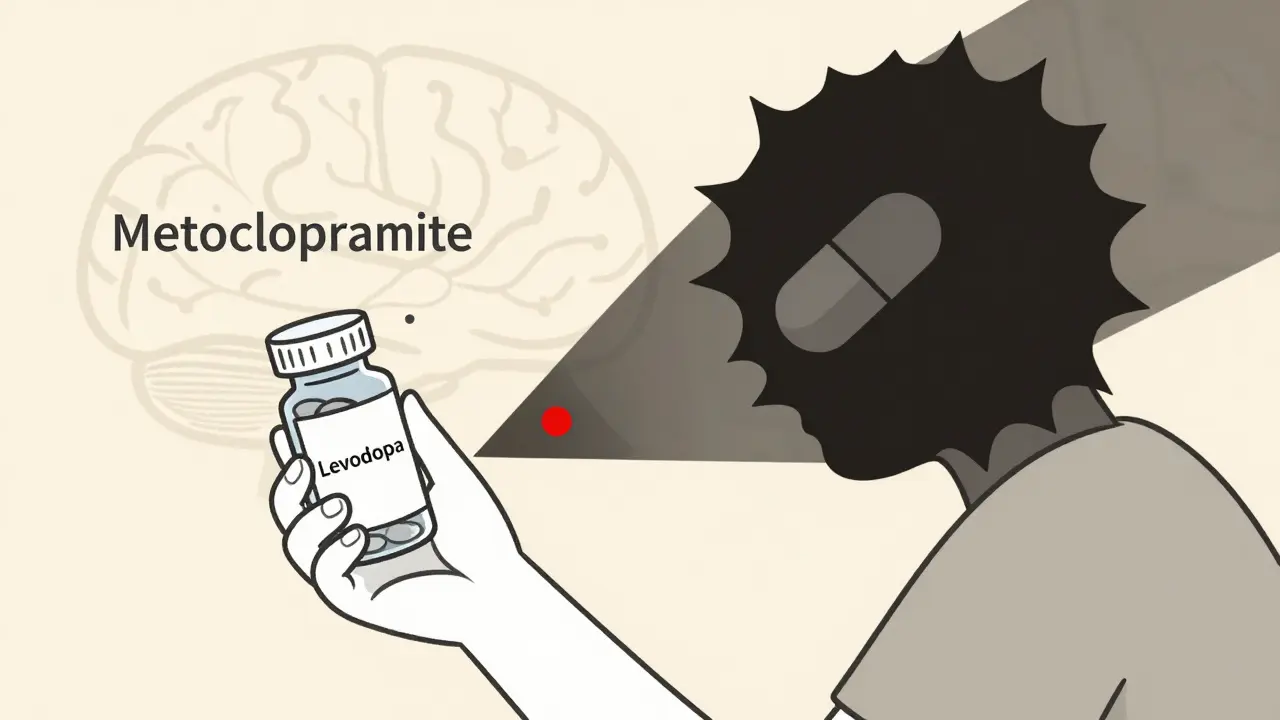
When you’re living with Parkinson’s disease, nausea isn’t just uncomfortable-it can be a sign that your treatment is working. Levodopa, the main drug used to manage Parkinson’s, causes nausea in 40 to 80% of patients when they first start taking it. But here’s the problem: the most common drugs doctors reach for to stop that nausea-like metoclopramide, prochlorperazine, and haloperidol-can make your Parkinson’s symptoms dramatically worse.
Why Dopamine Blockers Are a Double-Edged Sword
Parkinson’s disease is caused by the slow death of dopamine-producing cells in the brain. That’s why levodopa is the cornerstone of treatment: it gets converted into dopamine to replace what’s been lost. But antiemetics like metoclopramide (Reglan) and prochlorperazine (Stemetil) work by blocking dopamine receptors. That’s great for stopping vomiting in the gut, but when these drugs cross into the brain, they block dopamine in the same areas already struggling to function. This isn’t just theoretical. A 2022 survey by the Michael J. Fox Foundation found that 68% of Parkinson’s patients who received dopamine-blocking antiemetics in the hospital reported a sudden spike in tremors, stiffness, or freezing episodes. One patient on the Parkinson’s NSW Forum described how a single dose of metoclopramide after dental surgery sent his tremors into overdrive-taking three weeks to recover, even after increasing his levodopa dose.Not All Antiemetics Are Created Equal
The key difference between safe and dangerous antiemetics comes down to one thing: whether the drug can get into your brain. High-risk antiemetics (avoid completely):- Metoclopramide (Reglan, Maxalon)
- Prochlorperazine (Stemetil)
- Haloperidol (Haldol)
- Chlorpromazine
- Promethazine
- Domperidone (Motilium)
- Cyclizine (Vertin)
- Ondansetron (Zofran)
The Dangerous Gap Between Guidelines and Practice
You’d think this would be common knowledge. But a 2022 study in the Journal of Parkinson’s Disease found that only 37% of emergency room doctors could correctly identify metoclopramide as dangerous for Parkinson’s patients. That means over 6 in 10 ER staff are giving a drug that could send someone into a severe “off” state. It gets worse. The Anesthesia Patient Safety Foundation reports that 25% of Parkinson’s patients still receive dopamine-blocking antiemetics during surgery or in post-op care. Each incident adds an average of $3,200 in extra hospital costs and delays recovery by days. Many patients are discharged with prescriptions they shouldn’t have, because their neurologist wasn’t consulted.
What to Do If You’re Nauseous
Don’t panic. There are clear, safe steps to take. Step 1: Try non-drug options first. Ginger (1 gram daily in capsule or tea form), eating small meals, staying hydrated, and sitting upright after eating can reduce nausea in many patients. Dr. Espay recommends these as first-line treatments. Step 2: If you need a drug, ask for domperidone or cyclizine. Domperidone is preferred if available. If not, cyclizine is a solid second choice. Ondansetron works for some, but it’s less reliable for levodopa-induced nausea. Step 3: Never accept metoclopramide, prochlorperazine, or haloperidol. If a doctor suggests one of these, say: “I have Parkinson’s. Are you aware these can make my symptoms worse?” Then ask for an alternative. Step 4: Carry your medication card. The American Parkinson Disease Association has distributed over 250,000 wallet cards listing dangerous drugs. If you have one, show it. If you don’t, download and print one from their website. Many patients report a 40% drop in inappropriate prescriptions after carrying the card.What About Levomepromazine or Other “Middle-Ground” Drugs?
Levomepromazine (Nozamine) is sometimes used in palliative care for severe nausea. It’s not a clear yes or no. It has moderate dopamine-blocking effects-around a 30-40% risk of worsening Parkinson’s. The GGC Medicines Update says it should only be used after discussion with both a Parkinson’s specialist and a palliative care doctor. Even then, start low: 6.25 mg twice daily, max 25 mg daily.
The Future Is Brighter
There’s real progress. The Parkinson’s Foundation’s 2023 Quality Improvement Initiative trained over 1,200 doctors and nurses in antiemetic safety. In hospitals that participated, inappropriate prescriptions dropped by 55%. New drugs are coming. Aprepitant (Emend), which blocks a different nausea pathway (neurokinin-1), showed 92% effectiveness in a 2023 trial with zero motor side effects. The Michael J. Fox Foundation is funding research into a new serotonin modulator designed to stop nausea without touching dopamine at all.Final Takeaway: Your Voice Matters
Nausea is common in Parkinson’s. But the wrong antiemetic can undo weeks of progress. The safest path isn’t always the fastest. It’s not about avoiding all drugs-it’s about choosing the right ones. If you’re prescribed an antiemetic, ask:- Is this a dopamine blocker?
- Will it cross into my brain?
- Is there a safer alternative?
Can I take metoclopramide if I have Parkinson’s disease?
No. Metoclopramide is a dopamine D2 receptor antagonist that crosses the blood-brain barrier and can significantly worsen Parkinson’s motor symptoms like tremors, stiffness, and freezing. The American Parkinson Disease Association and Movement Disorder Society classify it as contraindicated. Even though it’s sometimes used for nausea, the risks far outweigh the benefits for Parkinson’s patients.
Is domperidone safe for Parkinson’s patients?
Yes, domperidone is generally considered the safest antiemetic option for Parkinson’s patients. It blocks dopamine receptors in the gut but doesn’t cross the blood-brain barrier due to P-glycoprotein efflux. Studies show less than 2% risk of worsening motor symptoms. It’s widely used in Australia, Canada, and Europe. In the U.S., it’s only available through a special FDA program (IND application) due to cardiac safety concerns, but these are unrelated to Parkinson’s.
What antiemetic should I ask my doctor for instead of metoclopramide?
Ask for cyclizine (Vertin) or domperidone (Motilium). Cyclizine is an antihistamine with minimal dopamine activity and a 5-10% risk of worsening symptoms. Domperidone is preferred if available. Ondansetron (Zofran) is another option, though it’s less effective for levodopa-induced nausea. Always confirm with your neurologist before starting any new medication.
Why do emergency rooms keep giving me dangerous antiemetics?
Many ER doctors aren’t trained in Parkinson’s-specific drug interactions. A 2022 study found only 37% could correctly identify metoclopramide as dangerous. Nausea is common in ER visits, and metoclopramide is fast, cheap, and widely stocked. The solution? Carry a printed medication warning card from the American Parkinson Disease Association and say, “I have Parkinson’s-please avoid dopamine-blocking drugs.”
Can ginger really help with Parkinson’s nausea?
Yes. Clinical experience and patient reports show that 1 gram of ginger daily (in capsule or tea form) reduces nausea in many Parkinson’s patients. It’s not a cure-all, but it’s a safe, non-drug first step recommended by experts like Dr. Alberto Espay. Combine it with small, frequent meals and staying upright after eating for best results.
What should I do if I’ve already taken metoclopramide and my symptoms got worse?
Stop taking it immediately. Contact your neurologist or Parkinson’s nurse. Symptoms like increased tremors, rigidity, or freezing usually improve over days to weeks once the drug is cleared. Do not increase your levodopa dose on your own-this can lead to dyskinesia. Document the timing and severity of symptoms to help your doctor adjust your treatment plan.
Are atypical antipsychotics safer than antiemetics for Parkinson’s patients?
Yes, but only if they’re specifically designed for Parkinson’s psychosis. Drugs like clozapine (Clozaril), quetiapine (Seroquel), and pimavanserin (Nuplazid) have minimal dopamine-blocking effects in motor areas. They’re used for hallucinations or delusions in advanced Parkinson’s-not for nausea. Never use them as substitutes for antiemetics. Their purpose and dosing are completely different.





Payton Daily
Man, I had no idea metoclopramide could wreck your Parkinson’s like that. I thought it was just for nausea. Now I’m wondering how many people out there are getting worse because some ER doc just grabbed the first thing on the shelf. This is wild. Like, why isn’t this taught in med school?!
Kelsey Youmans
Thank you for this meticulously researched and profoundly important post. The clinical implications are staggering, and the human cost-measured in tremors, dignity, and lost time-is incalculable. I urge all healthcare professionals to internalize these guidelines and advocate for systemic change.
Sydney Lee
Let’s be clear: this isn’t just medical negligence-it’s institutional betrayal. The FDA’s ban on domperidone? A corporate farce. The fact that patients have to beg for a safe drug while hospitals stock poison like it’s aspirin? This is capitalism turning human suffering into a cost-benefit spreadsheet. And don’t get me started on how ‘cheap and fast’ became the moral compass of emergency medicine.
They don’t care about you. They care about turnover. About liability. About not having to look up a damn drug interaction. And you? You’re just a case number with a tremor.
oluwarotimi w alaka
u think this is bad? wait till u hear about how the west hides the truth about meds. in africa we use natural herbs and no one gets worse. they poison us with pills then say we dont know science. this is all a trick to make us buy more drugs. domperidone? its banned for a reason. they dont want you to be healthy. they want you hooked.
Debra Cagwin
This is such an important reminder for everyone-patients, caregivers, even friends and family. If you or someone you love has Parkinson’s, please, please carry that wallet card. It’s simple, it’s powerful, and it could save someone from months of suffering. You’re not being difficult-you’re being your own best advocate. I’m so proud of how many of you are speaking up.
And if you’re a provider reading this? Thank you for learning. Every time you pause and ask, ‘Is this safe?’ you’re changing lives.
Hakim Bachiri
Domperidone?? You’re telling me we can’t get this in the US because of ‘heart risks’?? Bro. The same FDA that approved Ozempic for weight loss won’t let a guy with Parkinson’s get a drug that doesn’t even cross his blood-brain barrier?? This is pure corporate greed wrapped in a lab coat. They’d rather let you freeze in a hospital bed than risk a lawsuit. And don’t even get me started on how they’re charging $500 for a 30-day supply of Zofran while domperidone costs $10 overseas…
It’s not medicine. It’s a scam.
Celia McTighe
OMG I just showed this to my dad-he’s been on levodopa for 8 years and got metoclopramide after his knee surgery last year 😭 he was stuck in ‘off’ mode for 3 weeks. We had no idea it was the drug. I’m printing out that wallet card right now. Thank you for sharing this. 🙏❤️
Ryan Touhill
Interesting. But let’s not ignore the fact that domperidone’s cardiac risks aren’t trivial-QT prolongation is real. And while it’s true that ER docs are undertrained, the real issue is systemic: we’ve outsourced patient education to Reddit threads and blog posts. Shouldn’t this be in the EMR alerts? In the formulary restrictions? In the hospital protocols? This isn’t about individual advocacy-it’s about institutional accountability. We need policy, not pamphlets.