, randomized, double-blind, placebo-controlled trials demonstrates conclusively that isolated CBD lacks statistically significant analgesic efficacy beyond placebo for chronic non-neuropathic pain conditions. The conflation of cannabis-derived products with pharmaceutical-grade cannabinoid formulations is not merely misleading-it is dangerous. One cannot extrapolate the therapeutic profile of Sativex to a $19.99 tincture purchased from a gas station. The regulatory vacuum in this space is a public health liability.
JUNE OHM
THEY DON'T WANT YOU TO KNOW THIS BUT CBD IS A BIG PHARMA COVER-UP!! 🇺🇸 They're scared because if you can heal pain with a plant, you don't need their $10,000 opioids or their patented drugs that make them billions. The FDA is in the pocket of Big Pharma. They banned cannabis in 1937 because cotton and paper companies wanted to kill hemp. Now they're lying to you about 'no evidence'-but my cousin in Colorado? Pain gone. No more morphine. 🚩🚩🚩
Philip Leth
Man, I grew up in Jamaica-we used ganja for back pain since forever. No lab reports, no fancy bottles, just smoke it or make tea. My abuela? 82, arthritic knees, never took a pill. Just a little herb at night. Now I’m in the States, paying $60 for a bottle that says ‘1000mg CBD’ but the lab report says 87mg? That’s not wellness, that’s robbery. The real answer? Find someone who knows what they’re doing. Not some influencer with a vape pen and a yoga mat.
Angela Goree
I’ve been using THC/CBD tincture for 3 years for fibro. 1:1. 7.5mg each. Twice a day. Pain? Down 60%. Sleep? Better. Anxiety? Gone. But I bought it from a licensed dispensary in Michigan. COA? Always. I track everything. 1-10 scale. Journal. I’m not some idiot buying Amazon junk. And I’m sick of people acting like this is magic. It’s medicine. Treat it like it. And if you’re too lazy to research? Then don’t blame the plant when it doesn’t work.