When you hear the buzz around prebiotics and inflammation, it usually comes with a promise of a calmer gut and a healthier body. But what’s the real connection? Below we break down the science, point out the foods that matter, and give you a practical roadmap to use prebiotics for reducing inflammation.
Quick Takeaways
- Prebiotics are non‑digestible fibers that feed beneficial gut microbes.
- These microbes produce short‑chain fatty acids (SCFAs) that tighten the gut barrier and dampen inflammatory signals.
- Inulin, fructooligosaccharides (FOS), galactooligosaccharides (GOS) and resistant starch are the most studied anti‑inflammatory prebiotics.
- Adding 5‑15g of prebiotic fiber daily can lower markers like C‑reactive protein (CRP) in many people.
- Pair prebiotics with a diverse diet and regular movement for the best results.
What Are Prebiotics?
Prebiotics are dietary fibers that resist digestion in the upper gastrointestinal tract and reach the colon alive, where they serve as food for beneficial gut bacteria. Common examples include inulin, fructooligosaccharides (FOS), galactooligosaccharides (GOS) and resistant starch. Unlike probiotics, which are live microorganisms, prebiotics act like fertilizer for the microbes already living in your intestines.
Understanding Inflammation
Inflammation is a complex immune response triggered by injury, infection or metabolic stress, marked by the release of cytokines, prostaglandins and other signaling molecules. Acute inflammation protects, but chronic low‑grade inflammation underlies conditions such as obesity, type‑2 diabetes, cardiovascular disease and inflammatory bowel disease (IBD).
How Prebiotics Talk to the Immune System
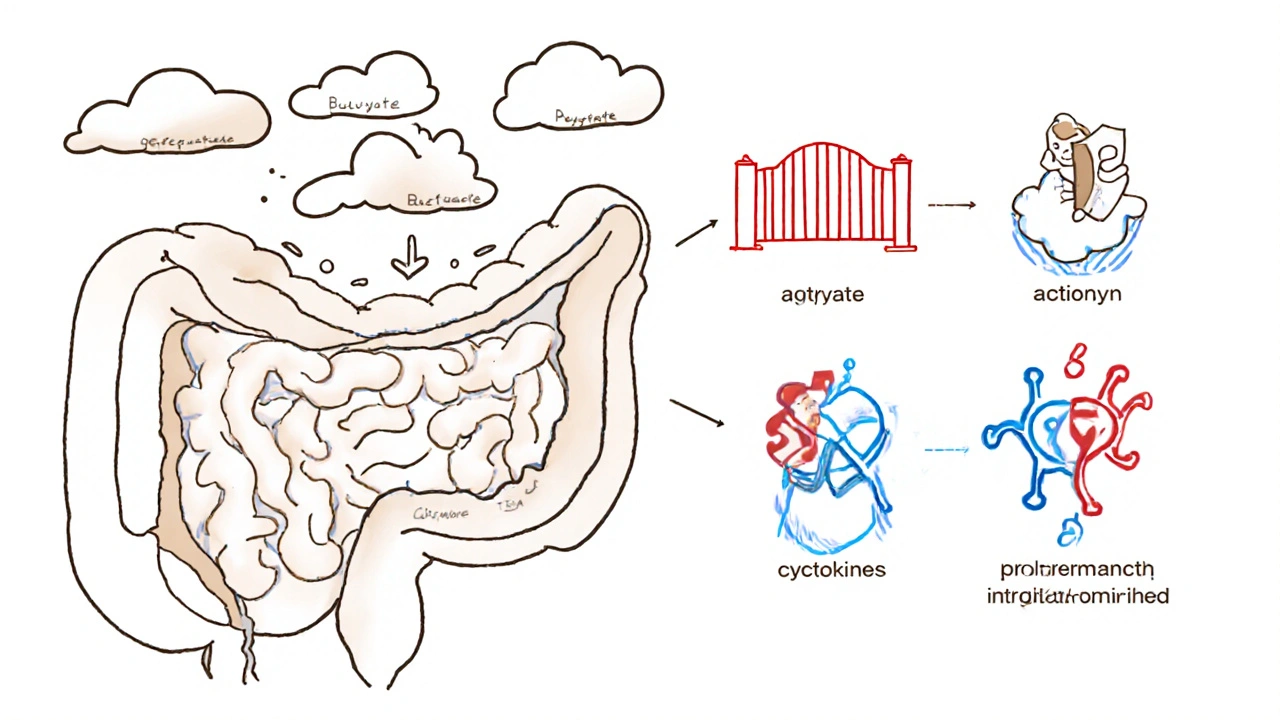
The gut hosts roughly 70% of the body’s immune cells. When prebiotics reach the colon, they ferment into short‑chain fatty acids (SCFAs) - mainly acetate, propionate and butyrate. These SCFAs have three key anti‑inflammatory actions:
- Barrier reinforcement: Butyrate fuels colonocytes, tightening tight junctions and preventing endotoxin leakage (metabolic endotoxemia) that would otherwise provoke systemic inflammation.
- Regulatory T‑cell promotion: SCFAs stimulate the production of Foxp3⁺ regulatory T cells, which keep pro‑inflammatory Th‑17 cells in check.
- Cytokine modulation: They blunt the release of tumor necrosis factor‑α (TNF‑α) and interleukin‑6 (IL‑6) while boosting anti‑inflammatory interleukin‑10 (IL‑10).
In short, a fiber‑rich diet gives your gut microbes the tools to keep the immune system from over‑reacting.
Evidence from Human Studies
Several randomized controlled trials (RCTs) have examined prebiotic supplementation and inflammatory biomarkers:
- Inulin (10g/day, 12weeks) lowered serum CRP by 18% in overweight adults (J. Nutr. 2022).
- FOS (8g/day, 8weeks) reduced fecal calprotectin - a gut‑specific inflammation marker - by 22% in patients with mild ulcerative colitis (Gut Microbes 2023).
- Resistant starch (15g/day, 6weeks) decreased IL‑6 and TNF‑α in type‑2 diabetics by 12% and 15% respectively (Diabetes Care 2024).
Meta‑analyses published in 2024 across 27 trials conclude that prebiotic intake of 5‑20g per day yields a modest but statistically significant reduction in systemic inflammatory markers.
Choosing the Right Prebiotic for Anti‑Inflammatory Benefits
| Prebiotic Type | Key SCFA Produced | Typical Dose (g/day) | Evidence of Inflammation Reduction |
|---|---|---|---|
| Inulin (chicory root) | Butyrate > Propionate | 5‑10 | CRP ↓ 10‑20% (over 8‑12wks) |
| Fructooligosaccharides (FOS) | Propionate > Acetate | 5‑8 | Fecal calprotectin ↓ 15‑25% (8wks) |
| Galactooligosaccharides (GOS) | Acetate > Butyrate | 4‑6 | IL‑10 ↑, TNF‑α ↓ (6‑10wks) |
| Resistant Starch (unripe bananas, cooked‑cooled potatoes) | Butyrate dominant | 10‑20 | IL‑6 & TNF‑α ↓ 10‑15% (6wks) |
Pick a type that fits your dietary preferences and start low (3‑5g) to avoid gas or bloating, then gradually increase to the target dose.
Practical Ways to Add Prebiotics to Your Day
- Morning smoothie: Blend a tablespoon of chicory‑root inulin powder with banana and almond milk.
- Snack boost: Swap regular crackers for a handful of raw Jerusalem artichoke slices (high in inulin).
- Side dish: Add cooked lentils or chickpeas (rich in resistant starch) to salads.
- Evening prep: Cool a pot of quinoa or rice, then reheat - the cooling process creates resistant starch.
- Supplement option: If whole foods feel too much, choose a certified prebiotic capsule (look for 5‑10g of FOS or GOS per dose).
Remember: diversity matters. A mix of fibers feeds a broader range of microbes, which in turn creates a richer SCFA profile.

Potential Pitfalls and How to Avoid Them
While prebiotics are generally safe, a few issues can arise:
- Gas and bloating: Increase intake slowly; split the dose across meals.
- Underlying IBS: People with irritable bowel syndrome may need to stay below 5g/day or choose low‑FODMAP prebiotics like partially hydrolyzed guar gum.
- Over‑reliance on supplements: Whole‑food sources provide micronutrients and polyphenols that further support anti‑inflammatory pathways.
If symptoms persist, consult a gastroenterologist or dietitian.
Frequently Asked Questions
Can prebiotics replace anti‑inflammatory medication?
No. Prebiotics can lower inflammation markers and improve gut health, but they are not a substitute for prescribed drugs. Use them as a complement under medical guidance.
How quickly can I expect to see a change in CRP levels?
Most RCTs report measurable reductions after 8‑12weeks of consistent prebiotic intake at therapeutic doses (5‑15g/day).
Are there any foods that are both probiotic and prebiotic?
Yes-foods like kefir, kimchi, and kombucha contain live cultures (probiotics) and, when made with fiber‑rich substrates, also deliver prebiotic compounds.
Is there a difference between soluble and insoluble fiber for inflammation?
Soluble fibers (e.g., inulin, pectin) ferment into SCFAs and have the strongest anti‑inflammatory effect. Insoluble fibers mainly add bulk and aid regularity.
Can I take prebiotics if I’m on a low‑carb diet?
Yes, but choose low‑carb sources like chicory root inulin powder or small portions of resistant starch from cooled cauliflower. Keep total carbs within your daily limit.
Next Steps: Building an Anti‑Inflammatory Routine
1. Audit your current diet. Identify fiber gaps - most adults get under 15g of prebiotic fiber a day.
2. Add one new prebiotic source each week. Start with inulin powder in coffee, then rotate to lentils, then roasted Jerusalem artichokes.
3. Track symptoms and biomarkers. Use a simple journal for bloating, energy, and, if possible, have a blood test for CRP after 8weeks.
4. Combine with lifestyle habits. Regular moderate exercise, adequate sleep, and stress‑reduction techniques amplify the anti‑inflammatory impact of prebiotics.
By feeding the right microbes, you give your immune system a better chance to stay calm, and you set the stage for long‑term health.




Steve Holmes
Whoa, I just finished reading the deep dive on prebiotics and inflammation, and I’m amazed! The way those non‑digestible fibers act like fertilizer for our gut microbes is mind‑blowing, especially when you consider the cascade of short‑chain fatty acids that follow. First, the butyrate production strengthens the gut barrier, which keeps those nasty endotoxins from leaking into the bloodstream-yeah, that’s a huge win for systemic inflammation. Then, the promotion of regulatory T‑cells helps keep the immune system from going overboard, a subtle yet powerful effect. The article even points out real‑world data: a 10‑gram daily dose of inulin slashing CRP by almost a fifth in just twelve weeks! Imagine combining that with a few weeks of resistant starch and seeing IL‑6 and TNF‑α dip together. I’ve been slowly adding a tablespoon of chicory‑root inulin to my morning coffee, and after a month I noticed less bloating and a steadier energy curve. The key, as the piece stresses, is to start low-3‑5 g is enough to avoid gas, then ramp up to the therapeutic sweet spot of 10‑15 g. It’s also fascinating how a diverse fiber portfolio-mixing inulin, FOS, and some resistant starch-creates a richer SCFA profile, essentially giving your gut a balanced playlist. The author’s practical tips, like cooling rice to boost resistant starch, are gold nuggets you can try tomorrow. And remember, the gut houses about 70 % of our immune cells, so feeding those microbes is like giving the immune system a calm mentor. Lastly, the meta‑analysis from 2024 confirms that the effect is modest but consistent across populations, which tells us this isn’t just a fad. So, if you’re curious about dialing down chronic inflammation, grab a bag of Jerusalem artichoke chips, sprinkle some GOS powder on your smoothie, and stay consistent-your gut (and maybe your joints) will thank you! Consistency is key, because the gut microbiome adapts over weeks, not days, and you’ll notice the most benefit after about two months of steady intake. Keep tracking your symptoms and, if possible, get a follow‑up CRP test to see the numbers move in the right direction.
Tom Green
Great summary! For anyone just starting out, I’d suggest picking one prebiotic source you already like-maybe inulin powder for your coffee or a side of lentils for dinner-and introduce it gradually. Aim for 3‑5 g per day the first week, then step up by 2‑3 g each subsequent week until you hit the 10‑15 g range the article mentions. Pair this with a colorful array of vegetables and regular movement, and you’ll create a solid foundation for gut‑immune balance.
Emily Rankin
Indeed, the journey of feeding our inner microbial garden can feel like a heroic quest! Picture the gut as a bustling city, each fiber a generous donation that funds the construction of sturdy walls (the tight junctions) and peace‑keeping forces (regulatory T‑cells). When we honor these tiny allies with a varied diet, the whole organism sings in harmony, and the chronic inflammation monsters lose their power. Let’s celebrate each small step-whether it’s a spoonful of chicory‑root or a cooled‑potato side-as a triumph worth shouting about.
Rebecca Mitchell
Prebiotics work.
CHIRAG AGARWAL
Honestly, I could care less about the hype-if you’re not feeling any difference after a month, maybe it’s just marketing fluff, not magic.
genevieve gaudet
i think its coolh how they talk bout pre-bio-tics n how they fix gut, but some peepz may not get it coz they cant read the scientfic stuff LOL
Patricia Echegaray
Don't forget that big pharma doesn't want you to know how simple fibers can tame inflammation; they're busy selling pricey anti‑inflammatory drugs while the real cure sits on the grocery aisle, hidden in plain sight.
Miriam Rahel
Whilst the article provides a comprehensive overview of prebiotic mechanisms, it would benefit from a more rigorous examination of the heterogeneity among study populations, particularly concerning baseline microbial composition, which may significantly modulate response to fibre supplementation.
Samantha Oldrid
Oh sure, because a handful of chicory root will magically erase years of lifestyle‑induced inflammation. 🙄
Richard O'Callaghan
i thnik the key is to start smalld and gautingly incres the amt, otherwise you get gut bloat and not much benifit.
Darryl Gates
Exactly, Richard-gradual increase is the smartest approach. Start with a teaspoon of inulin in a smoothie, monitor how your belly feels, and then step it up. Consistency beats intensity any day.
Chris Beck
These claims sound good but real life results vary a lot.
Winston Bar
Well, if you look at the data, the reductions in CRP are modest at best; you could just as easily chew gum and see similar tiny changes.
Russell Abelido
I totally get the frustration, Winston 😅. It can feel underwhelming when the numbers shift just a few points, but even a small dip in systemic inflammation can translate to better sleep, clearer skin, and more stable energy. Keep at it, and celebrate the tiny wins! 🌱😊
Katie Henry
In conclusion, adopting a structured prebiotic regimen-anchored in evidence‑based dosing, diversified fiber sources, and regular monitoring-offers a viable strategy for attenuating chronic inflammation and fostering overall health. I encourage practitioners and patients alike to integrate these guidelines into their therapeutic plans.