CLL Treatment Personalization Calculator
Patient Profile
When doctors talk about personalized medicine is a health‑care approach that tailors prevention, diagnosis and therapy to an individual’s genetic, molecular and lifestyle profile, they’re describing a shift that’s now reshaping how we fight Chronic Lymphocytic Leukemia (CLL). Once considered a slow‑growing disease with limited options, CLL today boasts a menu of targeted drugs, immune‑cell products and precision diagnostics that let clinicians strike at the cancer’s specific weaknesses.
Why One‑Size‑Fits‑All No Longer Works
Traditional chemotherapy treats cancer like a blunt instrument - it damages rapidly dividing cells whether they’re malignant or healthy. In CLL, that often meant weeks of fatigue, infection risk and modest response rates. The problem isn’t the drug; it’s that CLL isn’t a single disease. Genetic lesions, such as TP53 mutation (a defect that disables a key tumor‑suppressor pathway) or the status of the IGHV gene (mutated vs. unmutated immunoglobulin heavy‑chain variable region), dictate how aggressive the leukemia behaves and how it reacts to therapy.
Key Pillars of Precision in CLL
Three technological pillars enable true molecular profiling (high‑resolution analysis of DNA, RNA and protein alterations) of CLL patients:
- Next‑generation sequencing (NGS) panels that screen for >30 CLL‑relevant genes in a single run.
- Fluorescence in situ hybridization (FISH) to spot common chromosomal deletions such as del(17p).
- Flow‑cytometry based minimal residual disease (MRD) testing, which quantifies disease burden down to one cancer cell in a million normal cells.
These data points feed directly into treatment algorithms, deciding whether a patient should start on a BTK inhibitor, a BCL‑2 inhibitor, or head straight to an immunotherapy.

Targeted Therapies: From Broad to Ultra‑Specific
Two drug classes now dominate the first‑line landscape:
| Agent | Mechanism | Typical Response Rate | Key Side Effects |
|---|---|---|---|
| Ibrutinib | A BTK inhibitor | ≈80% complete remission (CR) in fit patients | Atrial fibrillation, bleeding, hypertension |
| Venetoclax | A BCL‑2 inhibitor | ≈90% MRD‑negative remission when combined with anti‑CD20 antibodies | Tumor lysis syndrome, neutropenia, diarrhea |
| KTE‑X19 (CAR‑T) | Engineered CAR T‑cell therapy | ≈70% durable CR in relapsed/refractory setting | Cytokine release syndrome, neurotoxicity |
Choosing among them depends on a patient’s genetic landscape, comorbidities and personal preferences. For example, a 68‑year‑old with a TP53 mutation and a history of atrial fibrillation may avoid Ibrutinib and start with Venetoclax, which sidesteps cardiac risk while delivering deep remissions.
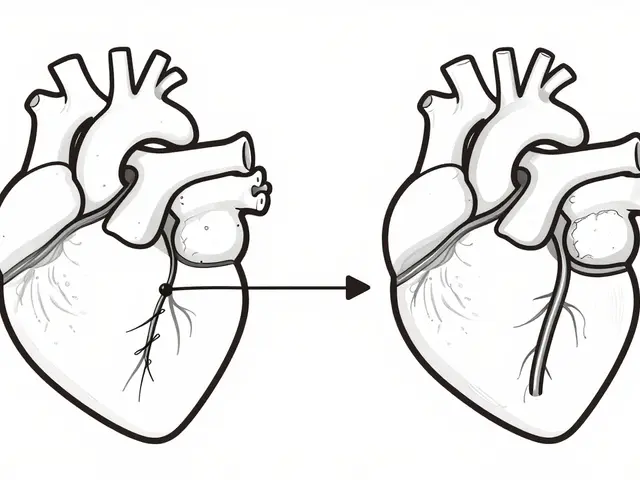
Putting Genetic Data to Work: Real‑World Decision Flow
Below is a simplified flow that many oncology clinics follow after receiving a molecular report:
- Identify high‑risk lesions (TP53 loss, del(17p)). If present, prioritize a BCL‑2 inhibitor or consider early CAR‑T referral.
- Check IGHV mutation status. Unmutated IGHV predicts a more aggressive course; clinicians often add a BTK inhibitor to boost durability.
- Review comorbidities (cardiac, hepatic, renal). Choose agents with the safest side‑effect profile for the individual.
- After starting therapy, monitor MRD every 3-6months. Achieving MRD‑negativity may allow time‑limited treatment rather than indefinite dosing.
This algorithm illustrates how personalized medicine isn’t just a buzzword-it’s a step‑by‑step roadmap that translates genetic numbers into concrete treatment moves.
Challenges on the Path to Full Personalization
Even with powerful tools, clinicians face hurdles:
- Access and cost. Targeted agents and NGS panels can run into tens of thousands of dollars per patient, creating inequities across health systems.
- Data interpretation. A TP53 mutation is clear‑cut, but many variants of unknown significance (VUS) still leave doctors guessing.
- Resistance mechanisms. CLL cells can acquire new mutations that bypass BTK inhibition, necessitating sequential therapy changes.
Addressing these issues requires policy support for reimbursement, expanded databases that classify VUS, and ongoing research into combination regimens that forestall resistance.
Looking Ahead: The Next Generation of Tailored CLL Care
Several emerging trends promise to tighten the personalization loop:
- Single‑cell sequencing. By dissecting the tumor ecosystem at a cellular level, doctors could target sub‑clones before they dominate.
- Bispecific antibodies. Molecules that bind both CD20 on CLL cells and CD3 on T‑cells are already showing activity in early trials.
- Artificial intelligence‑driven risk models. AI can crunch thousands of molecular and clinical variables to predict which patients will benefit most from a given drug.
When these technologies mature, the goal will be to start every CLL patient on the exact regimen that guarantees the longest remission with the fewest side effects-no trial‑and‑error needed.
Quick Takeaways
- Personalized medicine leverages genetic and molecular data to match CLL patients with the most effective targeted therapy.
- Key biomarkers include TP53 mutation, IGHV status, and MRD levels.
- BTK inhibitors, BCL‑2 inhibitors, and CAR‑T cells are the three main pillars of modern CLL treatment.
- Cost, data complexity, and drug resistance remain the biggest obstacles.
- Future advances-single‑cell analysis, bispecific antibodies, and AI-will sharpen treatment precision even further.
Frequently Asked Questions
What is the difference between a BTK inhibitor and a BCL‑2 inhibitor?
BTK inhibitors (e.g., Ibrutinib) block a signaling enzyme that CLL cells use to survive, while BCL‑2 inhibitors (e.g., Venetoclax) directly trigger programmed cell death by disabling a protein that protects cancer cells from apoptosis. The choice depends on the patient’s genetic lesions and tolerance for specific side effects.
How does MRD testing guide treatment length?
If MRD testing shows no detectable disease after a defined period (often 12 months), many physicians will stop continuous therapy and switch to observation, reducing exposure to drug toxicity and cost.
Can patients with TP53 mutations still benefit from BTK inhibitors?
BTK inhibitors do work in TP53‑mutated CLL, but response depth is usually lower than with BCL‑2 inhibitors. Many experts start with a BCL‑2 inhibitor or combine both classes to achieve deeper remissions.
Is CAR‑T therapy approved for first‑line CLL treatment?
As of 2025, CAR‑T (e.g., KTE‑X19) is approved for relapsed or refractory CLL after at least one prior therapy. Ongoing trials are testing it earlier, but it’s not yet standard first‑line care.
What are the biggest cost drivers for personalized CLL care?
Targeted drugs (especially BTK and BCL‑2 inhibitors), NGS panel testing, and CAR‑T manufacturing all carry high price tags. Insurance coverage varies widely by country and health system.





Claire Kondash
Personalized medicine in CLL feels like an echo of the age‑old philosophical debate between determinism and free will, where each patient’s genome writes a script that both constrains and empowers therapeutic choice. 🌌 The discovery of TP53 mutations and IGHV status reshapes our understanding of destiny, suggesting that biology not only dictates risk but also opens doors to targeted interventions. 🎯 When we speak of a “blunt instrument” like chemotherapy, we are invoking a metaphor for a world that once ignored individual nuance, much like ancient societies that imposed uniform laws on diverse peoples. 🌍 Yet today’s molecular panels act as moral philosophers, interrogating each cell’s narrative and demanding a tailored response. 🧬 The very act of sequencing becomes a dialogue between clinician and patient, a Socratic inquiry into what it means to be ill. 📜 Moreover, the ability to monitor MRD with such precision is akin to a modern oracle, offering glimpses of remission that were previously unimaginable. 🌟 The ethical implications are profound: should we allocate expensive targeted agents based on genetic risk, or strive for egalitarian access regardless of molecular profile? 🤔 The answer, perhaps, lies in a synthesis of justice and efficacy, a balance that respects both the science and the human story behind each barcode. 🔬 As we integrate AI‑driven risk models, we edge closer to a future where treatment decisions are not merely reactive but preemptively shaped by predictive patterns, echoing the deterministic threads of fate while preserving agency. 🧩 In this evolving landscape, the patient’s voice becomes as essential as the data, reminding us that medicine, at its core, remains a profoundly personal endeavor. 🌱
Matthew Ulvik
Totally agree, this stuff really changes the game! :)
Mark Eddinger
From a clinical standpoint, the integration of NGS panels and MRD assessment provides a robust framework for risk‑adapted therapy. The data support the preferential use of BCL‑2 inhibitors in TP53‑mutated cases, given their superior depth of response. Conversely, BTK inhibitors remain appropriate for patients without high‑risk cytogenetics and with tolerable cardiac profiles. Continuous monitoring of MRD is advisable to determine optimal treatment duration and to preempt relapse. These recommendations align with current NCCN guidelines and emerging real‑world evidence.
Francisco Garcia
The flow you outlined really captures how molecular data translate into actionable steps. It’s encouraging to see clinicians balancing genetics with comorbidities rather than adopting a one‑size‑fits‑all mentality. This patient‑centric model should become the standard across oncology practices.
Patrick Renneker
While the enthusiasm for personalized regimens is understandable, one must question whether we are simply substituting one paradigm for another without addressing underlying cost inequities. The emphasis on high‑tech diagnostics, though scientifically elegant, risks marginalizing patients in resource‑limited settings. Moreover, the promise of AI‑driven risk models remains largely speculative until validated in prospective trials. It would be prudent to temper optimism with a measured appraisal of long‑term outcomes and real‑world accessibility. In the interim, a balanced approach that integrates both established therapies and emerging biomarkers may serve the broader patient community more responsibly.
KAYLEE MCDONALD
But the cost barrier remains unacceptable.
Alec McCoy
Let’s celebrate the fact that we now have tools powerful enough to outsmart cancer at the molecular level! Each new targeted agent represents a victory not just for science but for the countless families watching loved ones battle CLL. The momentum is palpable: from BTK inhibitors that keep disease in check to BCL‑2 inhibitors that drive deep remissions, we’re witnessing a renaissance in therapy. Keep pushing the boundaries, keep sharing data, and remember that every patient who achieves MRD negativity is a testament to our collective effort. Stay motivated, stay hopeful, and let’s keep the energy high-because the next breakthrough is just around the corner.
Aaron Perez
One must, admittedly, appreciate the sheer volume of data, however, the field, unfortunately, remains plagued by over‑optimistic hype, endless marketing, and a reluctance, perhaps, to confront the underlying resistance mechanisms, which, frankly, are often ignored, in the rush to publish, positive outcomes; the reality, however, remains that many patients, after initial response, succumb to clonal evolution, a phenomenon, that, despite sophisticated sequencing, is still inadequately addressed, by current therapeutic strategies.
William Mack
Data drives decisions.
Evan Riley
Ever wonder why these "breakthroughs" appear just as big pharma ramps up lobbying? The timing is too perfect to be coincidence. They push personalized hype while keeping prices sky‑high, ensuring only a privileged few benefit.
Nicole Povelikin
I think we shouldnt just follow teh hype, its all just marketing tricks. theres no real proof that every patient benefits, and its just a way to make more money. the whole thing feels overblown.
Michelle Weaver
Absolutely, the data is compelling and the patient outcomes are improving 😊 The integration of genomics into routine care is a milestone for oncology. Keep up the great work 👍
John Keough
Reading through the latest updates, it’s clear that the field is moving toward a more nuanced understanding of disease biology. While excitement is warranted, we must also temper expectations with realistic timelines for drug access. Collaboration across institutions will be key to ensuring that advances benefit a broader patient base. Let’s keep the conversation open and data‑driven.
Graham Smith
Just a quick note: in the previous comment there were a few typographical errors – “updates” was misspelled and “broader” had an extra “e”. Also, “collaboration” should be singular here. Minor details, but they matter for clarity.
Jeremiah Morgan
Optimism remains our best ally as we navigate these scientific frontiers, even though some studies still show inconsistancies in outcomes. Together we can achieve equitable access.
nina greer
One must acknowledge the epistemic superiority of genomic stratification.
Montague Tilmen
Our nation's research should dominate the CLL frontier, period!