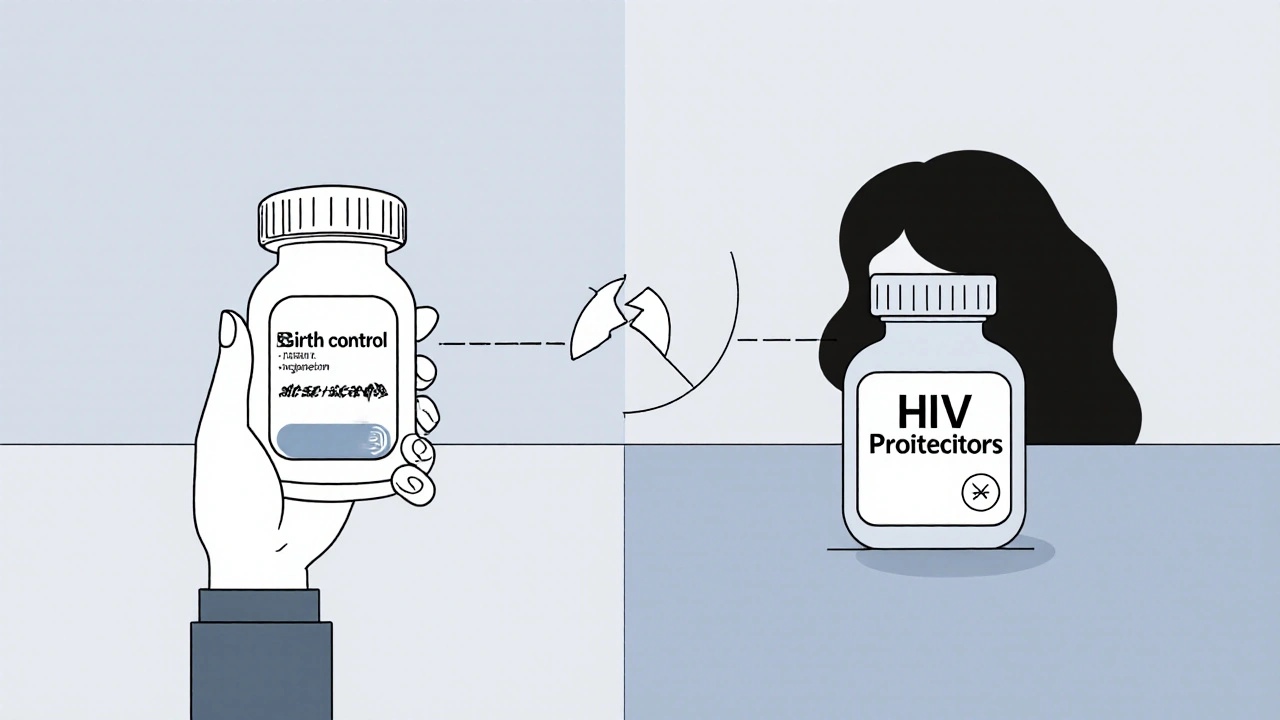
When you're living with HIV and taking antiretroviral drugs, your body is already managing a complex balance. But if you're also using hormonal birth control-pills, patches, rings, or implants-you might be at risk for something no one talks about enough: contraceptive failure. It’s not rare. It’s not theoretical. And it’s not always obvious until it’s too late.
Why HIV Medications Can Break Birth Control
HIV protease inhibitors (PIs), like lopinavir, atazanavir, and darunavir, are powerful drugs. They block the virus from copying itself. But they don’t just target HIV. They also mess with your liver’s ability to process other drugs-especially hormones. Most birth control methods rely on synthetic estrogen and progestin. These hormones are broken down by an enzyme in your liver called CYP3A4. Protease inhibitors, especially when boosted with ritonavir, can either block or overstimulate this enzyme. The result? Your body either clears the hormones too fast-or holds onto them too long-both of which can make birth control ineffective.The Real Numbers: How Much Effectiveness Is Lost?
It’s not just a theory. Studies show real drops in hormone levels. In one 2010 trial, women using the contraceptive patch while taking lopinavir/ritonavir saw a 45% drop in estrogen levels. That’s not a small change-it’s enough to stop ovulation from being suppressed. Another study found that the contraceptive ring, which normally releases steady hormones, dropped to subtherapeutic levels in 38% of women on efavirenz-based regimens. That means nearly 4 out of 10 women using this method were at risk of pregnancy, even though they took their pills or wore their ring exactly as directed. Even more alarming: women on ritonavir-boosted protease inhibitors who used progestin-only pills had pregnancy rates as high as 11-15% per year. Compare that to the typical 7-8% failure rate in HIV-negative women using the same pill. That’s not user error. That’s drug interaction.Not All HIV Drugs Are the Same
This isn’t true for every antiretroviral. The problem is mostly with protease inhibitors, especially when boosted with ritonavir or cobicistat. But other classes have different effects. Efavirenz, an NNRTI, is another major offender-it slashes estrogen levels by up to 60%. Nevirapine? Much milder. And integrase inhibitors like dolutegravir? Nearly no interaction at all. That’s why treatment guidelines have shifted. In 2023, more than 70% of new HIV patients started on dolutegravir-based regimens-not protease inhibitors. Why? Because they’re simpler, more effective against the virus, and far less likely to interfere with birth control. If you’re on an older regimen, it’s worth asking your doctor if switching could improve both your health and your contraceptive safety.What Birth Control Methods Are Safe?
Here’s the bottom line: if you’re on a protease inhibitor, especially ritonavir-boosted, avoid hormonal methods that rely on estrogen or progestin alone. That includes:- Progestin-only pills (the “mini-pill”)
- Combined oral contraceptives (the regular pill)
- The contraceptive patch
- The vaginal ring (NuvaRing)
- Hormonal implants like etonogestrel (Nexplanon)
- Copper IUD-no hormones, 99% effective, lasts up to 12 years.
- Hormonal IUD (like Mirena or Kyleena)-releases progestin locally, so it doesn’t rely on liver metabolism. Safe with all HIV drugs.
- Depo-Provera (DMPA) injection-safe with most regimens, except efavirenz. Even then, pregnancy rates are lower than with pills or rings.
- Permanent methods-tubal ligation or partner vasectomy.
Real Stories Behind the Data
Behind every statistic is a person. MariaJ, from the HIV.gov forum, got pregnant while taking darunavir/cobicistat and Tri-Sprintec. She took her pill every day. No missed doses. No vomiting. But the drug interaction still happened. She wasn’t warned. Another woman, posting on Reddit, used Depo-Provera with atazanavir/ritonavir and didn’t realize she was pregnant until 18 weeks. Her provider said the interaction was “well-documented but often overlooked.” That’s the problem. Many clinics, especially outside major cities, don’t have the training or tools to catch this. A 2021 survey of 327 HIV-positive women found that 28% had experienced contraceptive failure while on antiretrovirals. Over 60% of those cases involved protease inhibitors. And here’s the hardest part: 41% of women said they weren’t properly counseled about this risk when they first started HIV treatment.What Should You Do?
If you’re on HIV meds and using hormonal birth control, here’s what to do now:- Check your regimen. Are you on lopinavir, atazanavir, darunavir, or any drug with “ritonavir” or “cobicistat” in it? If yes, you’re at risk.
- Don’t assume your pill or ring is working. Even perfect use doesn’t guarantee protection.
- Ask your provider for a copper or hormonal IUD. They’re the safest, most reliable option.
- If you can’t get an IUD right away, switch to Depo-Provera (if you’re not on efavirenz) or use condoms consistently as backup.
- Use the CDC’s online drug interaction checker-it’s free and updated quarterly. Input your exact medications and birth control method.

What If You’re Already Pregnant?
If you’re pregnant and on HIV meds, don’t panic. Many women have had healthy pregnancies while on antiretrovirals. But you need to act fast. Tell your HIV provider and OB/GYN right away. Some drugs, like dolutegravir, are now considered safe in early pregnancy. Others, like efavirenz, are avoided in the first trimester. Your treatment plan can and should change to protect both you and your baby.Why This Isn’t Getting Better Faster
The science is clear. The guidelines exist. But access isn’t equal. In sub-Saharan Africa, 63% of clinics can’t insert IUDs on the spot. In the U.S., community health centers are half as likely as academic hospitals to have protocols for these interactions. Cost, training gaps, and outdated assumptions still get in the way. But change is coming. The WHO is pushing for all national HIV guidelines to include contraceptive advice. New training programs have already reached over 8,000 providers worldwide. And the NEXT-Study, currently underway, is testing whether levonorgestrel IUDs work safely with every major antiretroviral. Results are due in late 2025.Final Takeaway
HIV treatment has come a long way. People are living longer, healthier lives. But birth control shouldn’t be an afterthought. It’s not just about preventing pregnancy-it’s about autonomy, dignity, and control over your body. You shouldn’t have to choose between staying healthy and not getting pregnant. If you’re on protease inhibitors, your birth control might not be working-even if you’re doing everything right. Talk to your provider. Get an IUD. Use condoms. Don’t wait for a surprise pregnancy to learn the hard way.Can HIV protease inhibitors make birth control pills ineffective?
Yes. Protease inhibitors like lopinavir, atazanavir, and darunavir-especially when boosted with ritonavir or cobicistat-can significantly lower hormone levels in birth control pills, patches, and rings. Studies show estrogen levels can drop by 35-83%, making these methods unreliable. Even perfect adherence doesn’t prevent this interaction.
Is the birth control implant safe with HIV medications?
No, not if you’re on ritonavir-boosted protease inhibitors. Studies show etonogestrel implants (like Nexplanon) can lose 40-60% of their hormone levels when taken with these drugs. The WHO and CDC recommend avoiding implants in this scenario. Hormonal IUDs are a safer alternative.
What’s the safest birth control for women on HIV drugs?
The copper IUD and hormonal IUD (like Mirena or Kyleena) are the safest options. They work locally in the uterus and aren’t affected by liver enzyme changes from HIV medications. Both are over 99% effective and last 3-12 years. Depo-Provera injections are also safe with most regimens, except efavirenz.
Does dolutegravir interfere with birth control?
No. Dolutegravir, an integrase inhibitor, has minimal to no interaction with hormonal contraceptives. It’s now the first-line HIV treatment for most people, including women of reproductive age, because it’s effective and doesn’t compromise birth control. If you’re on an older regimen, switching to dolutegravir may improve both your HIV control and contraceptive safety.
What should I do if I’m on a protease inhibitor and just found out I’m pregnant?
Contact your HIV provider and OB/GYN immediately. Many HIV medications are safe during pregnancy, but some need to be adjusted. Dolutegravir is now preferred in early pregnancy. Your team will help you switch drugs if needed and monitor your viral load and baby’s development. Don’t stop your HIV meds-uncontrolled HIV poses a greater risk to your baby than most medications.
Why don’t doctors always warn patients about this?
Many providers, especially in community clinics or low-resource settings, haven’t received updated training. A 2022 survey found that 34% of U.S. community health centers lack formal protocols for contraceptive-HIV drug interactions. Also, some assume patients will bring it up, or that birth control is “common sense.” But the data shows this interaction is overlooked far too often-with real consequences.
Can I use emergency contraception if I’m on HIV meds?
Levonorgestrel emergency pills (Plan B) may be less effective if you’re on protease inhibitors or efavirenz. The 2024 NIH report found levonorgestrel levels drop by 35% with darunavir/cobicistat. For better protection, use ulipristal acetate (Ella) or a copper IUD inserted within 5 days. The IUD is the most effective emergency option and also provides ongoing contraception.





Ravinder Singh
Man, this is the kind of post that should be mandatory reading for every HIV clinic worldwide. I’m from India, and I’ve seen too many women told ‘just take your pill’ without a word about drug interactions. The copper IUD is a game-changer-no hormones, lasts forever, and doesn’t care what antiretrovirals you’re on. 🙌 If your provider doesn’t bring this up, ask them. You deserve to be safe, not lucky.
Russ Bergeman
Wait… so you’re saying the pill doesn’t work? But I’ve been on it for 5 years!!! And my viral load is undetectable!! So… what now? 😅
Dana Oralkhan
I’m a nurse in a community clinic in Ohio, and I can tell you-this isn’t just theoretical. We had a patient last month who got pregnant on darunavir + the patch. She cried because she thought she was doing everything right. We switched her to a hormonal IUD the next week. She’s been calm ever since. Please, if you’re on PIs, don’t wait for a surprise. Get checked. Get an IUD. It’s not scary. It’s just smart.
Jeremy Samuel
lol so the pill dont work? what a shocker. i thought my body was a magic box that ignored drugs. also, i dont trust any study that says '38% of women'-sounds like they counted their exes.
Destiny Annamaria
OMG I just realized I’ve been on atazanavir + NuvaRing for 2 years. 😳 I’m literally booking my IUD appointment right now. Thank you for this. I’ve been so scared to say anything because I thought it was my fault if I got pregnant. Turns out it was the damn drug. 🤦♀️
Ron and Gill Day
This is just another example of how lazy medicine has become. Why are we still using protease inhibitors at all? If the data’s been out since 2010, then why are clinics still prescribing them to women? This isn’t ‘unavoidable’-it’s negligence. Someone should sue the manufacturers.
Alyssa Torres
I just want to say-this isn’t just about birth control. It’s about being seen. I’ve had doctors tell me, ‘Oh, you’re on HIV meds, so pregnancy isn’t a priority.’ Like my body isn’t mine. Like my desire to not get pregnant doesn’t matter. I got my IUD last year. I cried. Not because I was scared-but because for the first time, someone treated me like a whole person. 🫂
Summer Joy
So… you’re telling me I’ve been risking pregnancy this whole time?? And no one told me?? My doctor said ‘just use condoms’ like that’s enough?? I’m so mad right now. I’m not even mad at my doctor-I’m mad at the system. Why is this still a secret? 😭
Aruna Urban Planner
From a public health systems perspective, the disconnect lies in the fragmentation of HIV and reproductive care pathways. The pharmacokinetic interactions are well-documented, yet the operationalization of integrated counseling remains under-resourced. Structural barriers-such as provider training gaps and supply chain limitations for IUDs-exacerbate disparities, particularly in low- and middle-income settings. A systems-level intervention, rather than individual-level education, is required to mitigate this risk at scale.
Nicole Ziegler
Just got my Mirena inserted yesterday. 🎉 No more worrying about pills, rings, or patches. And my HIV doc didn’t even blink. Just said, ‘Smart move.’ I feel like a superhero now. 💪🩺
Bharat Alasandi
Bro, I’m on darunavir/ritonavir and was using the shot. My doc said it’s fine. But now I’m confused. Should I switch? I don’t wanna mess with my regimen. Anybody else in this boat?
Kristi Bennardo
This is irresponsible. If you're going to publish information about contraceptive failure, you must include the full list of contraindications, absolute risk percentages, and clinical trial citations. This post is dangerously oversimplified. Someone could die because of this.
Shiv Karan Singh
Oh so now we’re blaming the drugs? My cousin got pregnant on the pill and she was on tenofovir. So it’s not the PI? It’s her fault? 🤷♂️
Ravi boy
im on dolutegravir and i use the patch and i never had a problem. maybe its just me? idk but i think this whole thing is overblown. also i spelled contraceptive wrong lol