When a patient walks into a clinic with a prescription for a brand-name drug that costs $150 a month, they’re not just facing a medical decision-they’re facing a financial one too. Many don’t realize that a generic version of the same drug might cost less than $20. The gap isn’t just in price. It’s in understanding. And that’s where healthcare providers play a critical role-not just as prescribers, but as advocates.
Why Generic Medications Matter More Than Ever
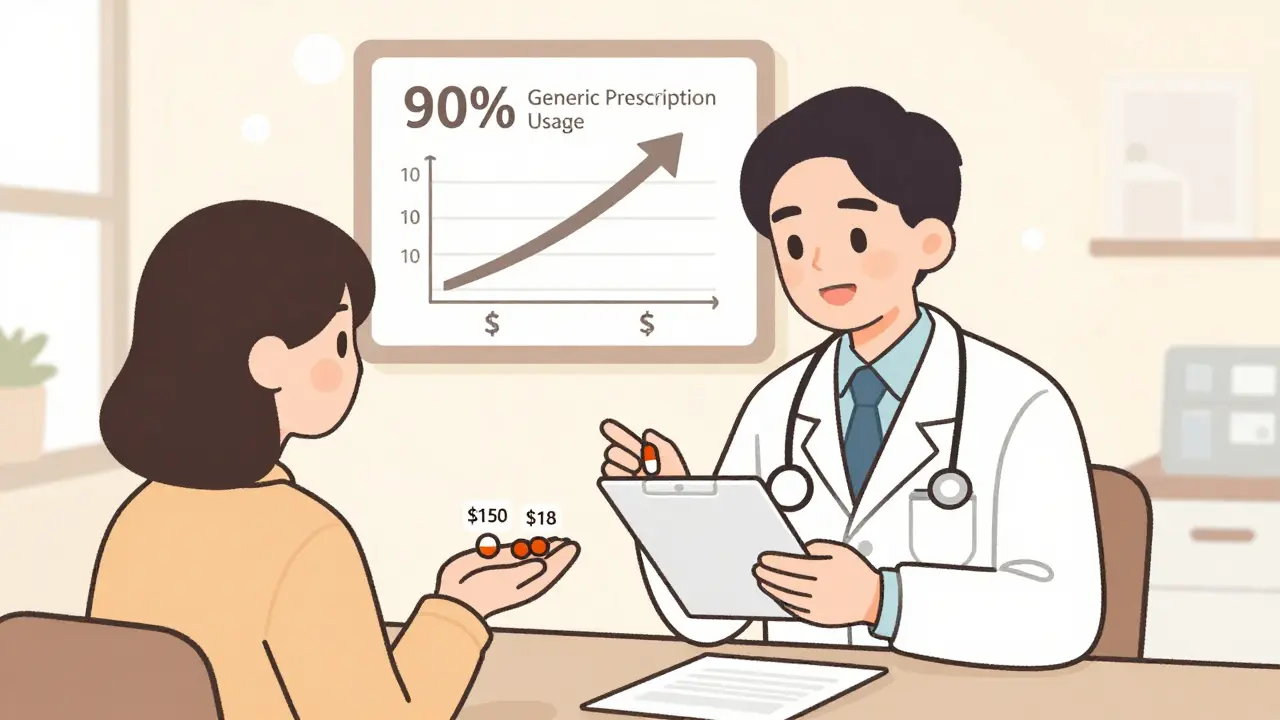
Generic drugs aren’t second-rate. They’re the same medicine, approved by the FDA, with the same active ingredients, strength, and dosage form as their brand-name counterparts. The only differences? Inactive ingredients like fillers or dyes, and the price. A generic version typically costs about 15% of the original brand price within a year of launch. In 2022, generics made up 90% of all prescriptions filled in the U.S.-but only 23% of total drug spending. That’s billions saved every year. Yet, despite these numbers, patients still hesitate. Why? Because they’ve been told-sometimes by well-meaning friends, sometimes by misleading ads-that generics are weaker, less safe, or "not as good." A 2015 review in the PMC found that while trust in generics has improved, a stubborn belief persists: "If it looks different, it must be different." And when a patient’s pill changes color or shape after a refill, confusion sets in. That’s when they stop taking it.The Real Cost of Not Using Generics
The financial burden isn’t just on patients-it’s on the whole system. When someone can’t afford their medication, they skip doses. They delay refills. They abandon therapy altogether. Data from the Association for Accessible Medicines shows that new patient abandonment rates are 266% higher for brand-name drugs than for generics. Why? Because 90% of generic copays are under $20. Meanwhile, 61% of brand-name copays exceed that threshold. For someone managing high blood pressure, diabetes, or depression, skipping doses isn’t just inconvenient-it’s dangerous. A missed dose can mean a trip to the ER, hospitalization, or long-term complications. Providers who don’t address cost aren’t just missing a chance to save money-they’re missing a chance to save lives.What Providers Are Saying
The American College of Physicians (ACP) made it official in 2022: "Doctors should prescribe generic medications whenever possible." The American Academy of Family Physicians (AAFP) agrees-but with a caveat. They oppose mandatory substitution because some drugs, like those with a narrow therapeutic index (NTI), need careful monitoring. Warfarin, levothyroxine, and certain seizure meds fall into this category. Even here, though, the goal isn’t to block generics-it’s to ensure the switch is done safely, with proper follow-up. Pharmacists, who often have the most direct contact with patients, are on the front lines. They see the confusion firsthand. A patient might say, "This pill looks different. Is this the same?" That’s not a challenge-it’s an opening. A quick explanation can turn fear into confidence.
How to Talk About Generics Without Sounding Like a Salesperson
You don’t need a script. You need honesty and clarity. Start by normalizing it: "Many of my patients take this same medication in its generic form. It’s just as effective, and it’s much more affordable." Then, anticipate the next question: "But it looks different." Explain why: "The active ingredient is the same, but the filler or color might change depending on the manufacturer. That doesn’t affect how it works. The FDA requires every generic to meet the same safety and effectiveness standards as the brand." Use numbers. "Your brand-name version costs $140 a month. The generic is $18. That’s $1,464 saved every year. That’s a new pair of shoes, a month of public transport, or groceries for your family." Don’t wait for the patient to ask. Proactively mention generics during the initial prescription. Say: "I’m prescribing the generic version of this drug because it’s just as effective and will save you a lot of money. If you have any questions later, let me know."Barriers Providers Face-and How to Overcome Them
Time is the biggest obstacle. Primary care visits average just 13 to 16 minutes. Adding a 30-second explanation about generics feels like a luxury. But here’s the truth: skipping that conversation costs more time later. A patient who stops taking their meds because they’re confused or can’t afford them will need follow-up calls, repeat visits, or worse-emergency care. Electronic health records (EHRs) are starting to help. Some now flag when a brand-name drug has a cheaper generic alternative, showing the exact copay difference at the point of prescribing. Use those alerts. They’re there for a reason. Another barrier? Fear of pushback. Some patients insist on the brand. That’s okay. Listen. Ask: "What concerns you about the generic?" Sometimes, it’s not about the drug-it’s about control. If they’ve been on the same brand for years, switching feels risky. Acknowledge that: "I get it. You’ve been on this for a long time. Let’s talk about why switching might be safe-and how we’ll watch for any changes."When Generics Aren’t the Answer
Not every drug should be switched. NTI drugs require special attention. If a patient is stable on a brand-name version of levothyroxine, switching to a different generic every few months can cause hormone fluctuations. In those cases, the goal isn’t to force substitution-it’s to ensure consistency. Some providers request "dispense as written" on the prescription. Others work with pharmacies to stick with one generic manufacturer. Also, watch for price spikes. In early 2023, the American Society of Health-System Pharmacists warned that some essential generics-like insulin, certain antibiotics, and blood pressure meds-had become unaffordable due to supply chain issues and consolidation. Advocacy now includes checking prices before prescribing. If a "generic" is now $100, you need to know. Don’t assume it’s cheap.
The Bigger Picture: Generics Are Just the Start
This isn’t just about pills. It’s about trust. When patients see their provider actively working to reduce their costs without sacrificing care, it builds a deeper relationship. It says: "I’m not just treating your condition-I’m thinking about your life." It also opens the door to other conversations: Are you filling your prescriptions? Are you taking them as directed? Are you worried about side effects? When patients feel heard, they’re more likely to speak up. And it’s not just for adults. Parents managing their child’s ADHD medication, elderly patients juggling five prescriptions, young adults with chronic asthma-all benefit when providers make affordability part of the conversation.What You Can Do Tomorrow
You don’t need a policy change or a new system. Start small:- Check your EHR for generic alternatives before prescribing.
- Add a line to your standard script: "This is available as a generic that costs significantly less."
- Keep a printed one-pager on generics in your exam rooms-simple, clear, in plain language.
- Ask your pharmacy if they can notify you when a generic price spikes.
- Don’t assume patients know. Many think "generic" means "inferior." Correct that myth, gently.
Final Thought: Advocacy Isn’t Optional
Healthcare providers are the most trusted source of medical information. Patients believe you. That’s not a power-it’s a responsibility. When you choose a generic, you’re not just cutting costs. You’re removing a barrier to care. You’re helping someone take their medicine. You’re helping them stay healthy. The science is clear. The data is clear. The ethical obligation is clear. The only thing left is to speak up.Are generic medications really as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove bioequivalence-meaning they work the same way in the body, with absorption rates falling within 80% to 125% of the brand. Thousands of studies confirm they’re equally effective. The only differences are in inactive ingredients like dyes or fillers, which don’t affect how the drug works.
Why do generic pills look different from brand-name ones?
By law, generic manufacturers can’t copy the exact appearance of brand-name drugs to avoid trademark infringement. So they use different shapes, colors, or markings. But these changes are only cosmetic. The active ingredient-and how your body absorbs it-is identical. Many patients worry when their pill looks different, but it’s not a sign of lower quality. It’s just a different manufacturer.
Can I trust generics for chronic conditions like high blood pressure or diabetes?
Absolutely. Generics are widely used for chronic conditions. In fact, most patients on long-term medications take generics. Studies show no difference in outcomes for conditions like hypertension, diabetes, or depression when switching from brand to generic. The key is consistency-if a patient is stable on a particular generic, avoid switching manufacturers unless necessary, especially for drugs with narrow therapeutic windows like levothyroxine or warfarin.
Why do some doctors still prescribe brand-name drugs?
Sometimes, it’s because the patient has had a bad experience with a generic in the past-often due to switching between different generic manufacturers. Other times, it’s because the doctor isn’t aware of the cost difference or assumes the patient prefers the brand. In rare cases, for drugs with a narrow therapeutic index, a provider may choose to stick with one version to avoid fluctuations. But for most medications, the brand offers no clinical advantage.
What if my patient refuses to take a generic?
Listen first. Ask why. Is it cost? Fear? A past experience? Don’t argue. Explain the science simply: "The FDA requires generics to be just as safe and effective. The only difference is the price-often 85% less." Offer to check the copay together. If they still refuse, document the conversation and respect their choice. But don’t stop advocating. Sometimes, a patient changes their mind after seeing the actual price at the pharmacy.
Are there times when I shouldn’t prescribe a generic?
Yes-for drugs with a narrow therapeutic index (NTI), where small changes in blood levels can cause serious side effects. Examples include warfarin, levothyroxine, phenytoin, and cyclosporine. For these, it’s best to stick with one manufacturer once a stable dose is found. Some providers request "dispense as written" on the prescription. But even here, switching between generics isn’t automatically unsafe-it just requires closer monitoring.
How do I know if a generic price has gone up?
Check your EHR-it may flag price changes. Ask your pharmacy for updates. Some health systems now provide real-time cost tools at the point of prescribing. Also, watch for alerts from organizations like ASHP, which have warned about price spikes in essential generics like insulin or certain antibiotics. If a "generic" now costs more than $50, question why and consider alternatives.
Does prescribing generics save the healthcare system money?
Yes-massively. In 2022, generics saved the U.S. healthcare system over $370 billion. That’s money that can be redirected to care, infrastructure, or patient support services. Every time you prescribe a generic instead of a brand, you’re reducing financial strain on patients, insurers, and public programs like Medicare and Medicaid.




Andy Thompson
lol so now the FDA is in on the big pharma cover-up? 🤡 generics are just the placebo version they give you so you don't notice the real medicine is being hoarded for the elites. I heard the active ingredient is replaced with chalk and government microwaves. 💀
sagar sanadi
generic = bad. brand = good. why? because brand has logo. logo = trust. no logo = scam. america good. india bad. generics from india? no thanks. 🤡
Thomas Varner
I mean... I get it. I really do. But I’ve seen people switch to generics and then get weird side effects-like, not the drug’s fault, but the fillers? Who even knows what’s in those? 🤔 And then they blame the doctor. It’s messy. I just wish there was more transparency.
Art Gar
The ethical imperative to prescribe generics is not predicated upon cost reduction alone, but upon the fiduciary responsibility of the physician to maximize therapeutic efficacy while minimizing financial burden. The data presented is statistically robust, yet the ethical framework must remain unassailable.
clifford hoang
They say generics are the same... but have you ever looked at the patent expiration dates? 🤫 The FDA is basically a puppet for Big Pharma. They let generics in... just enough to make you think you're saving money... while the real profit is in the refill cycles and insurance kickbacks. 🧠👁️🗨️ We're all lab rats in a price-gouging maze.
Carolyn Rose Meszaros
I had a patient cry last week because she couldn’t afford her brand-name insulin. When we switched her to a generic, she said, 'I didn’t think they’d let me live this long.' 😔 I’ll never stop pushing for generics. It’s not just medicine-it’s dignity.
Greg Robertson
I’ve been prescribing generics for 15 years. Most patients don’t even notice. But when they do ask? I just say, 'Same pill, less money.' Simple. Works every time. 🤝
Nadia Watson
I work in a community clinic and we have a one-pager on generics in every room. We don't use the word 'cheap'-we say 'equivalent' and 'affordable'. One elderly woman said, 'So it's not a knockoff? Like my fake purse?' We laughed. Then she took it. 🌍
Shane McGriff
I used to think generics were just fine... until my mom switched from her brand-name thyroid med and started having panic attacks. Turned out the filler in that batch was triggering her anxiety. We went back. She’s stable now. So yeah-generics are usually fine. But don’t treat them like they’re all the same. Monitoring matters.
Jacob Cathro
Bro, this whole post is just a corporate shill for CVS and Walmart. 'Generic = good'? Nah. They're just the placebo version of the placebo. The real profit is in the 1000% markup on the brand-name stuff that no one ever takes anyway. 🤡 #BigPharmaLies
Paul Barnes
The assertion that generics are always equivalent is misleading. Bioequivalence standards permit up to a 25% variance in absorption rates, which can be clinically significant for drugs with narrow therapeutic indices. Prescribing decisions must account for individual pharmacokinetic variability, not just cost.