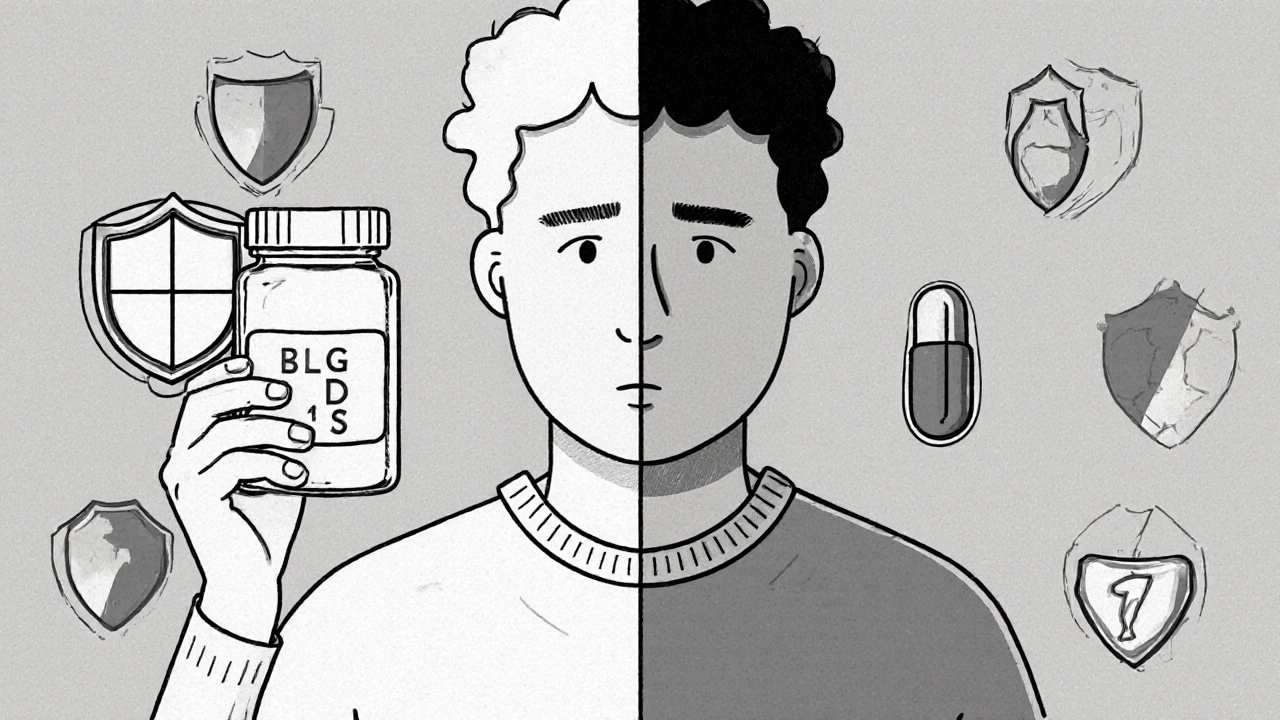
Restarting a medication after taking a break can be deadly-even if you were taking it safely before. It’s not about being careless. It’s about your body changing. When you stop a drug like an opioid, benzodiazepine, or even certain antidepressants, your body forgets how to handle it. The tolerance you built? Gone. In days. Sometimes even hours. But your brain still remembers the dose that used to work. That’s where the danger lies.
Why Your Body Can’t Handle the Same Dose Anymore
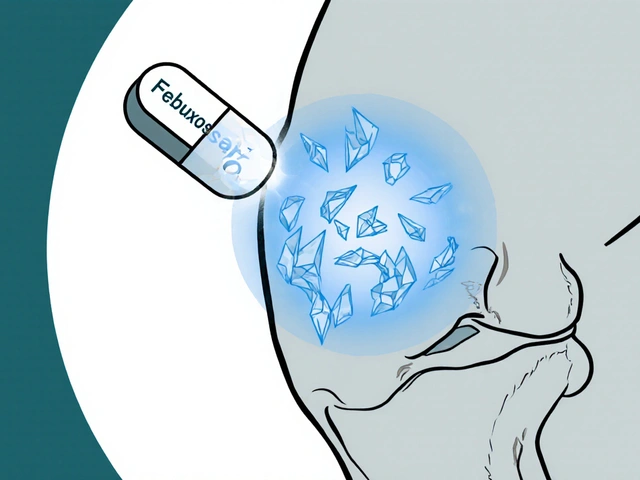
Think of tolerance like a shield. When you take a medication regularly, your body adjusts. It builds defenses against its effects. But when you stop, those defenses fade fast. For opioids like oxycodone or heroin, tolerance drops within 3 to 5 days. For methadone, it’s about a week. Benzodiazepines like Xanax? Just a few days. Your liver doesn’t metabolize it as quickly anymore. Your brain receptors don’t respond the same way. But if you take the same dose you used to, your body has no defense left.
This isn’t theoretical. In 2022, Washington State’s health department found that 62% of fatal opioid overdoses happened within 72 hours after someone left jail, a treatment center, or the hospital-places where they were forced to stop using. One man in Perth, who’d been off oxycodone for 10 days after surgery, took his old 40mg tablet because he was still in pain. He stopped breathing. He survived, but only because his sister had naloxone on hand.
It’s not just opioids. People restarting antidepressants like paroxetine or venlafaxine after a break have ended up in the ER with serotonin syndrome. Those on MAOIs need to wait weeks before switching to other meds, or they risk a deadly spike in serotonin. Even quetiapine, used for sleep or bipolar disorder, can cause dangerous drops in blood pressure if restarted at the old dose.
The Only Safe Way: Start Low, Go Slow
There’s one rule that saves lives: start low, go slow. That means restarting at a fraction of your old dose-not 50%, not 75%, but often 25% or even less. For opioids, Washington State guidelines say begin at 25-50% of your previous daily dose. For quetiapine, start at 25mg. For benzodiazepines, start with a quarter of your old dose and wait 3-5 days before increasing.
Here’s how it works in practice:
- Find out your last dose before the break. Write it down.
- Calculate 25% of that dose. That’s your new starting point.
- Take that small dose once a day. Wait at least 24 hours.
- Only increase if you feel no side effects-no dizziness, no extreme sleepiness, no trouble breathing.
- Wait another 2-3 days before the next small increase.
- Never rush. It’s not a race. It’s a rescue mission.
One woman in Adelaide restarted her clonazepam after a 12-day break. She took 0.5mg instead of her old 2mg. She felt nothing. On day four, she went up to 0.75mg. By day 10, she was back to 1mg-with no issues. She didn’t need to go back to 2mg. Her body had re-adapted at a lower level.
Medical Supervision Isn’t Optional-It’s Essential
Restarting alone is risky. Even if you think you know your body, you don’t. Your liver changes. Your kidneys change. Your sleep, stress, and diet affect how drugs are processed. That’s why medical supervision isn’t a luxury-it’s a necessity.
Hospitals and clinics with formal restart protocols have 87% success rates. Those without? Only 42%. That’s not a small gap. That’s life or death.
Ask your doctor or pharmacist:
- Is this medication still necessary? Maybe you don’t need it anymore.
- What’s the safest starting dose based on how long I was off?
- Do I have any other meds that could interact dangerously?
- Should I get naloxone before restarting?
Many doctors skip this conversation because they assume you’re still on the drug. Don’t let them assume. Say it clearly: “I stopped this for X weeks. I need to restart safely.”

What to Watch For-Signs of Overdose
Even with a low dose, overdose can happen fast. Know the warning signs:
- Slowed or shallow breathing (less than 12 breaths per minute)
- Unresponsiveness-you can’t wake the person up
- Pinpoint pupils (tiny dots in the center of the eyes)
- Blue lips or fingernails
- Extreme drowsiness or confusion
- Cold, clammy skin
If you see any of these, act immediately. Call emergency services. Give naloxone if you have it. Don’t wait. Don’t hope it passes. This isn’t a bad trip. This is a medical emergency.
Naloxone isn’t just for heroin users. It works on any opioid-oxycodone, fentanyl, tramadol-even if you’re taking it for pain. And it’s safe. It won’t hurt you if you don’t have opioids in your system.
Don’t Mix Medications-Especially With Alcohol or Sleep Aids
One of the deadliest mistakes? Combining your restarted medication with alcohol, sleeping pills, or even over-the-counter cold meds. These all slow your breathing too. Together, they multiply the risk.
Washington State’s overdose data shows that 81% of fatal opioid restarts involved another sedating substance. One man restarted his hydrocodone after a month off. He took a Tylenol PM for sleep. He didn’t wake up. The combination of the opioid and diphenhydramine crushed his breathing.
Check every pill you take. Even melatonin, muscle relaxers, or antihistamines can be dangerous. Ask your pharmacist: “Is this safe to take with [medication name] after a break?”

Special Cases: MAOIs, Antidepressants, and Withdrawal
Some medications need longer waits. MAOIs (like phenelzine or tranylcypromine) require a 14-day washout before starting SSRIs or SNRIs. Restarting too soon can trigger serotonin syndrome-a condition that causes high fever, seizures, and heart rhythm problems.
For antidepressants like sertraline or fluoxetine, restarting after a short break (a few days) is usually fine at your old dose. But after weeks or months? Start low. Your brain’s serotonin receptors are sensitive again. A full dose can cause agitation, nausea, or even suicidal thoughts in some people.
And if you’re restarting after detox or rehab? Your tolerance is near zero. Your risk is highest. That’s why programs like Evoke Wellness in Texas now require naloxone training and a supervised restart plan before discharge.
What You Can Do Right Now
You don’t need to wait for a doctor’s appointment to protect yourself. Here’s your action plan:
- Write down the name of your medication and your last dose.
- Calculate 25% of that dose.
- Call your doctor or pharmacist and say: “I’m restarting [medication]. I need a safe starting dose and a plan.”
- Ask for naloxone. If they say no, ask why. It’s not just for addicts-it’s for anyone restarting opioids.
- Tell a trusted friend or family member what you’re doing. Give them naloxone and instructions.
- Don’t use alone. Have someone nearby for the first few days.
If you’re in Australia, call the Alcohol and Drug Foundation at 1300 858 584. They can connect you with local services. If you’re in a rural area, ask your local pharmacy-they’re often the first line of defense.
What’s Changing in 2025
The FDA just released new draft guidelines for restarting opioids after interruption. The American Society of Addiction Medicine rolled out a 10-point scoring system in early 2024 to calculate safe restart doses based on your history, how long you were off, and your health conditions.
And now, wearable monitors are in trials that detect dangerous breathing patterns and auto-administer naloxone. They’re not everywhere yet-but they’re coming.
For now, the best tool you have is knowledge. And the most powerful action you can take is to start low.
Can I restart my medication on my own if I feel fine?
No. Feeling fine doesn’t mean your body is ready. Tolerance drops faster than you think. Even if you feel okay, your breathing and heart rate may be dangerously suppressed. Always restart under medical guidance, even if you think you know your limits.
How long does it take to lose tolerance to opioids?
Tolerance to short-acting opioids like oxycodone or heroin can drop in as little as 3-5 days. For methadone, it takes about 7-10 days. After that, your body can’t handle your old dose. The risk of overdose spikes dramatically.
Do I need naloxone if I’m restarting an antidepressant?
No, naloxone doesn’t work on antidepressants. But if you’re restarting an opioid-any opioid, even tramadol or codeine-you need naloxone. It’s not about addiction. It’s about safety. Keep it with you and make sure someone else knows how to use it.
What if I accidentally take my old dose?
If you’ve taken your old dose and feel dizzy, sleepy, or have trouble breathing, call emergency services immediately. Don’t wait. Use naloxone if you have it. Even if you feel okay now, effects can build over hours. Get checked out.
Is it safe to restart medication after a hospital stay?
Not without a plan. Hospitals often stop medications during admission, and tolerance drops fast. Always ask for a restart protocol before discharge. If they don’t give you one, insist. Your life depends on it.



Douglas Fisher
Wow. Just... wow. I’ve been through this twice-once with oxycodone after surgery, once with clonazepam after a mental health hospitalization. I didn’t know my body could forget so fast. I took my old dose thinking, ‘I’ve done this a hundred times.’ I didn’t even make it to the couch before my vision went gray. I woke up in the ER. Naloxone saved me. I’m still alive because my sister had it. Please-don’t be like me. Start low. Even if you feel fine. Your body isn’t lying-it’s just quiet.
Vanessa Carpenter
This is the kind of post that should be mandatory reading for anyone who’s ever taken meds for more than a few weeks. I’m a nurse, and I’ve seen too many people get discharged from hospitals with zero guidance on restarting. It’s not negligence-it’s systemic laziness. But you? You’re doing the right thing by learning this now. Keep sharing. Someone’s life might depend on it.
Bea Rose
Start low. Go slow. That’s it. No fluff. No drama. Just facts. If you don’t do this, you’re gambling with your brainstem. And you’re not a gambler. You’re someone who wants to live.
Michael Collier
It is imperative to underscore the clinical significance of pharmacokinetic and pharmacodynamic changes following medication discontinuation. The physiological recalibration of hepatic enzyme activity, receptor sensitivity, and neurochemical homeostasis occurs with remarkable speed-often within seventy-two hours. Consequently, the reinstatement of previously tolerated dosages constitutes a significant and potentially lethal pharmacological misalignment. Medical oversight is not merely advisable; it is a non-negotiable component of patient safety.
Shannon Amos
So let me get this straight… you’re telling me I can’t just take my old 20mg of quetiapine because I ‘felt like it’ after a week off? And I’m supposed to start at 25mg? Like I’m a baby? 😒 Well… guess what? I did that. And I didn’t die. So… thanks, I guess? 🤷♀️
Wendy Edwards
I was so scared to restart my antidepressant after 6 weeks off. I thought I’d be fine-I’m strong, right? But I got so dizzy I threw up. My heart felt like it was trying to escape my chest. I cried for an hour. Then I called my pharmacist and asked for help. She told me to drop to 10mg. I did. And now? I’m okay. Not perfect. But okay. You’re not weak for needing help. You’re brave for asking. I’m proud of you for reading this. You’re already doing better than you think.
Jaspreet Kaur
Life is not a race to feel normal again. It’s a quiet return to balance. The body remembers more than the mind. It holds space for what was lost. To rush is to betray that memory. To wait is to honor it. Start low. Not because you’re broken. But because you’re alive. And life deserves patience.
Gina Banh
Stop saying ‘I feel fine.’ That’s the lie that kills. Your liver doesn’t care how you feel. Your receptors don’t care about your willpower. If you restarted an opioid after 10 days off and didn’t start at 25%? You’re already in danger. And if you’re reading this and thinking ‘I’m not an addict’-good. That’s why you need naloxone even more. It’s not stigma. It’s science. Get it. Now.
Deirdre Wilson
I never thought about how my body ‘forgets’ meds. Like… it’s not like forgetting your keys. It’s more like your body turns off a light switch and then you flip it back on full blast. Boom. Lights explode. That’s what overdosing feels like. I’m starting my meds at 25% now. And I told my dog. He’s my witness. He doesn’t judge. He just lies on my lap. That’s enough.
Ryan C
Correction: The FDA hasn’t released final guidelines yet-only draft ones. Also, naloxone doesn’t work on tramadol unless it’s the opioid component you’re overdosing on. And serotonin syndrome isn’t caused by restarting SSRIs alone-it’s when you combine them with MAOIs or other serotonergics. Also, your 25% rule is good, but for methadone, it’s more like 10-20%. You’re mostly right, but details matter. 📊✅
Stephanie Deschenes
Thank you for writing this. I’ve been silent about my restart after 8 months off benzodiazepines. I started at 0.25mg. Took 3 weeks to get back to 0.5mg. No panic. No tremors. Just quiet healing. I didn’t tell anyone. I didn’t need to. But I’m telling you now-because you’re not alone. And you’re not broken. You’re rebuilding.
Cynthia Boen
This post is just a PSA for people who don’t want to take responsibility. You think your body ‘forgets’? No. You just got lazy. Stop taking meds if you can’t handle them. Stop pretending you need them. It’s not ‘safety’-it’s dependency culture. Start low? Just don’t start at all.