When your hormones are out of balance, your bones pay the price. This isn’t just a theory-it’s a clinical reality for millions with endocrine disorders like type 1 diabetes, hyperthyroidism, or hypogonadism. These conditions don’t just affect metabolism or energy levels; they directly attack bone strength. Many patients with these diseases have normal or only slightly low bone density on DEXA scans, yet still break bones from minor falls. Why? Because bone quality, not just density, is broken. That’s where FRAX and bisphosphonates come in-two tools that have changed how doctors assess and treat osteoporosis in people with hormonal disorders.
Why Endocrine Diseases Break Bones
Endocrine diseases mess with the body’s natural bone-building cycle. Bone isn’t static-it’s constantly being broken down by cells called osteoclasts and rebuilt by osteoblasts. Hormones like estrogen, testosterone, thyroid hormone, and insulin keep this process in check. When they’re too high, too low, or absent, the balance tips toward bone loss. In type 1 diabetes, fracture risk jumps 6 to 7 times higher-even when bone density looks normal. That’s the "diabetic paradox." The problem isn’t just low calcium. High blood sugar damages collagen in bone, reduces blood flow to bone tissue, and increases inflammation. These changes weaken bone structure in ways a DEXA scan can’t measure. Untreated hyperthyroidism is another silent bone thief. Too much thyroid hormone speeds up bone turnover. Bone gets broken down faster than it’s rebuilt. Studies show even mild, subclinical thyroid overactivity increases fracture risk by 15-20%. Hypogonadism-low testosterone in men or estrogen in women-causes bone loss at 2-4% per year. That’s faster than most postmenopausal women lose bone. And if you’re on androgen deprivation therapy for prostate cancer? You’re in the high-risk zone.FRAX: The Calculator That Sees Beyond DEXA
For years, doctors relied on DEXA scans alone. A T-score below -2.5 meant osteoporosis. Simple. But that approach misses too many people with endocrine disease. That’s why FRAX was created. Developed by the University of Sheffield in 2008, FRAX isn’t a machine. It’s a free, web-based algorithm that calculates your 10-year risk of a major osteoporotic fracture (like hip, spine, wrist, or shoulder) or a hip fracture specifically. It uses nine clinical risk factors: age, sex, BMI, prior fracture, parental hip fracture history, smoking, steroid use, alcohol intake (more than 3 units/day), and rheumatoid arthritis. Here’s the key: for endocrine disease patients, FRAX includes their condition as a risk factor-even if their DEXA scan looks okay. But here’s the catch: FRAX still underestimates fracture risk in type 1 diabetes by about 30%. That’s why experts now recommend using FRAX with BMD, not without it. Adding femoral neck bone density to the model improves accuracy dramatically. And now there’s an upgrade: the FRAX-adjusted Trabecular Bone Score (TBS). This isn’t another scan. It’s a computer analysis of the DEXA image that measures bone texture. Poor texture means weaker, more fragile bone-common in diabetes and hyperthyroidism. TBS helps catch what DEXA misses. The NIH recommends TBS for endocrine patients with osteopenia or borderline FRAX scores.When to Treat: The 3% and 20% Rules
Treatment doesn’t start because your T-score is -1.8. It starts because your risk is high enough to justify drugs with side effects. The Bone Health and Osteoporosis Foundation sets clear thresholds:- Treat if you’ve had a hip or spine fracture-no matter your T-score.
- Treat if your T-score is -2.5 or lower.
- Treat if your T-score is between -1 and -2.5 (osteopenia) AND your 10-year FRAX risk is 20% or higher for a major fracture, or 3% or higher for a hip fracture.

Bisphosphonates: The First-Line Shield
Bisphosphonates are the most studied, most prescribed drugs for osteoporosis. They include alendronate (Fosamax), risedronate (Actonel), ibandronate (Boniva), and zoledronic acid (Reclast). All work the same way: they stick to bone and shut down osteoclasts-the cells that chew up bone. The results? In clinical trials, bisphosphonates reduce vertebral fractures by 40-70% and hip fractures by 40-50%. For someone with endocrine disease, that’s life-changing. A 2023 Kaiser Permanente review confirmed these drugs work just as well in patients with diabetes or thyroid disorders as they do in the general population. There’s a reason they’re first-line: they’re cheap, effective, and well-understood. Oral versions are taken weekly or monthly. Zoledronic acid is an annual IV infusion-ideal for people who struggle with daily pills. Treatment usually lasts 3-5 years for oral bisphosphonates, or 3 years for zoledronic acid. After that, your doctor reassesses. If your FRAX score is still high and your T-score hasn’t improved, you might continue. If your risk has dropped, you might take a "drug holiday"-a pause in treatment while monitoring bone markers.Limitations and Controversies
FRAX isn’t perfect. It doesn’t capture everything. In type 1 diabetes, it still underestimates risk. In patients with chronic kidney disease or liver disease-common in endocrine disorders-it may not be accurate at all. That’s why experts stress: FRAX is a guide, not a rule. Some endocrinologists argue that all patients with type 1 diabetes over 50 should get a DEXA scan regardless of FRAX score. Others say the 3% hip fracture threshold is too low for younger patients with multiple risk factors. There’s no universal agreement. And bisphosphonates? They’re not risk-free. Rare side effects include jawbone problems (osteonecrosis) and unusual thigh fractures after long-term use. But these are extremely uncommon-less than 1 in 10,000 patients per year. The risk of breaking a hip without treatment is far higher.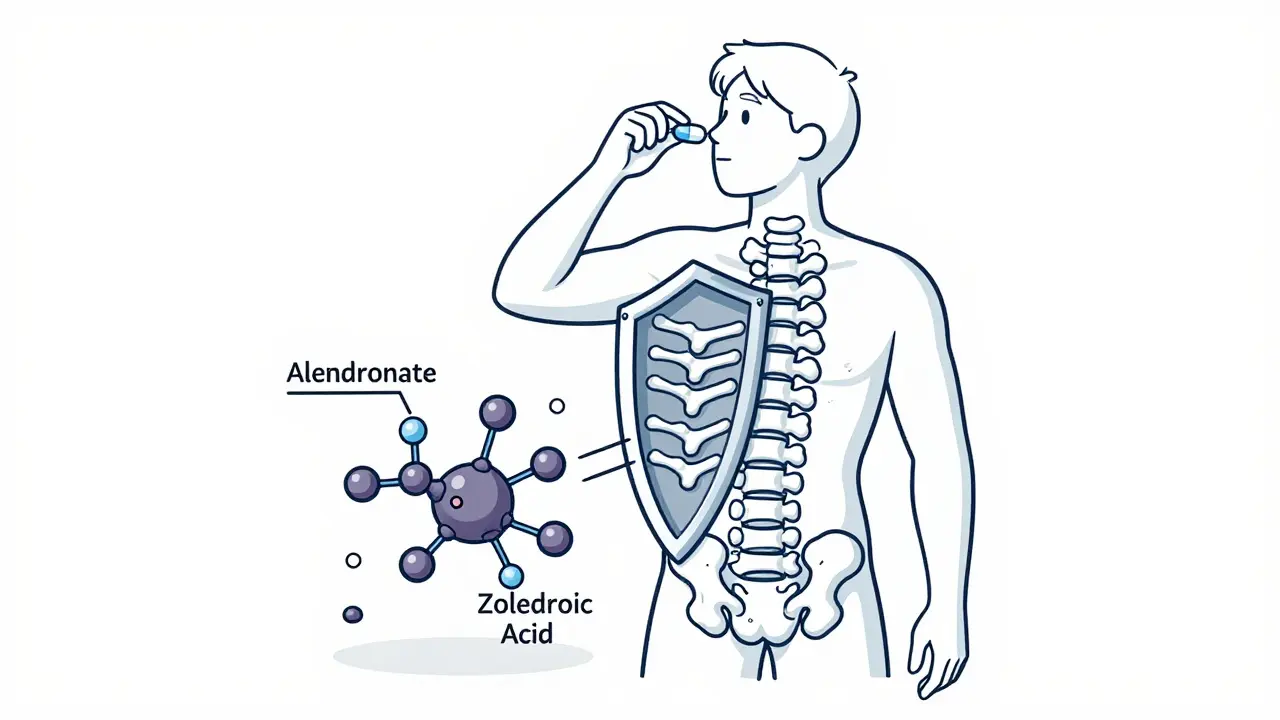
What Happens Next?
The field is evolving fast. The Bone Health and Osteoporosis Foundation is testing diabetes-specific FRAX adjustments. Early data shows they improve risk prediction by 25%. That means better targeting of treatment. Researchers are also exploring new biomarkers-blood or urine tests that measure bone turnover or collagen damage-that could replace or supplement DEXA. Artificial intelligence is being trained to combine FRAX, TBS, lab values, and even walking speed to predict fracture risk with more precision. By 2025, most endocrinologists will use FRAX with endocrine-specific adjustments. That’s the direction we’re heading. But right now, the tools we have-FRAX, DEXA, TBS, and bisphosphonates-are enough to save lives and prevent fractures.What You Should Do
If you have an endocrine disorder and are over 50-or under 50 with risk factors like a prior fracture, steroid use, or early menopause-ask your doctor for a FRAX assessment. Don’t wait for a fracture to happen. Get a DEXA scan if your FRAX score is above 9.3% for major fractures. If your score is borderline, ask about TBS. If you’re diagnosed with osteopenia or osteoporosis, discuss bisphosphonates. Don’t assume normal BMD means you’re safe. And if you’re on long-term steroids, have type 1 diabetes, or have had multiple fractures? Push for a referral to an endocrinologist. This isn’t just about bones. It’s about your whole health.Can FRAX be used for people with type 1 diabetes?
Yes, but it underestimates fracture risk by about 30%. FRAX should always be used with a DEXA scan and, if available, the Trabecular Bone Score (TBS) for people with type 1 diabetes. New diabetes-specific FRAX adjustments are being tested and may soon improve accuracy.
Do bisphosphonates work for endocrine-related osteoporosis?
Yes. Clinical trials show bisphosphonates reduce hip and spine fracture risk by 40-70% in patients with endocrine disorders like diabetes, hyperthyroidism, and hypogonadism. Treatment guidelines treat them the same as the general population: if your 10-year fracture risk meets the threshold, bisphosphonates are first-line therapy.
Is a DEXA scan enough to diagnose osteoporosis in endocrine disease?
No. Many patients with endocrine disorders have normal or near-normal bone density but still break bones. FRAX, TBS, and clinical history are needed to fully assess risk. Relying only on DEXA can miss up to 40% of high-risk patients.
How long should someone take bisphosphonates?
Typically 3-5 years for oral bisphosphonates, or 3 years for annual zoledronic acid infusions. After that, doctors reassess fracture risk using FRAX and repeat DEXA scans. If risk remains high, treatment may continue. If risk is low, a drug holiday may be safe.
Who should get a FRAX assessment?
All postmenopausal women and men over 50 with any clinical risk factor for fracture-including endocrine disorders like diabetes, thyroid disease, or hypogonadism. Even if you’re younger than 50, if you’ve had a fragility fracture or are on long-term steroids, you should be assessed.




Darren McGuff
Man, I’ve seen this play out in my clinic for years. DEXA scans lie. I had a 52-year-old with type 1 diabetes, T-score of -1.2, no fractures - then she dropped a coffee mug and snapped her wrist. FRAX flagged her at 5.1% hip risk. We started alendronate. Two years later, repeat DEXA didn’t change much, but TBS showed massive texture degradation. She hasn’t had another fracture since. Bone quality isn’t just a buzzword - it’s the silent killer.
Ashley Kronenwetter
While the clinical utility of FRAX and bisphosphonates in endocrine-related osteoporosis is well-documented, it is imperative to acknowledge the limitations of population-based algorithms when applied to heterogeneous patient populations. The generalization of treatment thresholds may not account for comorbidities such as chronic kidney disease, which significantly alters pharmacokinetics and bone remodeling dynamics.
Heather Wilson
Let’s be real - FRAX is a glorified spreadsheet. It doesn’t know if your patient is sedentary, has vitamin D deficiency, or takes metformin that messes with bone turnover. And bisphosphonates? Sure, they work - until you get the jaw necrosis or the femur shatters like a cheap phone screen. But hey, at least the pharma reps are happy. Meanwhile, real patients are left wondering why their ‘normal’ scan didn’t save them.
Micheal Murdoch
This is one of those topics where medicine feels like it’s playing catch-up with biology. We treat bone density like it’s a number on a scale, but bone is alive - it talks, it adapts, it remembers trauma. Endocrine diseases don’t just lower your T-score; they poison the soil your bones grow in. FRAX is a start, but it’s like using a flashlight to map a cave. TBS helps, sure - but what we really need is a way to measure bone resilience, not just density. Maybe someday we’ll track collagen cross-links or microdamage accumulation in real time. Until then? Trust the numbers, but never stop listening to the patient.
Jeffrey Hu
Everyone’s obsessed with FRAX, but no one talks about how it’s built on Western, white, elderly populations. What about younger South Asian men with hypogonadism? Or Black women with PCOS? The BMI cutoffs? The alcohol units? All based on data that doesn’t reflect global reality. And bisphosphonates? I’ve seen patients on them for 8 years - no drug holiday, no reassessment. That’s not medicine, that’s autopilot.
Drew Pearlman
I just want to say - if you’re reading this and you have diabetes or thyroid issues - please don’t wait until you break something. I was 48, thought I was fine, ignored my endo’s advice. Then I slipped on ice, landed wrong, and shattered my hip. Surgery, rehab, months of pain. My FRAX score was 4.8%. I was ‘borderline.’ But I broke anyway. Now I’m on zoledronic acid every year. It’s not glamorous, but it’s keeping me standing. Don’t be like me. Ask for the scan. Ask for the FRAX. Ask for TBS. Your future self will thank you.
Chris Kauwe
The entire osteoporosis industrial complex is a scam. FRAX is a bureaucratic tool designed to justify drug sales. Bisphosphonates? They’re just chemical bone suppressors. Real bone health comes from movement, sunlight, and ancestral nutrition - not pills pushed by Big Pharma. We’ve replaced wisdom with algorithms. We’ve replaced strength with scans. And now we’re medicating healthy people into fragility. Wake up. Your bones don’t need a calculator. They need gravity.
RAJAT KD
FRAX underestimates risk in type 1 diabetes? Of course. It doesn’t factor in glycemic variability or advanced glycation end-products. But we still use it because it’s the best we have. DEXA + TBS + clinical history is the real triad. Bisphosphonates work. Don’t let fear of rare side effects stop you from preventing a hip fracture. One fracture changes everything.
Matthew Maxwell
It’s tragic that so many physicians are now outsourcing clinical judgment to algorithms. FRAX was never meant to be a diagnostic tool - yet here we are, prescribing drugs based on a web calculator. And bisphosphonates? They’re the pharmaceutical equivalent of duct tape - temporary, masking the real problem: hormonal dysfunction. Fix the endocrine disorder, not just the bone. That’s medicine. This? This is damage control with a prescription pad.
Lindsey Wellmann
Okay but imagine if your bones were a person 🫠 they’d be like ‘hey i’ve been screaming for help since my thyroid went rogue and you just gave me a scan and said ‘eh, you’re fine’ 😭 i’m not a number bro. i’m collagen and calcium and trauma and i need you to SEE me. 🫂💔 #bonehealthismental #fraxisnotenough #tbsislife
Ian Long
There’s a middle ground here. FRAX isn’t perfect, but it’s better than ignoring risk. Bisphosphonates aren’t magic, but they’re proven. The real issue? Access. Not everyone can get a TBS scan. Not everyone has an endocrinologist who knows how to interpret it. We need guidelines that don’t assume everyone lives near a university hospital. Maybe we start with DEXA + FRAX for all high-risk endocrine patients, then escalate to TBS if resources allow. Progress, not perfection.
Pooja Kumari
I’ve been living with hypothyroidism for 15 years. I had two stress fractures before I was 40. No one ever connected the dots. My doctor said ‘you’re young, you’re active, your bones are fine.’ But I felt it - the aches, the fatigue, the way my spine felt like it was crumbling. When I finally got a DEXA, my T-score was -2.1. FRAX said 18% major fracture risk. I cried. Not because I was scared of the drug - but because I realized I’d been ignored for over a decade. Now I take alendronate. I’m not cured. But I’m not falling apart anymore. If you’re out there feeling this - don’t wait. Push. Keep pushing. Your bones are worth it.
Jacob Paterson
Oh wow, another ‘FRAX saves lives’ sermon. Let me guess - you also think DEXA is the Bible and bisphosphonates are holy water. Newsflash: we’ve been overmedicating low-risk people for decades. The 3% hip fracture threshold? That’s not medicine, that’s fear-based billing. Most people who hit that number will never fracture. But we give them drugs anyway. And then we blame them when they get jaw necrosis. Wake up. This isn’t prevention. It’s profit-driven overdiagnosis.