Ever opened a prescription bottle and stared at the tiny print, wondering what "take with food" really means? You’re not alone. Nearly half of all patients misinterpret these critical instructions - and the consequences can be serious. A single misunderstood line like "take on empty stomach" or "shake well before use" can lead to side effects, reduced effectiveness, or even hospital visits. These aren’t just suggestions. They’re life-saving directions written into your medication’s label for a reason.
What Are Special Instructions, Really?
Special instructions on prescription labels go beyond "take one pill daily." They tell you how to take the medicine so it works right and doesn’t hurt you. Think of them as the fine print that actually matters.
Examples include:
- Take with food
- Take on an empty stomach
- Shake well before use
- Refrigerate
- Do not crush or chew
- Avoid sunlight
- Take every 12 hours
- Discard after 14 days
These aren’t random. Each one is based on how the drug behaves in your body. For instance, some medications irritate your stomach if taken without food. Others break down too fast if eaten right after. Some lose potency if left out of the fridge. And crushing a time-release pill can dump its entire dose into your system at once - which can be dangerous.
On average, a prescription label has 3.7 special instructions. Compare that to over-the-counter labels, which average just 1.2. That’s because prescription drugs are stronger, more complex, and carry higher risks.
Where Do You Find These Instructions?
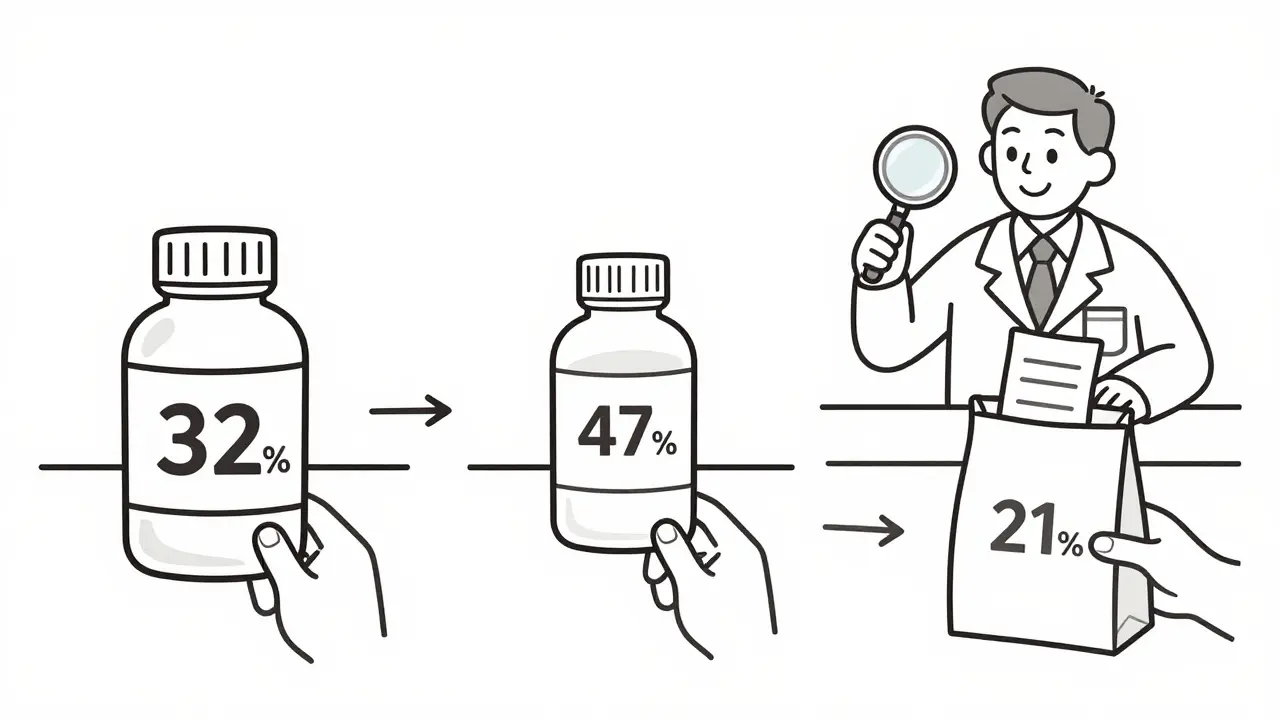
They’re not always where you expect. Pharmacists put special instructions in three places:
- Directly on the bottle label (32% of cases)
- On a small sticker stuck to the bottle (47%)
- In a separate paper insert (21%)
That’s why it’s so easy to miss them. You read the main label, think you’re done, and never check the sticker or the folded paper tucked in the bag. A 2022 Consumer Reports survey found that 54% of people had trouble locating these instructions - and 31% missed critical ones entirely.
And here’s something most people don’t know: the FDA requires these instructions to be printed in at least 10-point font with high contrast against the background. If you can’t read them easily, ask for a large-print version. Nearly all U.S. pharmacies offer this for free.
Why Do People Keep Misunderstanding Them?
It’s not that people are careless. It’s that the language is confusing - even when it’s clear.
Take "take with food." A 2021 Harvard Health study showed:
- 41% think it means "with the first bite of food"
- 33% believe it means "during the meal"
- 26% understand it as "within 30 minutes of eating"
Only one of those is correct - and it depends on the drug. Some need food to be absorbed. Others need food to avoid nausea. The wording doesn’t change, but the meaning does.
Timing is another big issue. "Take every 12 hours" sounds simple. But 53% of patients take doses too close together, thinking "morning and night" means 8 a.m. and 8 p.m. That’s only 12 hours if you’re awake the whole time. If you sleep from 11 p.m. to 7 a.m., you’re actually spacing doses 16 hours apart - which makes the medicine less effective.
And it’s worse for people with low health literacy. In the U.S., 36% of adults have basic or below-basic health literacy. Among them, 62% misinterpret special instructions - compared to just 28% of those with higher literacy. Spanish-speaking patients are 3.2 times more likely to misunderstand "take with food" than English speakers.
What Happens When Instructions Are Ignored?
The cost isn’t just personal - it’s financial and systemic.
Medication errors linked to poor label understanding cost the U.S. healthcare system $42 billion a year. About 43% of the 12,450 medication complaints filed with Medicare in 2023 were tied to misreading instructions. That led to an estimated $1.2 billion in preventable hospital stays.
Patients who misunderstood "take on empty stomach" were more likely to have stomach bleeding or nausea. Those who didn’t shake liquid antibiotics ended up with uneven doses - some too strong, some too weak. People who crushed pills meant to be swallowed whole had dangerous spikes in blood levels.
But here’s the good news: when patients understand these instructions correctly, medication errors drop by 38%. That’s not a small number. That’s thousands of avoidable ER trips, missed workdays, and complications.
How to Make Sure You Get It Right
You don’t have to guess. Here’s how to make sure you’re taking your meds safely:
- Check all three places. Look at the bottle, the sticker, and the paper insert. Don’t stop at the first thing you see.
- Ask your pharmacist to explain it. Don’t say "I think I know what this means." Say "Can you tell me exactly what this means for me?" Pharmacists are trained to spot confusion. In fact, 89% of positive pharmacy reviews mention this kind of help.
- Clarify vague terms. "With food" - what counts? A snack? A full meal? A glass of milk? Ask. "On an empty stomach" - how long before or after eating? Get specifics.
- Use tools. Medication reminder apps help 62% of users stay on schedule. Pill organizers with time compartments cut timing errors by 47%. Large-print labels are free and available at 94% of pharmacies.
- Write it down. If the instruction is "take every 12 hours," write "8 a.m. and 8 p.m." on your calendar - even if you think you’ll remember.
The Dana-Farber Cancer Institute recommends a simple 3-step process: Find it. Clarify it. Remember it. That’s it.

What’s Changing on Prescription Labels?
The system is slowly getting better.
The FDA launched its Enhanced Medication Labeling Initiative in 2021, pushing for clearer wording on high-risk drugs. In August 2023, they proposed a rule to standardize 12 key instructions across all prescriptions by 2026. That means "take with food" will mean the same thing on every drug.
Some pharmacies are testing AI-driven labels that adjust wording based on your literacy level. Others are piloting augmented reality labels - scan the bottle with your phone, and a video plays showing exactly how to take it.
And now, doctors can bill for a 5-minute session just to explain medication instructions. The new CPT code 99444 pays $27.63 per session. That’s a sign: the system finally recognizes that this isn’t just a label issue - it’s a communication problem.
Still, experts warn: without fixing health literacy across the board, even the clearest label won’t fix everything. Dr. David Bates from Harvard says label improvements alone will only solve 40% of the problem.
Bottom Line: Your Label Is Your Lifeline
Prescription labels aren’t just paperwork. They’re your safety net. Every instruction exists because someone got hurt - or worse - before it was added.
You don’t need to be a scientist to understand them. You just need to ask. Take five minutes. Look at the sticker. Ask the pharmacist. Write it down. Use your phone. Don’t assume. Don’t guess.
Because when it comes to your medicine, the smallest detail can make the biggest difference.
What does "take with food" actually mean on a prescription label?
It means you should take the medication during or shortly after eating, but the exact timing depends on the drug. Some need food to reduce stomach upset, others need it to absorb properly. Ask your pharmacist whether "with food" means "during the meal," "within 30 minutes," or "with a full meal." Never assume.
Why are special instructions on stickers instead of the main label?
Pharmacies use stickers because labels are printed in bulk before your specific instructions are added. The sticker lets them customize each bottle without reprinting entire labels. But it also means you might miss it. Always check the bottle for any added stickers - they’re often the most important part.
Can I ignore special instructions if I feel fine?
No. Feeling fine doesn’t mean the medicine is working right. Some drugs need specific timing or food to build up in your system. Skipping instructions can make the treatment less effective or cause side effects later. Even if you feel okay, follow the label exactly as written.
What should I do if I miss a dose because I misunderstood the instructions?
Don’t double up. Call your pharmacist or doctor right away. They’ll tell you whether to skip the missed dose, take it now, or wait until the next scheduled time. Never guess - a wrong move can be dangerous, especially with blood thinners, antibiotics, or heart medications.
Are there free tools to help me remember special instructions?
Yes. Most pharmacies offer free pill organizers with time slots. You can also use free apps like Medisafe or MyTherapy that send reminders and let you scan your label to store instructions. Large-print labels are also free at nearly all U.S. pharmacies. Ask for them - you don’t need a special reason.
Why do some prescriptions come with a Medication Guide?
The FDA requires a Medication Guide for about 250 high-risk drugs - like blood thinners, antidepressants, or cancer treatments - where misunderstanding could cause serious harm. These guides explain risks, side effects, and how to take the drug safely. If you get one, read it. It’s not optional. It’s meant for you.
Can I ask my pharmacist to rewrite the label in simpler language?
Absolutely. Pharmacists are trained to explain prescriptions in plain language. If the label uses terms like "q12h" or "NPO," ask them to translate it. You can also ask for a printed version with bullet points or a checklist. No pharmacist will say no - they’re paid to help you get it right.
What if I don’t speak English well?
Most major pharmacies offer translation services - either in person, over the phone, or through printed materials in Spanish, Mandarin, Vietnamese, and other languages. Ask for a bilingual pharmacist or request translated instructions. You have the right to understand your medication - language shouldn’t be a barrier.




Doreen Pachificus
So I just realized I’ve been taking my blood pressure med with a cup of coffee like it’s a morning ritual. Turns out caffeine might be interfering with absorption. Thanks for the wake-up call.
Stephen Craig
Labels aren’t instructions-they’re warnings written by people who’ve seen what happens when you don’t listen.
Charlotte N
why do they put the important stuff on stickers?? like who designed this system?? i mean come on
Ethan Purser
Let me tell you something-pharmacies are profit-driven machines. They don’t care if you understand your meds. They care if you refill them. The sticker? The tiny font? The folded insert? It’s all designed to make you feel like you’re in control while they quietly shift responsibility onto you. You think you’re reading a label? You’re reading a trap. And the FDA? They’re just putting band-aids on a hemorrhage. We need real reform-not more ‘enhanced labeling’ that still leaves you guessing. This isn’t about literacy. It’s about power.
Connor Hale
That 38% drop in errors when people follow instructions? That’s the quiet hero of modern medicine. We don’t hear about it because it’s not a breakthrough-it’s just someone doing what they’re told. But that’s the real win.
Roshan Aryal
USA spends billions on ‘label clarity’ while kids in India swallow antibiotics with chai and survive. You think your pills are special? We don’t need fancy apps or AR labels-we need less bureaucracy and more trust in common sense. Your ‘life-saving instructions’ are just corporate liability wrapped in Helvetica.
Catherine HARDY
Did you know the FDA gets funding from Big Pharma? That’s why the font size is just barely legal. They don’t want you to read it too well. The ‘large-print option’? A placebo. They’ll give you a bigger font but keep the jargon. And the ‘AI-driven labels’? That’s just surveillance with a side of aspirin. They’re tracking what you read. They know if you skipped the sticker. They know you didn’t scan the AR code. This isn’t safety. It’s control.
bob bob
My grandma used to write her med schedule on a sticky note and stick it to the fridge. Best system ever. No apps, no stickers, no confusion. Just ‘take blue pill after breakfast, white one before bed.’ Simple. Human. Works.
Vicki Yuan
It’s not just about reading the label-it’s about understanding the context. The difference between ‘take with food’ and ‘take during a meal’ can be the difference between therapeutic levels and toxicity. Pharmacists aren’t just dispensers; they’re translators. Asking them to clarify isn’t weakness-it’s wisdom.
Uzoamaka Nwankpa
I come from Nigeria where we often share meds with family because the pharmacy is miles away. We don’t have stickers or apps. We have memory. We have trust. We have elders who taught us what ‘take with food’ means by watching their mothers do it. Maybe the answer isn’t more labels-but less distance between people and knowledge.
Jack Wernet
Thank you for this thoughtful, meticulously researched piece. The systemic issues around medication literacy are profound and under-addressed. I particularly appreciate the emphasis on pharmacist engagement and the new CPT code 99444. This represents a meaningful step toward recognizing patient education as a clinical service-not an afterthought. I’ve shared this with my entire care team.