Drinking a glass of pomegranate juice in the morning might feel like a healthy habit-rich in antioxidants, sweet without added sugar, and packed with nutrients. But if you're taking medication, especially for heart conditions, blood thinning, or mental health, that glass could be doing more than just boosting your immune system. It might be changing how your body processes your pills. And that’s not something to take lightly.
Why Pomegranate Juice Can Interfere With Your Meds
Pomegranate juice doesn’t just sit in your stomach and get digested. It hits your liver and intestines, where a group of enzymes called cytochrome P450-specifically CYP3A4 and CYP2C9-do the heavy lifting of breaking down most medications. These enzymes are like molecular scissors, cutting drugs into smaller pieces so your body can eliminate them safely. But pomegranate juice? It throws a wrench in that process. Studies show that compounds in pomegranate juice, like punicalagins and ellagitannins, can block these enzymes. When that happens, your body can’t break down certain drugs as quickly. That means more of the drug stays in your bloodstream longer than it should. For some medications, even a small increase in concentration can lead to side effects-or worse, toxicity. This isn’t theoretical. The warfarin connection is the most documented. Warfarin is a blood thinner with a narrow therapeutic window: too little, and you’re at risk of clots; too much, and you could bleed internally. Case reports show people on warfarin who started drinking pomegranate juice daily saw their INR (a measure of blood clotting time) jump by 0.5 to 1.5 units. One Reddit user reported their INR soaring from 2.4 to 4.7 in just three days after adding pomegranate juice to their routine. That’s a dangerous spike. It’s not universal-some people see no change-but enough people have had real reactions that doctors now treat this as a real risk.Which Medications Should You Worry About?
Not all drugs are affected equally. The biggest red flags are medications that are:- Metabolized primarily by CYP3A4 or CYP2C9 enzymes
- Have a narrow therapeutic index (small difference between effective and toxic dose)
- Are taken daily, long-term
- Warfarin (Coumadin, Jantoven): The most studied. Risk of increased bleeding.
- Statins (atorvastatin, simvastatin): Can lead to muscle damage or liver issues if levels build up.
- Calcium channel blockers (amlodipine, felodipine): May cause low blood pressure or dizziness.
- Some antidepressants (sertraline, escitalopram): Risk of serotonin syndrome or excessive sedation.
- Immunosuppressants (cyclosporine, tacrolimus): Can cause kidney damage if levels rise.
- Some anti-seizure drugs (phenytoin): May increase seizure risk or toxicity.
The Science Is Mixed-So What Should You Believe?
Here’s where it gets confusing. Lab studies (in vitro) show strong enzyme inhibition. One study found pomegranate juice blocked up to 50% of CYP2C9 activity. That sounds alarming. But human trials? Not so much. A 2014 study with 12 healthy volunteers gave them pomegranate juice daily for two weeks and then measured how their bodies handled midazolam, a drug known to be broken down by CYP3A4. Result? No change in drug levels. The same study looked at other markers-nothing significant. Other trials on theophylline (used for asthma) and even warfarin in larger groups found minimal to no effect. So why the disconnect? Because lab tests use concentrated extracts. Real juice has dilution, varying sugar content, and different growing conditions. Plus, people metabolize things differently. Your genetics, liver health, gut bacteria, and even what else you eat that day can change how your body reacts. Dr. David Mischoulon, a psychiatrist and researcher at Massachusetts General Hospital, put it bluntly: “Lab data are insufficient grounds upon which clinical decisions may be based.” He’s not saying it’s safe-he’s saying we don’t have enough solid human evidence to make blanket rules.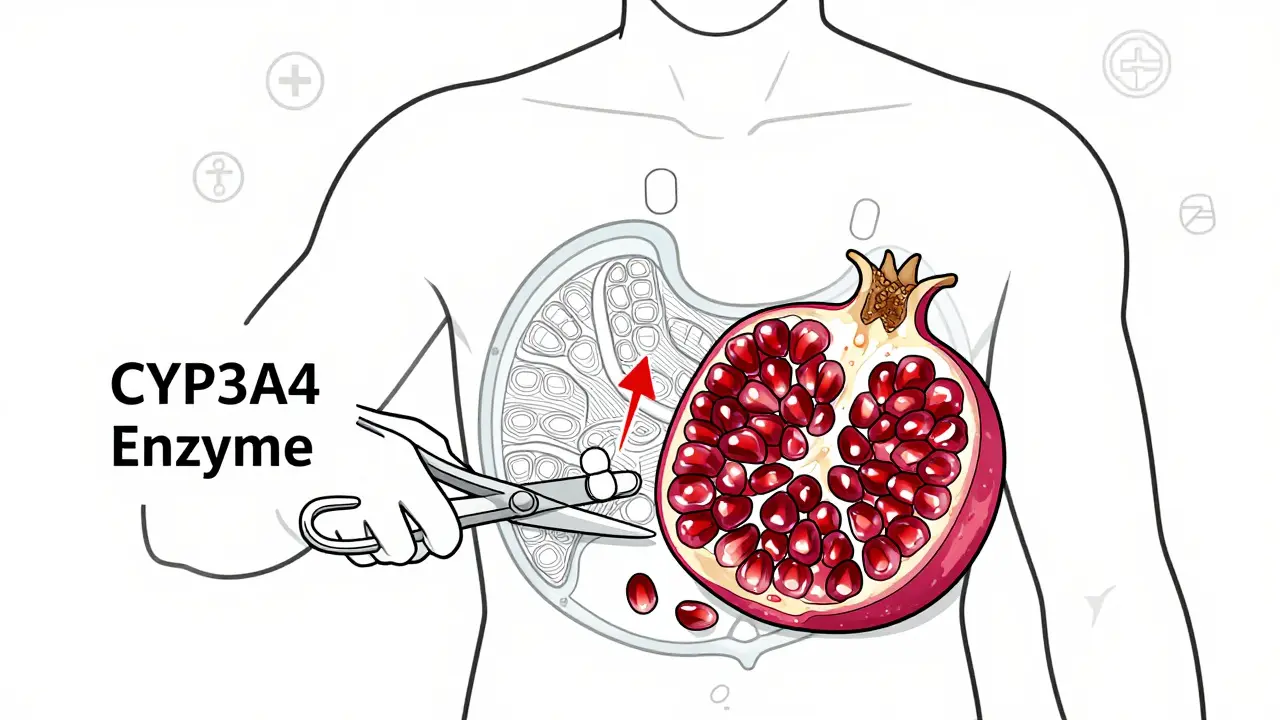
What Do Experts Actually Recommend?
Despite the mixed science, major health organizations aren’t ignoring the risk. Here’s what they’re telling patients right now:- Mayo Clinic (2023): Avoid more than 8 ounces of pomegranate juice per day if you’re on warfarin. Keep your intake consistent-don’t start or stop suddenly.
- American Heart Association (2021): Don’t eliminate pomegranate juice entirely. Abrupt changes in diet can be riskier than steady, moderate use.
- University of North Carolina Pharmacy (2020): Wait at least two hours between taking your medication and drinking pomegranate juice. That gives your body time to absorb the drug before the juice hits your system.
- European Medicines Agency (2022): For most drugs, the risk is low. But for warfarin? Increase INR monitoring when you start drinking it.
Real People, Real Stories
Online communities are full of mixed experiences. On r/bloodthinners, 17 users reported INR spikes linked to pomegranate juice. One man had to cut his warfarin dose by 30% after his INR hit 4.7. Another woman had nosebleeds and bruising she couldn’t explain until she remembered she’d started drinking juice every day. But flip over to PatientsLikeMe, and 89% of 214 users said they drank pomegranate juice daily with no issues. One woman wrote: “I’ve had two pomegranates a day for five years. My INR is perfect. My doctor never even mentioned it.” That’s the problem. It’s not the same for everyone. Genetics matter. Some people have a CYP2C9 variant that makes them extra sensitive. Others clear the compounds fast. You can’t predict it without testing.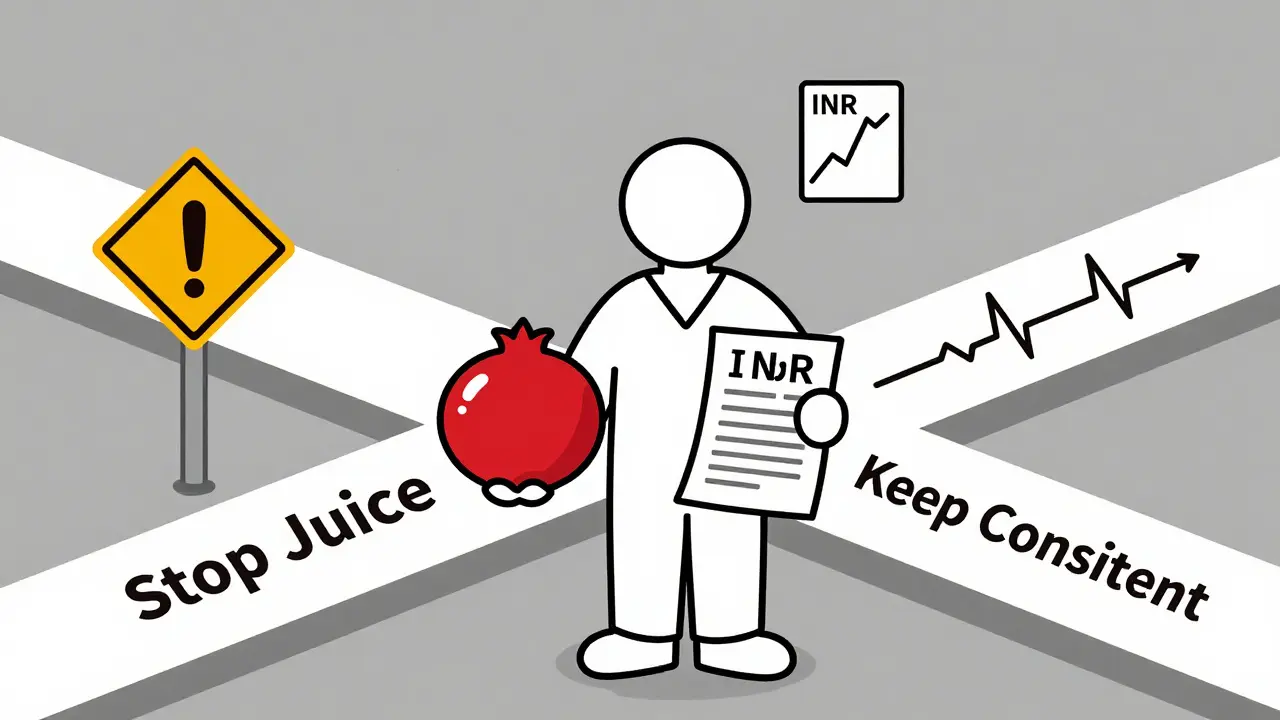
What Should You Do?
If you’re on medication and you like pomegranate juice, here’s your simple action plan:- Check your meds. Look up your prescriptions on a trusted interaction checker like Mayo Clinic’s or WebMD’s. If warfarin, statins, or blood pressure meds are on the list, pay attention.
- Talk to your doctor or pharmacist. Don’t wait for them to ask. Bring it up. Say: “I drink pomegranate juice daily. Should I be worried?”
- Keep it consistent. If you drink it, drink the same amount every day. Don’t go from zero to three glasses a week. Don’t quit cold turkey.
- Monitor for signs. For warfarin users: unusual bruising, nosebleeds, dark stools, headaches. For statins: muscle pain or weakness. For blood pressure meds: dizziness or fainting. Report these immediately.
- Wait two hours. Take your pill first. Drink the juice later. It won’t eliminate risk, but it reduces it.
The Bottom Line
Pomegranate juice isn’t poison. For most people on most meds, it’s fine. But for those on narrow-window drugs-especially warfarin-it’s a silent player that can tip the scales. The science isn’t settled, but the real-world cases are too frequent to ignore. Don’t let the word “natural” fool you. What’s natural doesn’t always mean safe, especially when it’s interacting with chemicals designed to change how your body works. The best protection? Knowledge. Communication. And consistency.Can pomegranate juice really affect my blood thinner?
Yes, it can. Pomegranate juice may inhibit enzymes that break down warfarin, leading to higher levels in the blood and increased risk of bleeding. While not everyone experiences this, case reports show INR levels rising significantly after starting regular consumption. If you’re on warfarin, talk to your doctor before drinking it regularly, and monitor your INR closely if you do.
Is pomegranate juice as dangerous as grapefruit juice?
No, it’s not nearly as potent. Grapefruit juice can increase drug levels by up to 15 times for some medications, which is why the FDA issues clear warnings. Pomegranate juice’s effect is much weaker-typically around 20-40% inhibition in lab studies, but often negligible in humans. Still, because it’s less well-known, people may not realize the risk, making it potentially more dangerous in practice.
Should I stop drinking pomegranate juice if I’m on medication?
Not necessarily. If you’ve been drinking it regularly and your medication levels are stable, there’s no need to quit. The bigger risk is sudden changes. If you’re thinking of starting it, talk to your doctor first. If you’re already drinking it, keep the amount consistent. Abruptly stopping or starting can be more harmful than steady, moderate use.
How long does it take for pomegranate juice to affect my meds?
It can happen quickly. In documented cases, INR changes appeared within 2-3 days of starting daily pomegranate juice. The effect builds over time as the compounds accumulate in your system. That’s why consistency matters-sudden changes are riskier than long-term, steady intake.
Are there any medications that are safe to take with pomegranate juice?
Yes, many are. Most common medications-like antibiotics, thyroid meds, or birth control pills-aren’t significantly affected by pomegranate juice. The risk is mostly with drugs metabolized by CYP3A4 or CYP2C9 and those with narrow therapeutic windows. If you’re unsure, check your specific medication with your pharmacist. For most people, moderate intake is safe.





Roshan Gudhe
This is such a nuanced topic. I've been drinking pomegranate juice for years with my statins, and my liver enzymes have never blinked. But I also know people who swear they had muscle pain vanish the day they quit. Science says 'maybe,' but lived experience says 'it depends.' Maybe the real takeaway isn't to fear it, but to observe your own body. Your genes, your gut, your habits-they all matter more than blanket warnings.
caroline hernandez
From a pharmacokinetic standpoint, CYP3A4 inhibition by punicalagin metabolites is well-documented in vitro, but the clinical relevance is confounded by first-pass metabolism variability, plasma protein binding, and interindividual CYP expression. The FDA's lack of labeling reflects this evidence gap. For high-risk patients-especially those on narrow-therapeutic-index agents-TDM (therapeutic drug monitoring) should be prioritized over dietary dogma.
Janice Williams
I find it deeply concerning that people treat natural substances as inherently safe. This is why we have so many avoidable ER visits. Pomegranate juice isn't 'healthy'-it's a bioactive compound with documented enzyme-inhibiting properties. If you're on warfarin and you're drinking it daily, you're gambling with your life. No amount of anecdotal 'I'm fine' changes the fact that some people aren't.
Wendy Lamb
I've been on blood pressure meds for 8 years. I drink a small glass of pomegranate juice every morning. My doctor never said a word. I checked my levels last month-perfect. Maybe it's not a problem for everyone. Don't scare people into quitting something they enjoy unless the evidence is crystal clear.
Alex LaVey
I love how we turn everything into a threat. I drink juice. I take my meds. I live. People in other countries drink this stuff daily and don't end up in the hospital. Maybe the real issue is over-medicalizing everyday life. Not everything that *can* interact *does*. Chill out. Enjoy your juice.
Kunal Kaushik
I’ve been drinking it with my antidepressants for 3 years. No issues. My therapist even said it’s good for mood. I think the fear is overblown. If it was that dangerous, we’d hear about it everywhere. But we don’t. So maybe… it’s fine?
Rachel Kipps
I'm not a doctor, but I work in a pharmacy. We see 2-3 patients a month who come in panicked because they read something online. Most of them are fine. The ones who aren't? They changed their intake suddenly. Consistency is key. Don't start drinking 3 glasses a day after never having it. Don't quit cold turkey. Just keep it steady. That's all.
Prajwal Manjunath Shanthappa
The fact that this isn't labeled like grapefruit juice is a scandal. Big juice corporations don't want you to know. The FDA is asleep at the wheel. This is corporate negligence disguised as 'natural wellness.' You think your 'healthy habit' is safe? It's a Trojan horse. Wake up. Read the studies. The data is there. They just don't want you to see it.
Jhoantan Moreira
I appreciate how balanced this post is. I'm on warfarin, and I had my INR checked last week-perfect. I drink a small glass every day. I don't see why we can't trust people to make informed choices instead of scaring them into avoidance. Knowledge > fear.
Ed Mackey
i read this and was like… wait i drink this every day with my amlodipine. should i be worried? i dont have any symptoms. my bp is stable. maybe i should talk to my dr. but i dont wanna sound dumb. anyone else?
Caleb Sutton
They don't want you to know the truth. Pomegranate juice is a cover. The real danger? The government and pharmaceutical companies are using this to push you toward synthetic alternatives. They profit from your fear. They profit from your meds. They profit from your confusion. Don't fall for it. Stop drinking juice. Stop trusting doctors. Take control.
Daz Leonheart
I just wanted to say thank you for writing this. I’ve been on cyclosporine since my transplant, and I had no idea. I started drinking pomegranate juice last year. I didn’t think it mattered. I just found out my levels spiked last month. I stopped it immediately. I’m so glad I read this before something worse happened.