Medication Restart: What It Means and When It’s Safe to Start Again
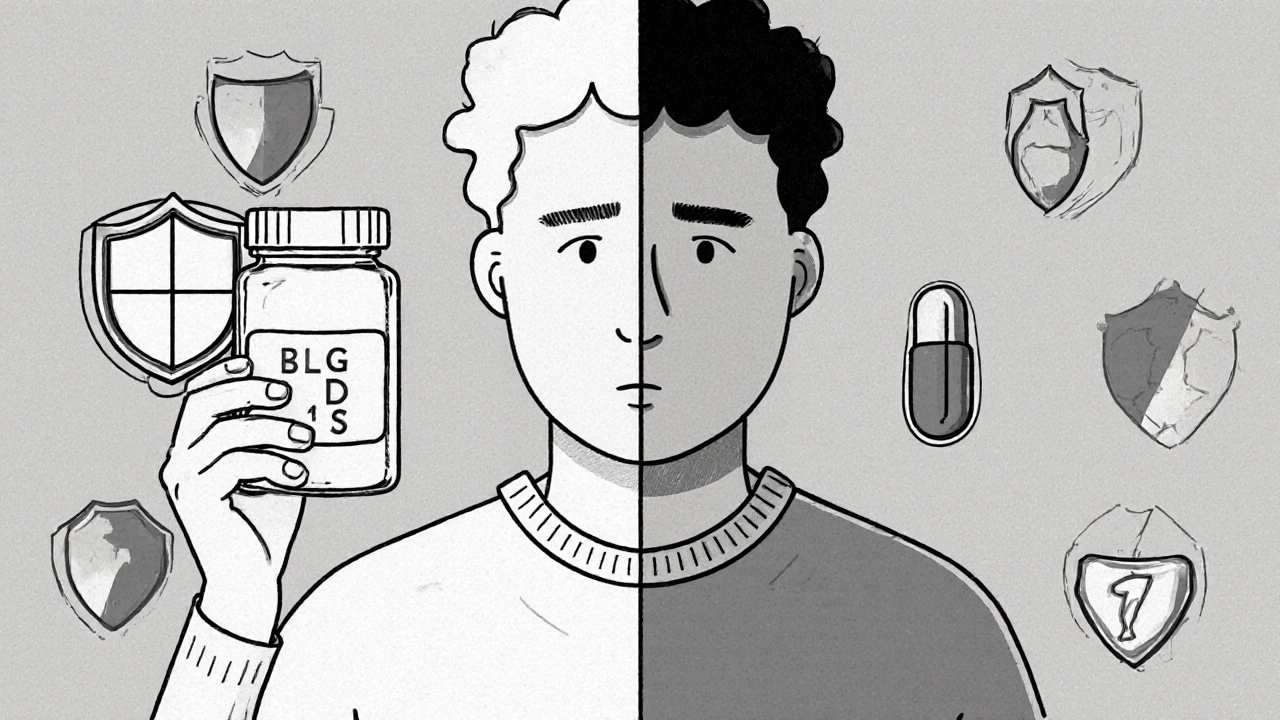
When you stop a medication—whether by accident, because of side effects, or because your doctor told you to—medication restart, the process of resuming a drug after a break. Also known as reinitiation, it’s not as simple as picking up where you left off. Many people assume that if a drug worked before, it’ll work the same way now. But your body changes. So do your health conditions, other meds, and even your liver’s ability to process things. Restarting without checking in can lead to dangerous side effects, failed treatment, or worse.
Take antidepressants, medications used to treat depression and anxiety. Stopping them suddenly can cause withdrawal. Restarting too fast can trigger serotonin syndrome. Or consider blood thinners, drugs like warfarin or apixaban that prevent clots. If you stopped them after surgery and now want to restart, your risk of bleeding or clotting depends on how long you were off, why you stopped, and what else you’re taking. Even something as common as thyroid medication, like levothyroxine for hypothyroidism—if you missed doses for weeks and then restart, your heart might not handle the sudden change.
What you’ll find below isn’t theory. It’s real stories from people who restarted meds and what happened next. Some got better. Some ended up in the ER. These posts break down exactly when restarts work, which drugs need a slow reintroduction, how to spot warning signs, and what questions to ask your doctor before you take that first pill again. You’ll see how medication restart ties into drug interactions, dosing errors, and why timing matters more than you think. Whether you’re coming off a painkiller, an antibiotic, or a chronic condition drug, the advice here is practical, no-fluff, and based on what actually happens in clinics and homes—not just textbooks.