Triptan Safety Checker
Check Your Safety
This tool helps you identify dangerous interactions with triptans based on your medications and health conditions. Always consult your doctor before taking new medications.
Results will appear here after checking
Please fill out the form to check your safety status
When a migraine hits, time matters. The sooner you treat it, the better your chances of stopping it in its tracks. That’s why triptans are often the first prescription doctors reach for - they work fast, they’re targeted, and for many people, they’re the only thing that brings real relief. But triptans aren’t magic pills. They come with serious rules, hidden risks, and tricky interactions that can turn a helpful treatment into a dangerous one if you don’t know what you’re doing.
What Triptans Actually Do
Triptans aren’t just painkillers. They’re designed to reverse the biological chaos behind a migraine. When a migraine attacks, blood vessels in your brain swell, and nerves around them release chemicals like CGRP and substance P, which amplify pain signals. Triptans shut this down by activating 5-HT1B and 5-HT1D receptors. The 5-HT1B receptors tighten those swollen blood vessels. The 5-HT1D receptors silence the pain-signaling nerves. It’s like flipping two switches at once - one to calm the blood flow, one to mute the noise.
There are seven FDA-approved triptans: sumatriptan, rizatriptan, zolmitriptan, naratriptan, frovatriptan, eletriptan, and almotriptan. Each has a slightly different profile. Rizatriptan hits fast - up to 45% of the dose gets into your bloodstream. Sumatriptan? Only 15%. Frovatriptan sticks around for over 24 hours, which helps if your migraine keeps coming back. Eletriptan has the highest success rate at two hours - 75% of people report headache relief. But none of them work the same for everyone.
The Big Red Flags: When Triptans Are Dangerous
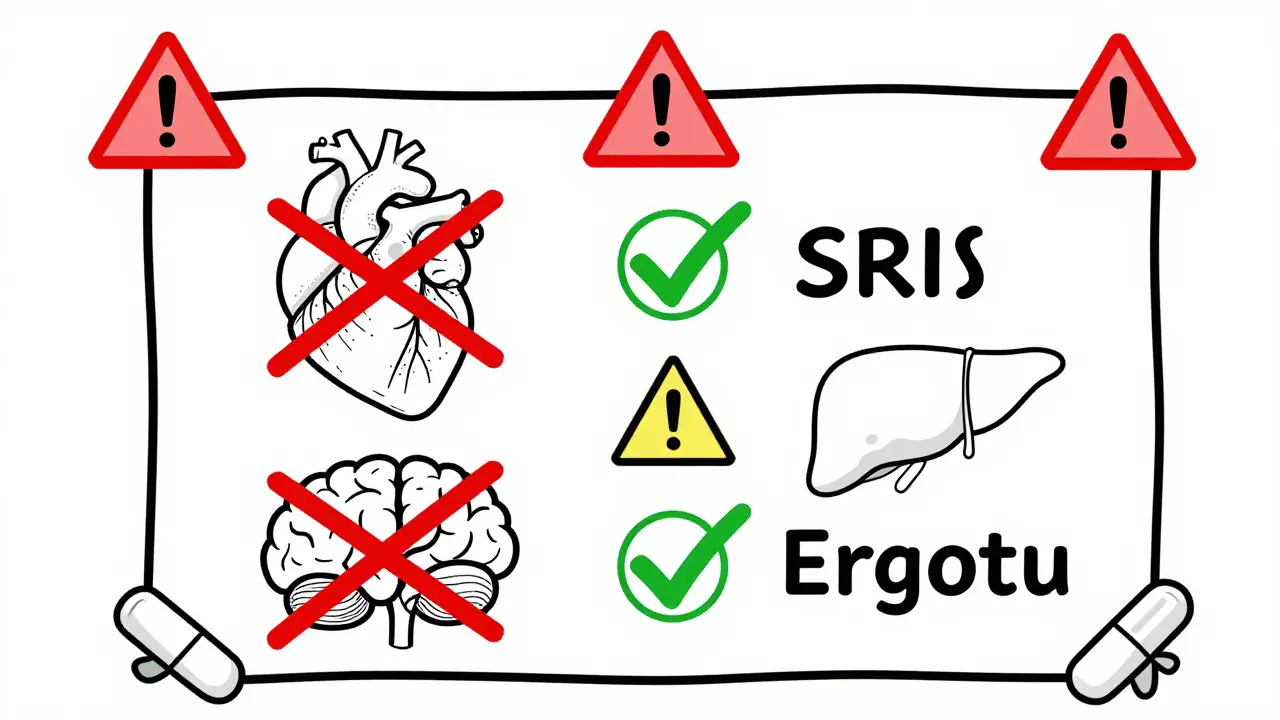
Triptans constrict blood vessels. That’s how they help migraines. But if you already have heart disease, high blood pressure, or a history of stroke, that constriction can trigger a heart attack or stroke. That’s why they’re absolutely off-limits if you have:
- Coronary artery disease
- History of heart attack or angina
- Cerebrovascular disease (like TIA or stroke)
- Peripheral artery disease
- Uncontrolled high blood pressure
- Severe liver damage
Even if you’ve never had symptoms, if you’re over 40 and have risk factors like smoking, diabetes, or high cholesterol, your doctor should screen you before prescribing a triptan. One study found that for every 10,000 people taking sumatriptan for a year, about 0.08 had a heart attack linked to the drug. That’s rare - but it’s not zero.
Drug Interactions You Can’t Ignore
The biggest interaction risk comes from other drugs that raise serotonin levels. That includes SSRIs like sertraline (Zoloft), fluoxetine (Prozac), and SNRIs like venlafaxine (Effexor). Both classes are common for depression and anxiety - conditions that often go hand-in-hand with migraines.
Combining these with triptans can, in rare cases, lead to serotonin syndrome. It’s not common - only a handful of confirmed cases exist - but it’s serious. Symptoms include confusion, rapid heart rate, high blood pressure, muscle rigidity, fever, and seizures. If you’re on an SSRI or SNRI and your migraine suddenly turns into a medical emergency after taking a triptan, get help immediately.
Another risky combo is with ergotamines (like Cafergot). Both cause vasoconstriction. Taking them together can tighten blood vessels too much, risking tissue damage or heart problems. Even over-the-counter cold medicines with pseudoephedrine can raise blood pressure and should be avoided.
Why Triptans Sometimes Just Don’t Work
One in three people with migraines don’t get relief from any triptan. And for 1 in 5, none of the seven options help at all. Why? Migraine isn’t one disease - it’s a spectrum. Genetics play a role. Some people’s nerves just don’t respond to 5-HT1D receptor activation the way others do.
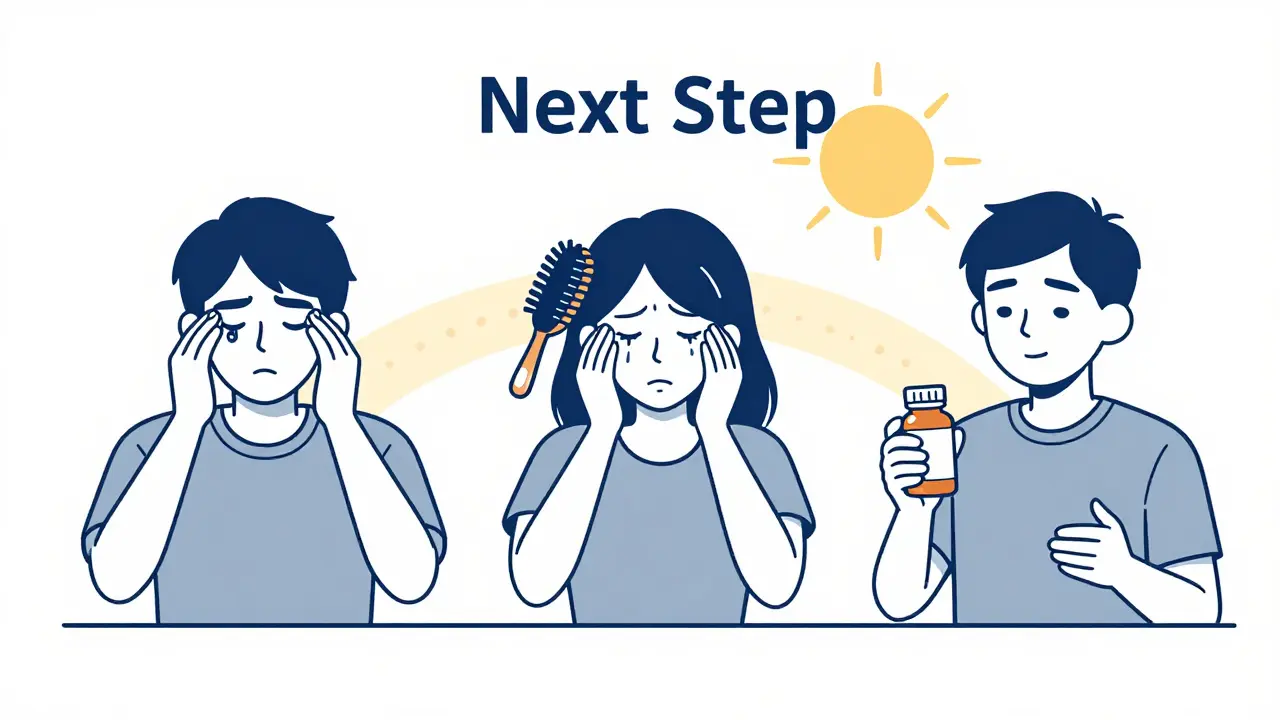
Timing matters more than you think. If you wait until the pain is at its peak, triptans lose power. The sweet spot is within 20 minutes of headache onset - before the pain fully locks in. Taking one during the aura phase? That’s a mistake. Blood vessels are already constricted then. Adding a vasoconstrictor can make neurological symptoms worse.
And then there’s allodynia - when your skin becomes painfully sensitive. If brushing your hair or wearing a shirt hurts, your migraine has progressed. Triptans work well in early-stage migraines - about 70-80% effective. But if allodynia is present? That drops to 30-40%. The nerves are too far gone. At that point, you might need something else - like a ditan (lasmiditan) or a gepant (ubrogepant) - which don’t constrict blood vessels at all.
Side Effects You’ll Likely Feel
Even if triptans work, you’ll probably feel something. About 5-7% of people get chest or throat tightness - it’s not a heart attack, but it feels like one. That’s because the drug affects receptors in the heart and throat. It’s temporary, harmless, and goes away in minutes. Still, it scares people. That’s why some stop taking them.
Dizziness? Common. Fatigue? Happens. Nausea? Especially with sumatriptan. These aren’t rare. Up to 10% report dizziness. Around 8% feel drained. Most people tolerate them fine, but if side effects are constant, it’s worth trying another triptan. Rizatriptan and zolmitriptan tend to cause fewer side effects than sumatriptan.
Rebound Headaches and Overuse
Using triptans too often turns them from heroes into villains. If you take them on 10 or more days a month, you risk medication-overuse headache. It’s a vicious cycle: you take a triptan, it helps, but then the rebound pain hits, so you take another. Soon, you’re having headaches every day.
Guidelines say: no more than two doses per day, and no more than 10 days a month. That’s not a suggestion - it’s a safety limit. If you’re hitting that ceiling, it’s time to talk about preventive treatments - beta-blockers, CGRP monoclonal antibodies, or even neuromodulation devices.
What to Do If One Triptan Fails
Don’t give up after one try. About 30-40% of people who don’t respond to one triptan respond to another. Why? Each has a slightly different shape, half-life, and receptor preference. If sumatriptan didn’t work, try rizatriptan - it’s faster and better absorbed. If naratriptan left you tired all day, try almotriptan - it’s gentler. If you need longer protection, frovatriptan lasts nearly a day.
Some people benefit from combining a triptan with an NSAID. The combo of sumatriptan 85mg and naproxen 500mg gives you a 27% chance of being pain-free in two hours - better than either drug alone. That’s why some doctors prescribe them together, especially for longer or more severe attacks.
The Future Is Here - But Triptans Still Lead
Newer drugs like gepants and ditans are changing the game. They don’t constrict blood vessels, so they’re safe for people with heart disease. They’re also less likely to cause rebound headaches. But they’re expensive. Most insurance still makes you try triptans first.
And here’s the truth: triptans have been used in over 300 million prescriptions since 1991. That’s not because they’re perfect. It’s because they’re proven. For most people without heart issues, they still work better than anything else. The key isn’t avoiding them - it’s using them right. Know your limits. Watch for red flags. Time your dose. And if one doesn’t work, try another. You might be one switch away from relief.
Can I take a triptan if I’m on an SSRI for depression?
Yes, but with caution. While the risk of serotonin syndrome is low, it’s real. Your doctor should monitor you closely, especially when starting or changing doses. Never combine triptans with MAOIs - those are dangerous. If you notice confusion, rapid heartbeat, muscle stiffness, or high fever after taking both, seek emergency help immediately.
Why does my migraine come back after a triptan works?
This is called migraine recurrence, and it affects 15-40% of users, depending on the triptan. Short-acting triptans like sumatriptan (2-hour half-life) are more likely to wear off before the attack fully ends. Longer-acting ones like frovatriptan (26-hour half-life) reduce recurrence. If this happens often, your doctor might suggest a second dose after two hours - but never more than two doses in 24 hours.
Is it safe to take triptans if I have high blood pressure?
Only if your blood pressure is well-controlled. If your systolic pressure is above 140 or diastolic above 90, triptans are not recommended. They can raise blood pressure further, increasing stroke risk. Always check your BP before taking one. If you’re unsure, ask your doctor for a simple test before your next prescription.
What’s the best time to take a triptan?
As soon as the headache starts - not during aura. If you wait until the pain is throbbing, the drug may not work as well. For best results, take it within 20 minutes of pain onset. If you have aura, wait until the visual or sensory symptoms fade and the headache begins. Taking it too early can worsen neurological symptoms.
Can I take a triptan every day if my migraines are frequent?
No. Triptans are for acute attacks only. Using them more than 10 days a month can cause medication-overuse headaches - where your headaches become daily and harder to treat. If you’re having migraines 10+ days a month, you need preventive treatment, not more triptans. Talk to your doctor about daily options like beta-blockers, topiramate, or CGRP blockers.




Eli Kiseop
Been on sumatriptan for years and it works like magic until it doesnt
One time I took it during aura and my vision got weirder not better
Now I wait till the headache hits hard and even then sometimes it just sits there like a lump
Ellie Norris
ohhh i didnt know frovatriptan lasts 24hrs 😅 i’ve been takin rizatriptan and wonderin why my migraines keep comin back
gonna ask my doc bout switchin, thx for the tip!!
Akhona Myeki
Let me be perfectly clear - this entire post is dangerously oversimplified. In South Africa, we have access to triptans only through private clinics and even then, doctors are terrified to prescribe them. The notion that 'one in three don't respond' is a Western privilege. Most of us can't even get ibuprofen reliably. You speak of gepants like they're accessible - they cost more than a month's rent here. This isn't a medical discussion. It's a luxury debate.
Chinmoy Kumar
so i tried sumatriptan and got that chest tightness thing and thought i was havin a heart attack 😅
turned out it was just the med
then i tried rizatriptan and no chest thing at all
weird how one body reacts so diff to similar drugs
also i take it with naproxen now and wow what a difference
maybe try combo before giving up on triptans?
Brett MacDonald
so like... if triptans constrict blood vessels and migraines are about blood vessels... isn't that just like fighting fire with fire?
what if the real problem is the brain's interpretation of pain and we're just bandaging the symptom?
also why do we call it a 'migraine' anyway? sounds like a bad sci-fi movie title
Sandeep Kumar
Americans think they invented medicine
in India we've been treating migraines with ginger, turmeric and silence for centuries
you take a pill for everything now
your brain is just a broken machine to you
no wonder you all have migraines
go sit under a tree and breathe
Solomon Ahonsi
so you're telling me the entire pharmaceutical industry built a billion-dollar market on a drug that gives you chest tightness and can kill you if you're over 40 and breathe air?
and we're supposed to be grateful?
bruh. i'm just gonna drink coffee and hope for the best.
George Firican
The philosophical tension here lies not in the pharmacology of serotonin receptors but in the human condition’s desperate attempt to externalize suffering through chemical intervention. We have evolved to endure pain as a signal - a messenger - and yet we treat it as an enemy to be eradicated at any cost. Triptans offer temporary silence, but they do not resolve the underlying dissonance between our nervous systems and the modern world’s relentless stimuli. Perhaps the real question isn’t whether triptans work, but why we’ve allowed our lives to become so unbearable that we require vasoconstrictors just to function. The body is not a machine. It is a conversation. And we keep shouting over its whispers.
Matt W
just wanna say thank you for this post
been sufferin for 12 years and no one ever explained the timing thing
took my triptan during aura once and felt like my brain was being squeezed
now i wait till the headache hits
and i take it with a glass of water and a deep breath
it's not perfect but it's better
you're not alone out there