Why Your Snoring Might Be Quietly Damaging Your Heart
If you or your partner snores loudly, wakes up gasping, or feels exhausted even after eight hours in bed, it’s not just annoying-it could be putting your heart at serious risk. Sleep apnea isn’t just a sleep problem. It’s a silent driver of high blood pressure, heart attacks, strokes, and heart failure. And the worst part? Most people who have it don’t even know.
More than 1 billion people worldwide suffer from sleep apnea, and in the U.S. alone, 40 million adults are affected. Of those, 80% have obstructive sleep apnea (OSA), where the throat muscles relax too much during sleep and block the airway. This isn’t just about poor sleep. Each time you stop breathing, your body goes into survival mode. Oxygen drops. Your heart races. Blood pressure spikes. And it doesn’t stop when you wake up-these episodes repeat dozens or even hundreds of times a night, every night.
The Link Between Sleep Apnea and High Blood Pressure
High blood pressure is the most common and best-documented heart problem tied to sleep apnea. In fact, up to 80% of people with resistant hypertension-meaning their blood pressure stays high despite taking three or more medications-also have undiagnosed sleep apnea.
Here’s how it works: When your airway collapses, your oxygen levels plummet. Your brain senses the danger and floods your body with stress hormones like adrenaline. This forces your blood vessels to tighten and your heart to pump harder. Over time, this constant surge rewires your nervous system. Even when you’re awake and breathing normally, your blood pressure stays elevated.
What makes this even more dangerous is the pattern. Most people’s blood pressure naturally drops 10-20% at night. But in people with sleep apnea, 70-80% don’t experience this dip. Instead, their pressure stays high or even rises overnight. This is called a "non-dipping" pattern-and it’s a red flag for future heart attacks and strokes.
Studies show that people with moderate to severe sleep apnea are two to three times more likely to develop high blood pressure within just four to five years. And it’s not just older adults. A 2024 study found that adults under 40 with untreated sleep apnea had a 45% higher chance of developing high blood pressure compared to peers without it. That’s not aging-it’s acceleration.
How Sleep Apnea Fuels Heart Disease
High blood pressure is just the start. Sleep apnea directly damages your heart in multiple ways.
Every time your airway closes, your chest creates a strong vacuum as you struggle to breathe. This pulls extra pressure onto your heart, forcing it to work harder just to pump blood. That stress, repeated hundreds of times a night, thickens the heart muscle, especially the left ventricle. Over time, this leads to heart failure.
People with moderate to severe sleep apnea have a 140% higher risk of developing heart failure. And once heart failure is present, sleep apnea makes it worse. About half of all heart failure patients also have sleep apnea, creating a vicious cycle: weak heart → poor oxygen delivery → more breathing pauses → more strain on the heart.
Coronary artery disease-the buildup of plaque in heart arteries-is also strongly linked. Those with moderate to severe sleep apnea are 30% more likely to develop heart disease and 60% more likely to have a fatal heart attack. And here’s something chilling: 26.5% of heart attacks in people with sleep apnea happen between midnight and 6 a.m. That’s when breathing pauses are most frequent and blood pressure spikes are highest.
Stroke Risk Skyrockets With Untreated Sleep Apnea
Stroke is another major threat. Sleep apnea doesn’t just raise your risk-it multiplies it. People with OSA are 2.5 times more likely to have a first stroke. If you’ve already had one, your chance of having another jumps to 3.2 times higher.
The severity of oxygen drops during sleep matters too. If your blood oxygen level falls below 90% for more than 12% of your sleep time, your risk of dying from a stroke increases by 4.3 times. That’s not a small risk-it’s a medical emergency waiting to happen.
Why? Repeated low oxygen triggers inflammation, damages blood vessel lining, and makes blood more likely to clot. All of this sets the stage for a stroke. And because these events often happen at night, many go unnoticed until it’s too late.
Arrhythmias: When Your Heart Goes Off-Rhythm
One of the most overlooked consequences of sleep apnea is irregular heartbeats, especially atrial fibrillation (AFib). People with sleep apnea are 2 to 4 times more likely to develop AFib. In fact, nearly 50% of people with paroxysmal AFib-the kind that comes and goes-also have undiagnosed sleep apnea.
This isn’t just a coincidence. The same stress hormones, oxygen drops, and pressure swings that cause high blood pressure also mess with the heart’s electrical system. And here’s the kicker: if you have AFib and don’t treat your sleep apnea, your chances of the ablation procedure working drop by 30%. Your heart rhythm therapy won’t work if the root cause-sleep apnea-is still active.
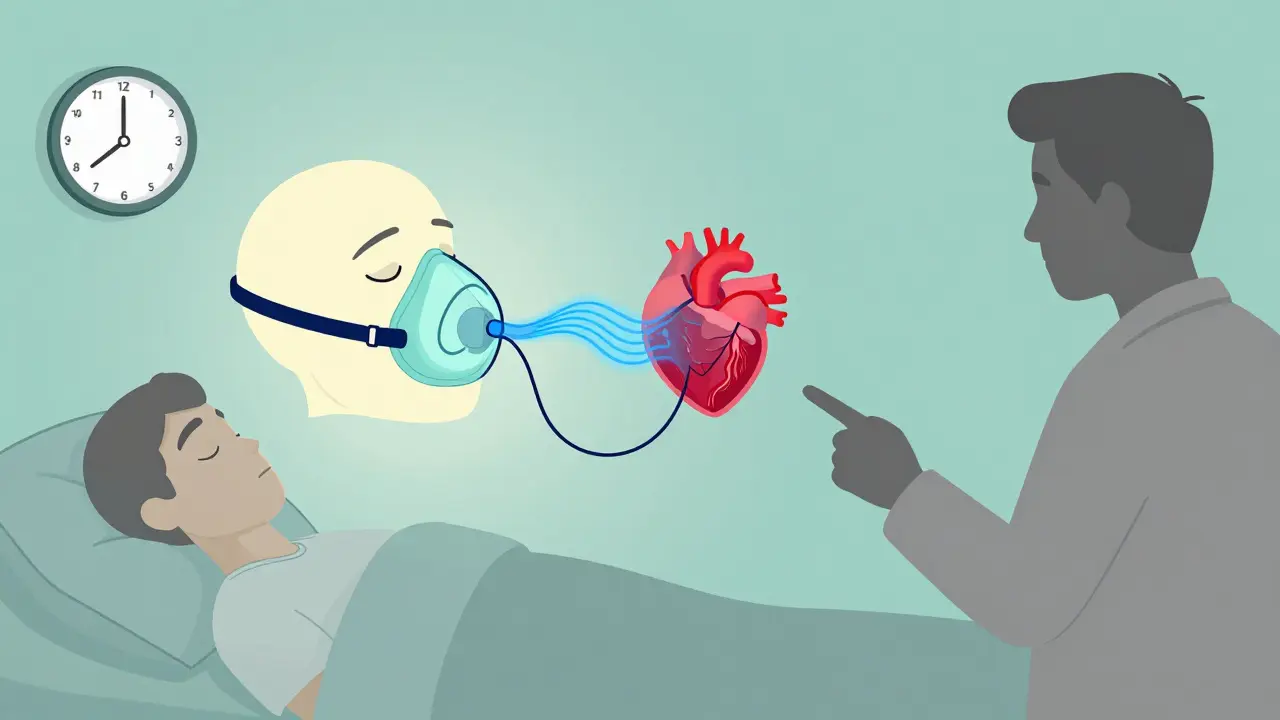
Why CPAP Isn’t a Magic Bullet (But It’s Still Essential)
You’ve probably heard that continuous positive airway pressure (CPAP) machines fix sleep apnea. And they do-but not always the way people expect.
CPAP doesn’t dramatically lower blood pressure in most people. Studies show an average drop of just 2-3 mmHg. That’s not nothing, but it’s not a cure. So why bother?
Because CPAP doesn’t just lower numbers-it saves lives. In people who’ve had a stroke, consistent CPAP use cuts the risk of another stroke by 37%. In heart failure patients with central sleep apnea, it improves survival and reduces hospital stays. It also makes heart rhythm treatments more effective.
The problem? Only 46% of people use their CPAP machine enough to get real benefits-meaning at least 4 hours a night, 70% of nights. Many quit because it feels uncomfortable, noisy, or claustrophobic. But the alternative-ignoring your sleep apnea-is far worse.
Who Should Be Screened-and How
If you have any of these, you should be tested for sleep apnea:
- High blood pressure, especially if it’s hard to control
- Heart failure or coronary artery disease
- Atrial fibrillation or other arrhythmias
- Stroke or transient ischemic attack (mini-stroke)
- Loud snoring, daytime sleepiness, or waking up gasping
- Obesity, especially with a neck circumference over 17 inches (men) or 16 inches (women)
Doctors can use a simple tool called the STOP-Bang questionnaire. It asks about snoring, tiredness, observed breathing pauses, high blood pressure, BMI, age, neck size, and gender. It’s not perfect-but it catches 84% of moderate to severe cases.
Home sleep tests are widely available and accurate for moderate to severe apnea. But if your results are normal and you still have symptoms, you may need a full overnight sleep study in a lab. Don’t give up if the first test doesn’t show anything.
The Bottom Line: Your Heart Can’t Wait
Sleep apnea isn’t a lifestyle issue. It’s a cardiovascular disease. It’s not just about feeling tired. It’s about your heart being under constant attack while you sleep.
And the good news? Treating it works. Even small improvements in breathing at night reduce inflammation, lower stress hormones, and protect your arteries. If you’ve been told you snore, or you’re struggling with high blood pressure, heart disease, or irregular heartbeat-ask your doctor about sleep apnea. Don’t wait for a heart attack or stroke to make you listen.
The data is clear: one in five adults has moderate to severe sleep apnea. And the number is rising 5% every year, fueled by obesity. This isn’t a niche problem. It’s a public health crisis hiding in plain sight-right in your bedroom.
Can sleep apnea cause high blood pressure even if I’m not overweight?
Yes. While obesity is the biggest risk factor-responsible for 70% of cases-sleep apnea can happen in thin people too. Factors like jaw structure, enlarged tonsils, nasal congestion, or family history can cause airway collapse. The mechanism-low oxygen, stress hormones, and pressure swings-is the same. So even if you’re not overweight, loud snoring or daytime fatigue should be checked.
If I use a CPAP machine, will my blood pressure go back to normal?
CPAP often helps, but it rarely normalizes blood pressure on its own, especially if you’ve had high blood pressure for years. Most people see a small drop-around 2-3 mmHg. But that’s not the whole story. CPAP reduces nighttime spikes, improves heart function, and lowers your long-term risk of heart attack and stroke. For many, it makes blood pressure medications work better. Think of it as removing the constant stress on your heart, not just lowering a number.
Is there a connection between sleep apnea and diabetes?
Yes. Repeated oxygen drops and stress hormones from sleep apnea interfere with insulin sensitivity. Studies show people with untreated sleep apnea have a 30-40% higher risk of developing type 2 diabetes. Even if you’re not diabetic, sleep apnea can make blood sugar harder to control. Treating apnea often improves insulin response and reduces HbA1c levels.
Can I treat sleep apnea without a CPAP machine?
Yes, depending on severity. For mild cases, weight loss, sleeping on your side, or avoiding alcohol before bed can help. Oral appliances that reposition the jaw are effective for some people. Surgery is an option if there’s a clear anatomical blockage, like enlarged tonsils. But for moderate to severe apnea, CPAP remains the most reliable treatment. Newer alternatives like hypoglossal nerve stimulators are available for select patients, but they’re not for everyone.
Should I get tested for sleep apnea if I have heart failure?
Absolutely. Between 40% and 60% of heart failure patients also have sleep apnea-and many don’t know it. Left untreated, it worsens heart function, increases hospital visits, and raises death risk. If you have heart failure and feel excessively tired, wake up short of breath, or snore loudly, ask your cardiologist for a sleep evaluation. Treating the apnea can improve your energy, reduce fluid buildup, and help your heart respond better to medications.
What to Do Next
If you’re at risk-whether because of snoring, high blood pressure, or heart trouble-don’t wait. Talk to your doctor. Ask for a sleep apnea screening. If you’ve been diagnosed but aren’t using your CPAP consistently, reach out to your sleep clinic. There are new masks, humidifiers, and support programs designed to make compliance easier.
Your heart doesn’t get a break at night. Don’t let sleep apnea steal yours either.





Brittany Wallace
I used to think snoring was just annoying... until my partner started gasping in his sleep. Now I keep a sleep tracker by the bed. Turns out he’s got moderate OSA. We started CPAP last year. He’s not just less tired-he’s present. Like, actually laughs at memes again. 🌙❤️
Palesa Makuru
Honestly? This post is so basic. Everyone knows sleep apnea is bad. But nobody talks about how the medical-industrial complex profits off CPAP rentals and $2000 masks while ignoring cheaper solutions like positional therapy or tongue-strengthening exercises. 🙄
Lori Jackson
The pathophysiological cascade is undeniable: hypoxic stress → sympathetic overdrive → endothelial dysfunction → systemic inflammation → atherogenesis. The data is robust. What’s lacking is population-level screening protocols. We’re treating symptoms, not root causes. This is preventive medicine 101-and we’re failing.
Wren Hamley
I’m a paramedic. Last month, we pulled a 38-year-old guy out of cardiac arrest at 3 a.m. He snored like a chainsaw. No history of hypertension. No diabetes. Just ‘tired all the time.’ He didn’t even know he stopped breathing. I’ve seen this too many times. If you snore louder than your dog barks-get checked. Seriously.
Sarah Little
I read the 2024 JAMA study on under-40 hypertension and OSA. The HR was 1.45. CI 1.22–1.72. P<0.001. But here’s the kicker-only 12% of primary care docs screen for it. Why? Time. Reimbursement. Lack of training. We’re not failing patients. The system is broken.
innocent massawe
In my village back home, people say snoring is just the spirit checking if you’re still breathing. 😅 But my cousin had a stroke at 41. He never snored loud... just woke up sweating and confused. Now he uses CPAP. He says it’s like his brain finally got a night off.
Tru Vista
CPAP is a joke. 46% compliance? Of course. Who wants to sleep with a mask that sounds like a jet engine? Try a mouthpiece. Or just sleep on your side. Duh.
Vincent Sunio
The author exhibits a concerning conflation of correlation with causation. While epidemiological associations exist, the causal mechanism remains incompletely elucidated. Moreover, the recommendation for universal screening lacks cost-benefit analysis. One must not mistake alarmism for evidence.
Shanahan Crowell
You’re not lazy. You’re not broken. You’re just breathing wrong at night. And guess what? You can fix it. CPAP isn’t punishment-it’s permission. Permission to wake up alive. Permission to be present for your kids. Permission to live longer than your parents did. Start tonight. You’ve got this.
Kerry Howarth
If you have high blood pressure and snore-get tested. No excuses. It’s that simple. Your heart doesn’t care if you’re ‘too busy.’
Haley Parizo
This isn’t just a health issue-it’s a class issue. The people who need CPAP the most can’t afford it. Insurance won’t cover it. The system is rigged to keep the poor tired and the rich healthy. Wake up. This is structural violence.