When your doctor suspects liver damage, you might expect a needle going into your liver. But that’s not the only option anymore. Today, two powerful tools-FibroScan and serum scores-can tell you how much scarring (fibrosis) is in your liver without a single incision. And with fatty liver disease affecting nearly 1 in 4 people worldwide, these tests are no longer niche. They’re becoming routine.
What FibroScan Actually Measures
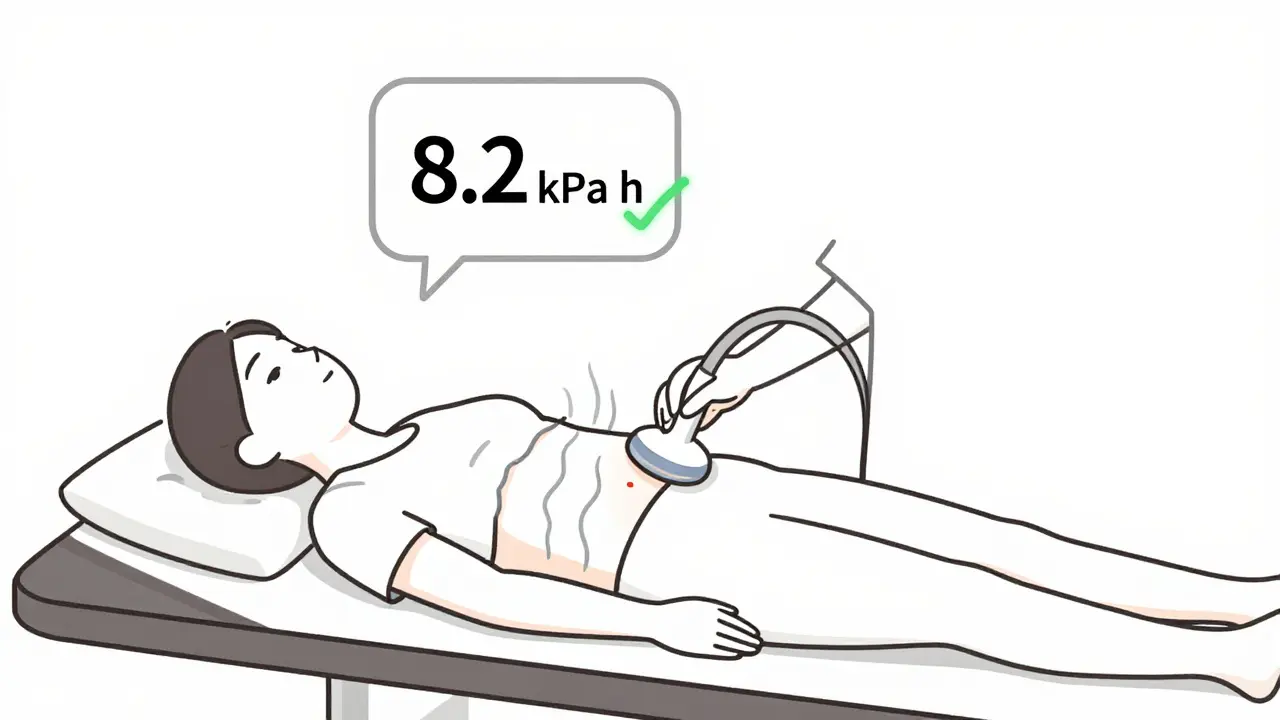
FibroScan isn’t a fancy ultrasound. It’s a device that sends low-frequency sound waves through your liver and measures how fast they travel. Stiff liver tissue-signs of scarring-makes those waves move faster. The result? A number in kilopascals (kPa). Normal is 2-7 kPa. Above 7? That’s a red flag. Above 12? Likely advanced fibrosis or cirrhosis.
The device uses two probes: one for thinner people (S probe), another for those with higher body fat (XL probe). If you have a BMI over 28 or a lot of liver fat, the XL probe is often needed. But here’s the catch: if you’ve eaten within the last 3 hours, or if you have active hepatitis or heart failure, the reading can be wrong. That’s why technicians take at least 10 measurements. If more than 30% of them vary wildly, the test is invalid. About 1 in 10 tests fail in real-world clinics-not because the machine is broken, but because the conditions aren’t perfect.
On top of stiffness, FibroScan also measures fat in your liver using CAP (Controlled Attenuation Parameter). A CAP score of 238-260 dB/m means 11-33% fat. 260-290? That’s 34-66%. Above 290? You’re looking at severe fatty liver. But CAP isn’t perfect. In obese patients, it overpredicts fat by as much as 81%. That’s why some doctors say, “Trust the FibroScan, but don’t believe everything it says.”
Serum Scores: Blood Tests That Do the Heavy Lifting
While FibroScan is a machine you sit in front of, serum scores are just blood tests you’ve probably already had. No special equipment. No appointment. Just your routine liver panel and platelet count.
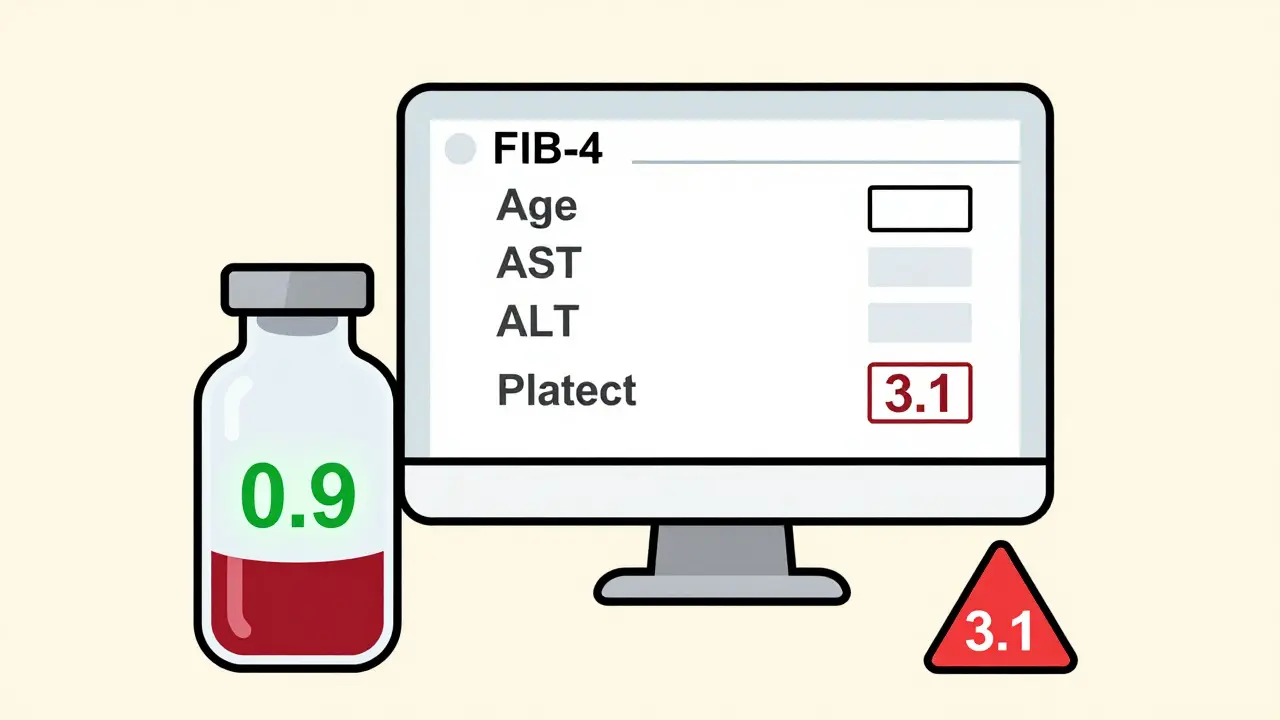
The most common one is FIB-4. It uses your age, AST, ALT, and platelet count. If your score is below 1.3, you’re very unlikely to have advanced fibrosis. That’s powerful. It means you might not need any further testing. But if it’s above 2.67? You’ve got a high chance of serious scarring. The problem? FIB-4 misses nearly 83% of advanced cases in people under 35. It’s designed for middle-aged and older adults. In younger people, its accuracy drops from 85% to 67%.
Then there’s APRI. It’s simpler: just AST and platelets. A score above 2.0 suggests cirrhosis. But it’s not great at spotting early scarring. It’s better at ruling out the worst cases. The ELF test is more complex, measuring three proteins linked to liver scarring. It’s more accurate than FIB-4 or APRI, especially when results are unclear. But it’s also more expensive and not always available outside specialty clinics.
The big advantage of serum scores? They’re cheap. FIB-4 costs about $10 to calculate. FibroScan? $50 to $150 per test. In clinics with tight budgets, serum scores are the only option. And because they’re built into electronic health records, some primary care doctors now screen 67% of at-risk patients-up from just 12% before.
Accuracy Wars: Which Test Gets It Right?
Here’s where things get messy. One 2023 study found FibroScan correctly identified only 45.9% of patients with advanced fibrosis (F3/F4). That sounds terrible. But another study showed FibroScan had a 99% accuracy rate for diagnosing cirrhosis (F4). So what’s going on?
It’s about the stage. FibroScan is great at spotting the worst cases-cirrhosis. But it struggles with moderate scarring. Serum scores like FIB-4 are better at saying, “You’re probably fine,” than “You’re in trouble.” FIB-4 has a 90% negative predictive value. That means if your score is below 1.3, you can relax. You almost certainly don’t have advanced fibrosis.
But if you have a high FIB-4 score? You can’t stop there. You need FibroScan to confirm. That’s why guidelines now say: start with FIB-4. If it’s low, you’re clear. If it’s high, get a FibroScan. If they disagree? That’s when you consider a biopsy.
And here’s a real-world surprise: in one study, a patient’s FibroScan said F2 (moderate scarring), FIB-4 said high risk, and the biopsy showed F3 (advanced). Both tests were wrong. That’s why no single test is trusted alone anymore. The best answer comes from combining them.
What Experts Really Think
Dr. Brent Tetri from Saint Louis University says bluntly: “FibroScan’s 54.1% false negative rate means we’re missing half the people who need help.” He’s not saying the test is useless. He’s saying it’s not a magic bullet.
Professor Manal Abdelmalek from Duke warns about CAP’s overprediction in obese patients. “You can’t treat fat based on a machine reading alone,” she says. “You need to look at the whole picture: diet, diabetes, activity levels.”
And Dr. Zobair Younossi, editor of Hepatology, puts it plainly: “If you rely only on serum markers, you’re letting advanced liver disease slip through the cracks.”
The European Association for the Study of the Liver (EASL) has a clear protocol: use FIB-4 first. If it’s borderline, use FibroScan. Only if they contradict each other-and you’re still unsure-do you go for a biopsy. That approach cuts biopsy rates by 70%.
Real People, Real Problems
On Reddit, users share stories. One person with a BMI of 38 had to try three times before the XL probe worked. Cost? Extra $200. Another said, “My doctor said my FibroScan was fine, but my FIB-4 was sky-high. I got a biopsy. Turns out I had F3. Both tests missed it.”
Doctors on professional forums say the same thing: 10-15% of FibroScan tests are unreliable. That’s not operator error. That’s physics. Fat, fluid, inflammation-they all interfere. Meanwhile, serum scores are praised for being automatic. “I don’t even have to think about it,” says Dr. Sarah Chen. “The system calculates FIB-4 as soon as the blood results come in.”
But patients get confused. 43% of those surveyed by the NAFLD Foundation said they didn’t understand why two tests gave different answers. And when a biopsy comes back different from both? That’s when trust in the system cracks.
What’s New in 2026?
The latest FibroScan model, the 730, launched in April 2024, uses AI to judge if a reading is trustworthy. Early results show it cuts technical failures by 22%. That’s huge.
And there’s a new serum score: FIB-5. It adds glucose levels to the mix. In diabetic patients with fatty liver, it’s 89% accurate at spotting advanced fibrosis. That’s better than FIB-4.
Big research groups like the NIH are now testing a three-part combo: FibroScan + FIB-4 + ELF. In pilot studies, this trio reduced unnecessary biopsies by 82% while catching 94% of all cirrhosis cases.
What Should You Do?
If you’re at risk-overweight, diabetic, have high liver enzymes, or drink alcohol regularly-ask your doctor for FIB-4. It’s fast, cheap, and if it’s low, you’re probably safe.
If FIB-4 is high or borderline, ask for FibroScan. Don’t assume it’s perfect. Ask if the technician used the right probe. Ask if you were fasting. Ask if the results met reliability standards (IQR under 30%).
If the two tests disagree? Don’t panic. Ask if an ELF test is available. If not, a biopsy might be the only way to know for sure.
There’s no perfect test. But there’s a smart way to use them together. And that’s the new standard of care.
Can FibroScan replace a liver biopsy?
No. FibroScan is excellent at ruling out or confirming advanced fibrosis and cirrhosis, but it can’t replace biopsy in all cases. Biopsy is still the gold standard when results from FibroScan and serum scores conflict, or when the doctor suspects something unusual like autoimmune liver disease. Guidelines recommend biopsy only when non-invasive tests give unclear answers.
Is FibroScan accurate for obese patients?
It can be, but it’s harder. Standard probes often fail in patients with BMI over 28. The XL probe helps, but even then, technical failures happen in 10-15% of cases. CAP scores for liver fat also overestimate in obese people. That’s why doctors always combine FibroScan with other tests like FIB-4 in overweight patients.
How often should I get tested for liver fibrosis?
If you have NAFLD or NASH and are at risk, get tested once a year. If your first test shows low risk (FIB-4 <1.3, FibroScan <7 kPa), you might wait two years. If you have high risk or are being treated, your doctor may recommend testing every 6-12 months. Don’t test more often unless your condition changes or your doctor recommends it.
Can alcohol affect FibroScan results?
Yes. Drinking alcohol within 24-48 hours before the test can cause temporary liver inflammation, which makes the liver appear stiffer than it is. This leads to falsely high readings. Always avoid alcohol for at least 2 days before your FibroScan. Same goes for fasting-don’t eat for 3 hours before the test.
Are serum scores like FIB-4 reliable for young people?
Not really. FIB-4 was designed for people over 35. In younger adults, its accuracy drops significantly because liver enzymes and platelet counts naturally fluctuate more. For people under 35, FibroScan or ELF is preferred. Some doctors now use FIB-5 for younger patients with diabetes, since it includes glucose levels.
Why do some doctors only use FIB-4 and skip FibroScan?
Cost and access. FibroScan machines cost tens of thousands of dollars and require trained operators. Many primary care clinics don’t have them. FIB-4 uses blood tests already ordered for liver health. It’s automatic, free, and fast. So in resource-limited settings, FIB-4 is used as a screening tool to find who needs referral-saving FibroScan for those who truly need it.
What’s the future of liver fibrosis testing?
The future is multi-test algorithms. Combining FibroScan, FIB-4, and ELF gives the most accurate picture. New AI tools are improving reliability. In the next 5 years, smartphone-based elastography and blood biomarkers for early scarring may become mainstream. But for now, the best strategy is using the right test at the right time-not the most expensive one.