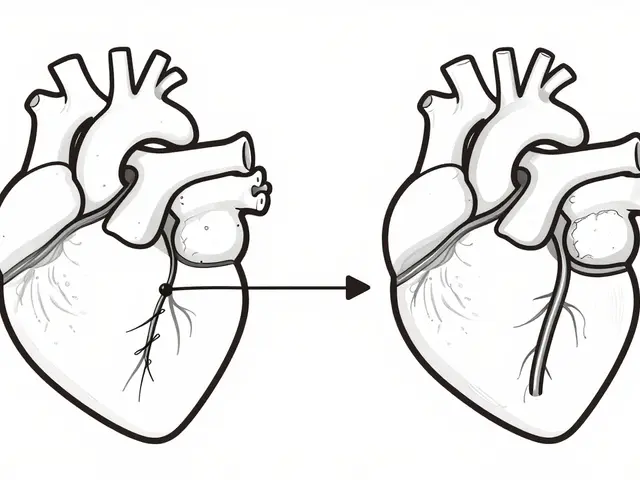
What if your body was sending you warning signs - not in the form of chest pain or dizziness, but through quiet, everyday changes: a growing waistline, rising blood sugar, stubborn high cholesterol? These aren’t just isolated issues. They’re signals of something bigger: metabolic syndrome. And if left unchecked, it doesn’t just raise your risk of heart disease - it sets you up for a cascade of life-altering health problems.
What Exactly Is Metabolic Syndrome?
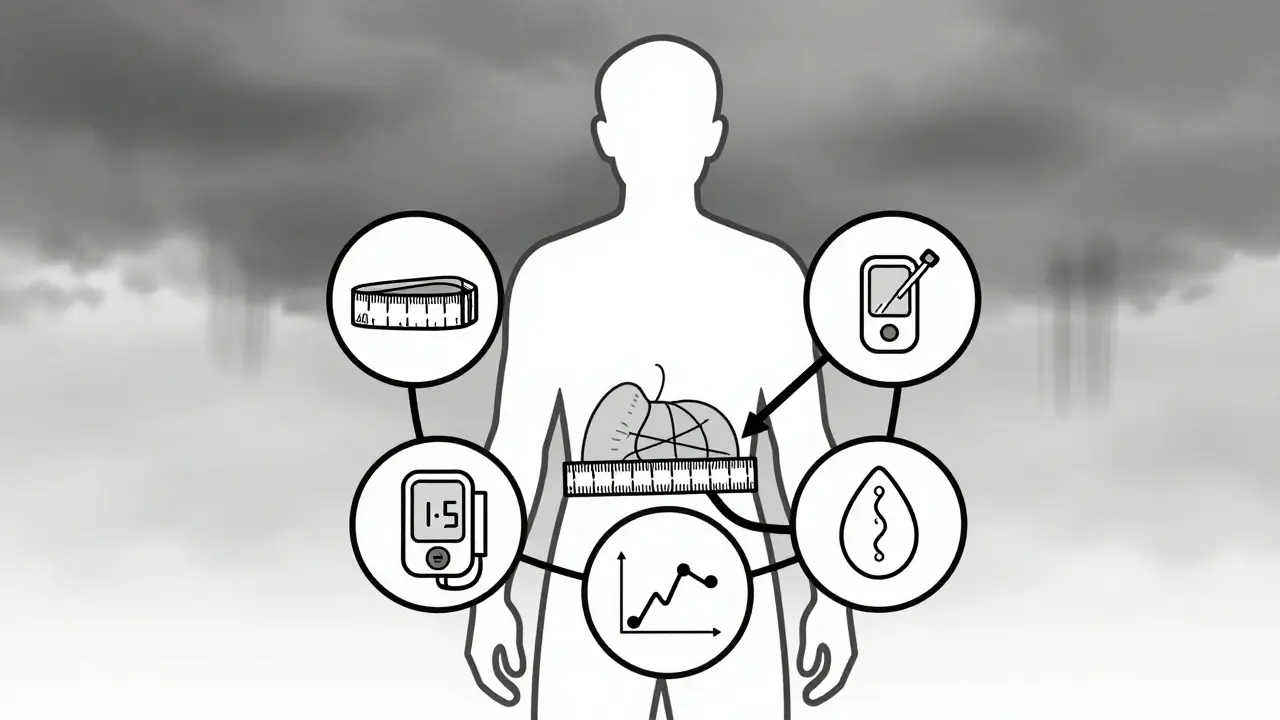
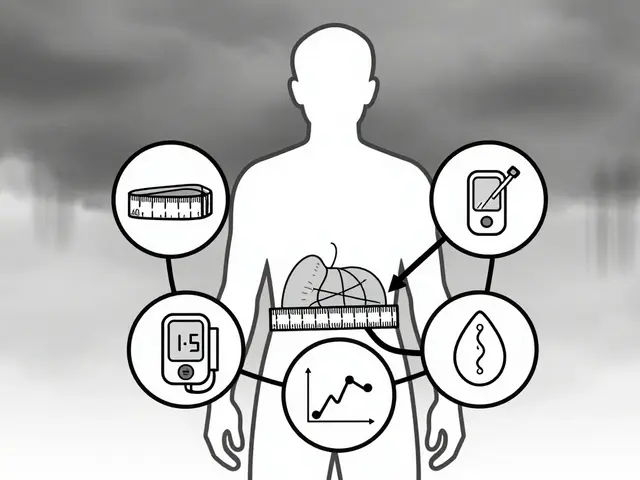
Metabolic syndrome isn’t a single disease. It’s a cluster of five related conditions that, when they show up together, dramatically increase your chances of developing heart disease, stroke, and type 2 diabetes. Think of it like a storm system: each factor alone is manageable. But when they gather - insulin resistance, belly fat, high blood pressure, abnormal cholesterol, and elevated blood sugar - they create a perfect storm for damage. To be diagnosed, you need at least three of these five criteria:- Waist circumference over 40 inches (102 cm) for men, or 35 inches (88 cm) for women
- Triglycerides at or above 150 mg/dL
- HDL ("good") cholesterol below 40 mg/dL for men, or 50 mg/dL for women
- Blood pressure at or above 130/85 mmHg
- Fasting blood sugar of 100 mg/dL or higher
Why Insulin Resistance Is the Root Cause
At the center of metabolic syndrome is insulin resistance. This isn’t just about sugar. It’s about how your body’s cells stop listening to insulin, the hormone that tells them to absorb glucose from your blood. When cells become resistant, your pancreas pumps out more insulin to compensate. That extra insulin doesn’t just raise blood sugar - it triggers a chain reaction. High insulin levels promote fat storage, especially around your abdomen. Visceral fat (the kind that clings to your organs) doesn’t just sit there. It releases inflammatory chemicals and free fatty acids that make your liver and muscles even more resistant to insulin. It’s a vicious cycle: insulin resistance → more belly fat → worse insulin resistance. This is why metabolic syndrome is different from having high blood pressure alone, or high cholesterol alone. Those conditions can come from genetics, stress, or aging. But when they appear together with abdominal obesity and high blood sugar, it’s almost always because insulin resistance is pulling the strings.Who’s at Risk - And Why It’s Worse Than You Think
About one in three American adults has metabolic syndrome - that’s over 86 million people. But it’s not evenly spread. Prevalence jumps from 20% in people aged 20-39 to nearly 50% in those over 60. Ethnic disparities are stark: 38.6% of Hispanic adults, 34.2% of non-Hispanic whites, and 31.8% of non-Hispanic Black adults are affected. Even lower rates in Asian populations don’t mean safety - because for Asians, the waist thresholds are lower (90 cm for men, 80 cm for women), meaning they develop metabolic risks at smaller waist sizes. Obesity is the biggest driver. Since 2000, abdominal obesity in U.S. adults has risen from 46% to nearly 60%. But it’s not just about weight. People with polycystic ovary syndrome (PCOS), sleep apnea, or a history of gestational diabetes are at much higher risk. Even if you’re not overweight, a sedentary lifestyle and a diet high in refined carbs and sugar can trigger insulin resistance. The scary part? Most people don’t know they have it. A 2022 survey on HealthUnlocked found that 68% of people with metabolic syndrome weren’t diagnosed - their doctors treated their high blood pressure or high cholesterol as separate issues, missing the bigger picture.
Why Lifestyle Change Is the Only Real Treatment
There’s no pill that cures metabolic syndrome. No drug targets all five components at once. That’s why the only proven, long-term solution is lifestyle change - and not just any change. It has to be structured, consistent, and focused. The Diabetes Prevention Program (DPP), a landmark NIH study, showed that losing just 7% of your body weight - say, 15 pounds if you weigh 215 - and doing 150 minutes of brisk walking per week reduced the risk of developing type 2 diabetes by 58%. Over 10 years, this same intervention cut the incidence of metabolic syndrome by 41%. The key components?- Diet: Cut out sugary drinks, white bread, pastries, and processed snacks. Focus on vegetables, lean proteins, whole grains, nuts, and healthy fats like olive oil and avocado. Aim for 1,200-1,500 calories daily if you’re a woman, 1,500-1,800 if you’re a man.
- Exercise: 30 minutes of moderate activity - walking, cycling, swimming - five days a week. Strength training twice a week helps too, because muscle burns more glucose than fat.
- Sleep and stress: Poor sleep and chronic stress raise cortisol, which increases belly fat and insulin resistance. Aim for 7-8 hours of quality sleep. Meditation, deep breathing, or even daily walks can help manage stress.
The Role of Technology and New Tools
In 2023, the FDA approved the first digital therapeutic for metabolic syndrome: DarioHealth’s Metabolic+ app. It combines continuous glucose monitoring with personalized coaching. In a trial, users saw their HbA1c drop by 0.6% and their waistline shrink by over 3 cm in just six months - results that matched or beat traditional programs. Wearable tech, like Fitbit or Apple Watch, now track activity, sleep, and even heart rate variability - all useful indicators of metabolic health. Apps that log meals and suggest portion sizes help people stay accountable without needing a dietitian on speed dial. The American College of Cardiology now recommends that people with metabolic syndrome be considered for earlier statin therapy, even if their cholesterol levels aren’t extremely high. Why? Because the syndrome itself is now classified as a "risk enhancer" - meaning it adds weight to your overall cardiovascular risk profile.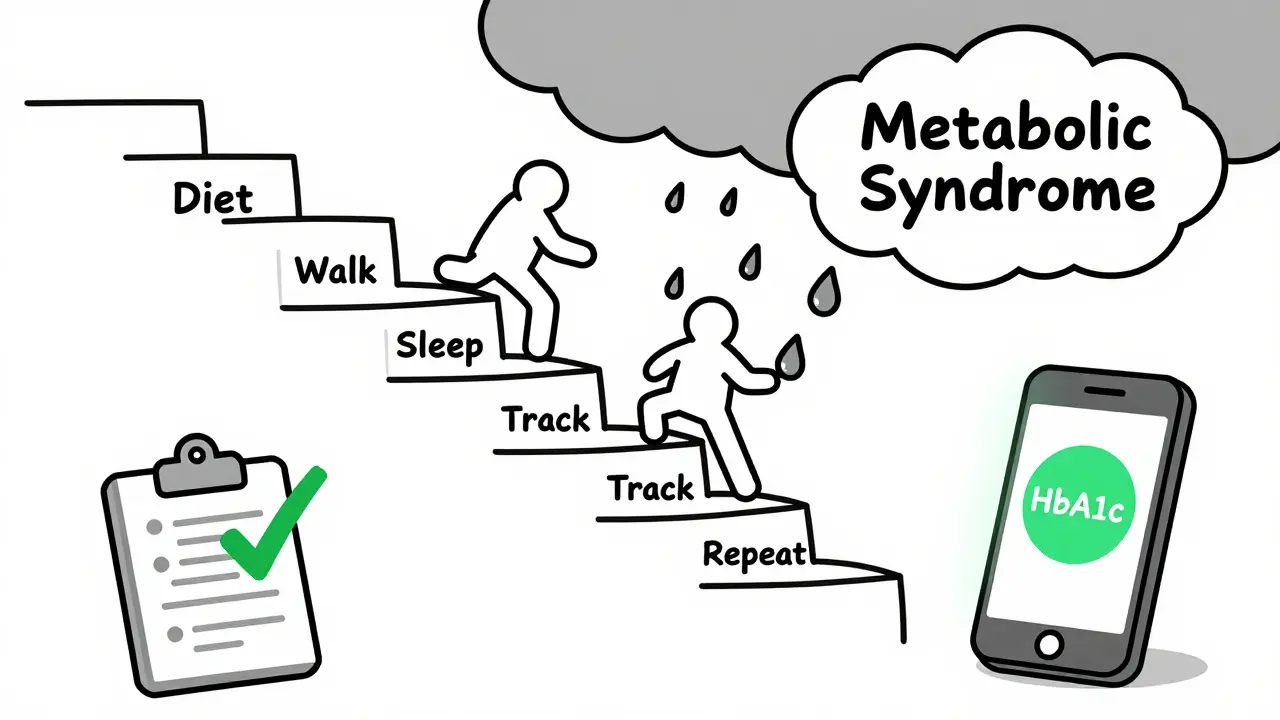
What Doesn’t Work - And Why
Many people try quick fixes: keto diets for a month, detox teas, or extreme fasting. These might drop the scale, but they rarely fix insulin resistance. In fact, yo-yo dieting can make it worse by increasing inflammation and fat storage around organs. Medications like metformin can help with blood sugar, and statins lower cholesterol. But they don’t reverse the syndrome. They manage symptoms. Only lifestyle change addresses the root cause. And here’s the hard truth: healthcare systems aren’t built for this. Most doctors have 15-minute appointments. Insurance often won’t cover nutrition counseling or exercise programs. Only 28% of Medicare Advantage plans fully cover evidence-based lifestyle interventions, according to a 2022 Kaiser Family Foundation report. That’s why community programs matter. The CDC’s National Diabetes Prevention Program uses trained coaches - often lay health workers - to guide groups through weekly sessions. In Hispanic communities, these programs achieved better weight loss than standard care, proving that peer support and cultural relevance make a difference.Can Metabolic Syndrome Be Reversed?
Yes. And not just improved - reversed. The DiRECT trial, published in The Lancet, followed people with type 2 diabetes and metabolic syndrome who lost 15 kg or more through a structured, low-calorie diet and behavioral support. After one year, 46% no longer met the criteria for metabolic syndrome. Their blood pressure normalized. Their triglycerides dropped. Their insulin sensitivity improved. This isn’t magic. It’s biology. When you remove the excess fat - especially visceral fat - your liver and muscles start responding to insulin again. The inflammation fades. The cycle breaks. The key? Consistency. Not perfection. One healthy meal. One walk. One night of good sleep. Repeat.What to Do Next
If you’re reading this and wondering if you might have metabolic syndrome, here’s your action plan:- Measure your waist. Stand up, relax, and wrap a tape around your belly at the level of your navel. If it’s over 40 inches (men) or 35 inches (women), that’s a red flag.
- Check your last blood test. Do you have high triglycerides? Low HDL? High fasting glucose? Even one of these should prompt a conversation with your doctor.
- Start small. Swap one sugary drink for water. Take a 20-minute walk after dinner. Skip the dessert once a week.
- Ask for a metabolic panel. Request fasting glucose, triglycerides, HDL, and blood pressure readings. Don’t assume your annual checkup covered everything.
- Find support. Join a CDC-recognized program, find a friend to walk with, or use a free app to track progress.
Can you have metabolic syndrome and not be overweight?
Yes. While abdominal obesity is one of the main criteria, some people - especially those with a genetic predisposition or hormonal conditions like PCOS - can develop insulin resistance and the other markers of metabolic syndrome even at a normal weight. It’s called "TOFI" - thin outside, fat inside. Visceral fat can accumulate without visible belly fat.
Does metabolic syndrome always lead to diabetes?
Not always, but the risk is very high. About 75-80% of new type 2 diabetes cases are linked to metabolic syndrome. Without intervention, up to 70% of people with the syndrome will develop diabetes within 10 years. But lifestyle changes can cut that risk by more than half.
Is metabolic syndrome the same as prediabetes?
No. Prediabetes means your blood sugar is higher than normal but not yet diabetic. Metabolic syndrome includes prediabetes as one of its five components, but also adds high blood pressure, abnormal cholesterol, and abdominal obesity. You can have prediabetes without metabolic syndrome - and vice versa, though they often overlap.
Can medications cure metabolic syndrome?
No. Medications can treat individual components - like statins for cholesterol or ACE inhibitors for blood pressure - but none are approved to treat the syndrome as a whole. Lifestyle change remains the only proven way to reverse it. Drugs may help manage symptoms, but they don’t fix the underlying insulin resistance.
How long does it take to reverse metabolic syndrome?
Many people see improvements in as little as 3-6 months with consistent lifestyle changes. Losing just 5-7% of body weight can normalize blood sugar and lower blood pressure. Full reversal - meeting none of the five diagnostic criteria - often takes 9-12 months, especially if weight loss is sustained and physical activity becomes routine.



jessica .
this is all government propaganda to get you to buy their fake meds and wearable trackers. they made up metabolic syndrome so they could sell you more tests. i saw a video on TruthTube that showed the CDC paid researchers to inflate the numbers. your waist size? it's your right to be fat. they want you scared so you'll take their pills. 🤡
Erica Vest
The clinical definition of metabolic syndrome is well-established in peer-reviewed literature, primarily through the IDF and AHA/NHLBI criteria. The clustering of visceral adiposity, insulin resistance, dyslipidemia, and hypertension is not arbitrary-it reflects shared pathophysiological pathways. Lifestyle intervention remains the cornerstone of management, with robust evidence from the DPP and DiRECT trials demonstrating reversal potential. Pharmacotherapy addresses individual components but not the underlying syndrome.
Chris Davidson
People don't get it. It's not about diet. It's about weakness. You let your body go. You eat junk. You sit. You blame the system. The system doesn't care. Your body does. If you can't control your eating and your time then you deserve what you get. No magic pills. No apps. Just discipline. Or don't. Your call
Ashley Bliss
I've been waiting for someone to finally say this out loud... this isn't medicine. This is a spiritual crisis disguised as science. We've been taught to fear our own bodies, to see fat as evil, to worship cholesterol like it's a demon. But what if... what if the real disease is the alienation we feel from our own flesh? What if insulin resistance is just the body screaming 'I'm tired of being lied to'? I lost 40 pounds on a keto diet and still felt hollow. Then I started walking barefoot in the grass at dawn. My triglycerides dropped. My soul did too. They can't measure that in a lab. But I know it. And I'm not alone.
Dev Sawner
The prevalence data presented is statistically valid but culturally biased. The waist circumference thresholds for Asian populations are appropriately adjusted; however, the underlying assumption that visceral adiposity is the primary driver of insulin resistance lacks universal applicability. In South Asian populations, ectopic fat deposition in the liver and skeletal muscle often precedes abdominal adiposity, suggesting a need for biomarker-based diagnostics over anthropometric criteria. Furthermore, the DPP results, while robust, are not generalizable to populations with lower caloric intake and higher physical activity baselines.
Moses Odumbe
Bro. I had metabolic syndrome. Lost 25 lbs. Walked every day. Cut soda. Used MyFitnessPal. Now my HbA1c is 5.2. No meds. Just consistency. 🚶♂️💪 Don't overthink it. Eat real food. Move your body. Sleep. Repeat. The app I used? DarioHealth. Free trial. Life changer. 🤝
Connie Zehner
I read this and I cried. I've been living with this for 8 years. My doctor said it was 'just aging.' But I knew. I felt it in my bones. The fog. The exhaustion. The way my clothes didn't fit even though I wasn't 'fat.' I started walking at 5am. I stopped drinking wine. I found a support group. I'm not cured. But I'm alive. And if you're reading this and you're scared? I see you. I'm right here with you. 💔❤️
mark shortus
I just found out I have metabolic syndrome. My wife left me. My boss thinks I'm lazy. My knees hurt. I'm 42. I used to be a runner. Now I can't walk to the mailbox without breathing hard. I tried keto. I tried intermittent fasting. I tried the damn app. Nothing stuck. I don't know if I can do this anymore. I just... I don't know. I'm tired.
Elaine Douglass
mark shortus i feel you. i was right there. i thought i was failing. but you know what? i started with one walk. just 10 minutes. then 15. then i swapped my soda for sparkling water. no big changes. just tiny ones. now i walk every night with my dog. we talk. i cry sometimes. but i'm here. you're not alone. 💛