Black Cohosh Liver Risk Assessment Tool
Assess Your Personal Risk
This tool helps you understand your risk of liver injury when using black cohosh based on your medications and health conditions.
Every year, over a million women in the U.S. turn to black cohosh to ease hot flashes, night sweats, and other menopausal symptoms. It’s marketed as a natural alternative to hormone therapy-no estrogen, no prescription, just a pill. But behind the soothing claims lies a quiet, serious risk: liver damage. And it doesn’t just happen to people taking too much. Even those using the standard dose, exactly as directed, have ended up in the hospital with acute hepatitis or liver failure.
What Is Black Cohosh, Really?
Black cohosh (Cimicifuga racemosa) is a plant native to North America. Its roots and rhizomes have been used for over 150 years, first by Native Americans, then by 19th-century Eclectic physicians. Today, it’s sold in capsules, tinctures, and teas, often under brand names like Remifemin. Most products contain 20-40 mg of standardized extract taken twice daily, with at least 1% triterpene glycosides-actein and cimicifugoside-as the active markers. It’s not a hormone. Unlike estrogen, black cohosh doesn’t bind to estrogen receptors in most studies. That’s why it became popular among breast cancer survivors who were told to avoid hormone therapy. But here’s the catch: just because it’s not estrogenic doesn’t mean it’s safe. The same compounds that might help with hot flashes are also the ones that can trigger liver injury in some people.The Liver Risk Isn’t Theoretical-It’s Documented
Since 2003, over 50 confirmed cases of liver injury linked to black cohosh have been reported in medical journals and databases like LiverTox (NCBI). These aren’t vague anecdotes. They’re detailed clinical cases:- A 51-year-old woman developed ALT levels of 722 U/L (normal: 7-56) after three months of use. She recovered fully after stopping the supplement.
- A 54-year-old woman took black cohosh and acetaminophen-both within recommended doses-and ended up in liver failure. She needed a transplant.
- Another case involved a 59-year-old woman with no prior liver disease who developed acute hepatitis after 90 days of black cohosh. Her bilirubin hit 15.8 mg/dL-a sign of severe liver stress.
How Does It Hurt the Liver?
Scientists don’t fully understand why black cohosh damages the liver in some people but not others. There are three leading theories:- Direct toxicity: The triterpene glycosides might be inherently toxic to liver cells in certain individuals.
- Idiosyncratic reaction: Your body’s unique metabolism turns a harmless compound into a liver toxin. Think of it like a genetic lottery-some win, some lose.
- Immune-mediated injury: Your immune system mistakes liver cells for invaders and attacks them after black cohosh exposure.
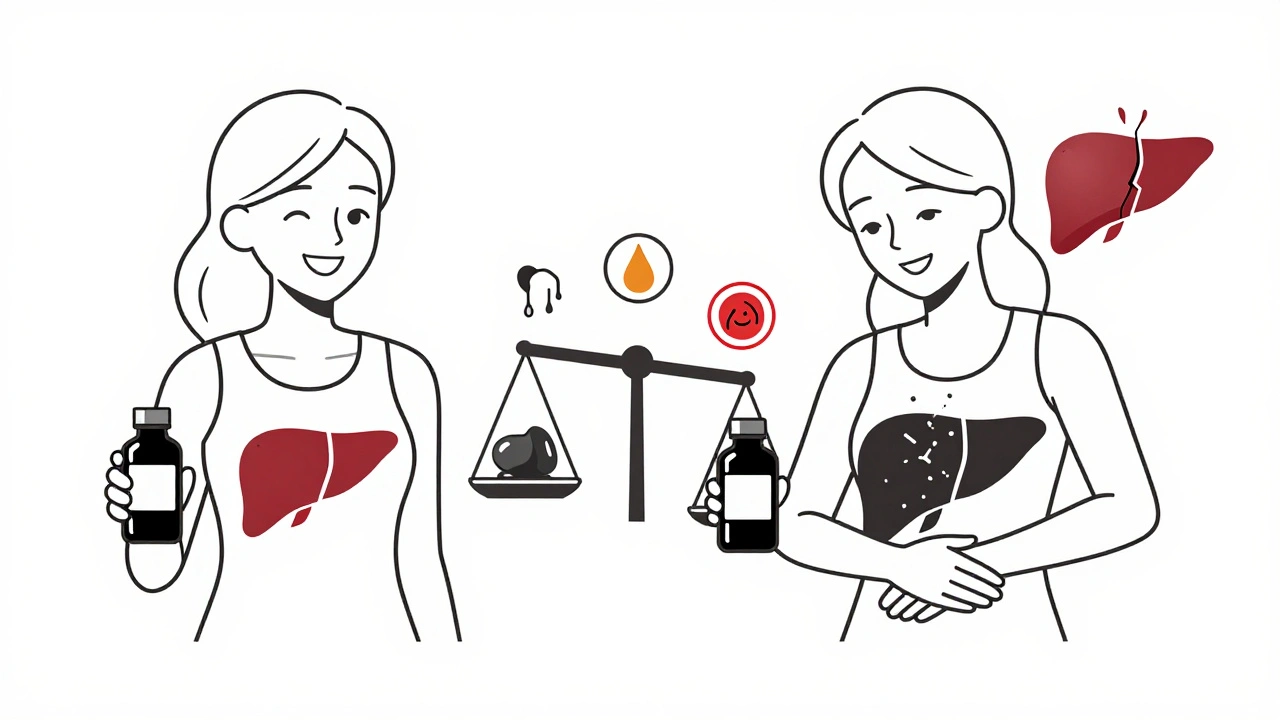
Medication Interactions: The Hidden Danger
Black cohosh doesn’t just sit quietly in your body. It’s processed by the liver using enzymes called CYP2D6 and CYP3A4. These are the same enzymes that break down dozens of common medications. When black cohosh overlaps with them, things get risky. Here’s what you should avoid combining with black cohosh:- Acetaminophen (Tylenol): Even at normal doses, this combo has caused liver failure. The risk triples when both are taken together.
- Statins (like atorvastatin or simvastatin): These already carry a small risk of liver enzyme elevation. Add black cohosh, and the chance of damage jumps significantly.
- Methotrexate: Used for autoimmune conditions and some cancers. Combined with black cohosh, it can cause severe, irreversible liver scarring.
- Certain antibiotics (clarithromycin, erythromycin): These inhibit CYP3A4, causing black cohosh to build up in your system and overwhelm your liver.
- Birth control pills and hormone therapies: Even though black cohosh isn’t estrogenic, mixing it with other hormones adds unpredictable stress to the liver.
Who’s Most at Risk?
Not everyone needs to avoid black cohosh-but some people absolutely should:- People with existing liver disease: Fatty liver, hepatitis, cirrhosis-any condition that already stresses the liver makes black cohosh dangerous.
- Those on multiple medications: Especially if any are processed by the liver.
- Women over 50: Liver metabolism slows with age. Older bodies clear toxins slower, increasing risk.
- People taking supplements long-term: Most liver injuries occur after 2-6 months. The longer you take it, the higher the chance.
- Those with a history of allergic reactions to herbs: Your immune system may be primed to overreact.
What Do Experts Say?
There’s deep division in the medical community. On one side: Dr. Jayant Talwalkar, author of the LiverTox monograph, says black cohosh has caused cases ranging from mild enzyme spikes to fatal liver failure requiring transplant. The European Medicines Agency has required liver injury warnings on all black cohosh products since 2012. On the other: Dr. Johanna Budwig, who led a large clinical trial in 2008, argues that most reports are misleading. She says in trials with over 1,200 women, no liver injury was linked to black cohosh. But her study didn’t test people on other medications or with pre-existing liver conditions. Real-world use is messier. The American Association for the Study of Liver Diseases (AASLD) classifies black cohosh as a “probable” cause of drug-induced liver injury. The American College of Obstetricians and Gynecologists (ACOG) updated its guidelines in January 2024 to explicitly advise against its use in women with liver disease or those on hepatotoxic drugs.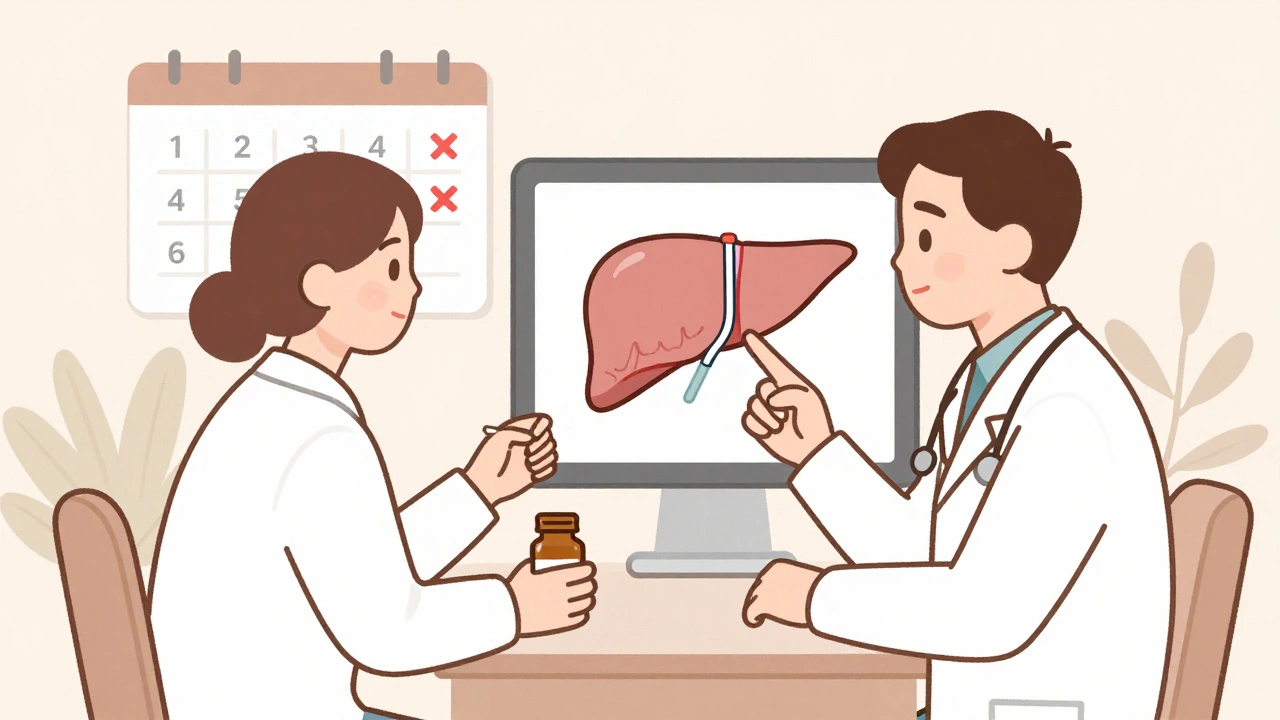
What About ‘Liver-Safe’ Formulas?
In 2023, companies like Gaia Herbs and Nature’s Way launched new black cohosh products claiming to remove the toxic compounds. They say their extraction methods make the supplement safer. Here’s the problem: there’s no clinical proof. The American Gastroenterological Association issued a statement in June 2023 saying, “No evidence demonstrates improved safety profiles for these modified formulations.” The NIH is funding a five-year study (NCT05112345) to find out what’s really going on. Results won’t be out until 2025. Until then, assume all black cohosh carries the same risk.What Should You Do?
If you’re currently taking black cohosh:- Stop immediately if you notice dark urine, yellow eyes, unexplained fatigue, or right-side abdominal pain.
- Get a liver panel (ALT, AST, bilirubin, Alk Phos) even if you feel fine. Many injuries show up on blood tests before symptoms appear.
- Talk to your doctor about every supplement you take-not just prescriptions. Most doctors don’t ask.
- Don’t restart even if your liver enzymes return to normal. The risk of recurrence is high.
- Ask your doctor if you have any liver condition, take any medications, or are over 50.
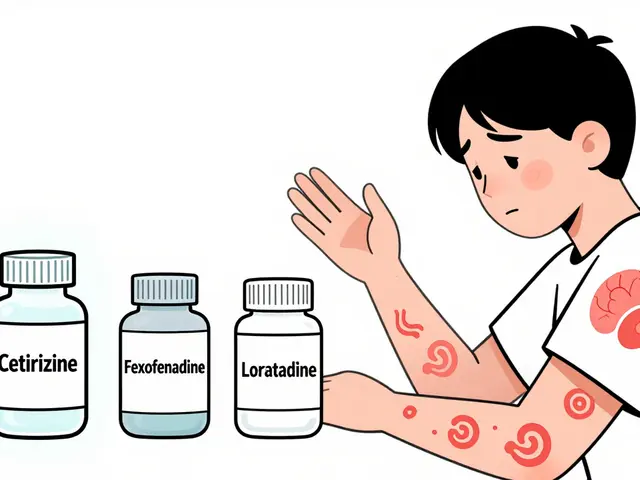
- Consider alternatives. SSRIs like paroxetine or escitalopram are proven to reduce hot flashes with far less liver risk.
- Look into non-pharmacological options: paced breathing, acupuncture, cognitive behavioral therapy-all shown in studies to cut hot flashes by 50% or more.
Bottom Line
Black cohosh isn’t a harmless herb. It’s a supplement with a documented, serious risk of liver damage-especially when mixed with common medications. The fact that it’s sold over the counter doesn’t mean it’s safe. The fact that some people feel better doesn’t mean it’s safe for you. The liver doesn’t scream until it’s too late. By the time you feel sick, the damage may already be done. If you’re using black cohosh, get tested. If you’re thinking about it, pause. There are safer ways to manage menopause symptoms. You don’t need to gamble your liver to feel better.Can black cohosh cause liver damage even if I take it as directed?
Yes. Liver injury from black cohosh isn’t always tied to overdose. Many cases occur in people taking the standard dose of 20-40 mg twice daily. The risk appears to be idiosyncratic-meaning your body’s unique chemistry may react unpredictably. Over 50 documented cases in medical literature involved patients taking recommended doses.
Is black cohosh safe for breast cancer survivors?
While black cohosh doesn’t act like estrogen and was once thought safe for breast cancer survivors, it’s no longer recommended. The risk of liver damage is real, and many survivors take other medications like tamoxifen or aromatase inhibitors, which are also processed by the liver. Combining them increases risk. Organizations like Susan G. Komen now advise against its use in this group.
What symptoms should I watch for if I’m taking black cohosh?
Watch for dark urine, yellowing of the skin or eyes (jaundice), extreme fatigue, nausea, vomiting, abdominal pain (especially on the right side), and unexplained itching. These are early signs of liver injury. If you notice any of these, stop the supplement immediately and get a liver function test.
Can I take black cohosh with vitamins or other herbal supplements?
It’s not safe to assume so. Many herbal supplements-like green tea extract, kava, and high-dose vitamin A-are also linked to liver injury. Combining them with black cohosh increases the burden on your liver. Even common vitamins like niacin (B3) in high doses can stress the liver. If you’re taking multiple supplements, assume risk is cumulative.
Are there safer alternatives to black cohosh for hot flashes?
Yes. Low-dose SSRIs like paroxetine or escitalopram are FDA-approved for hot flashes and have strong evidence behind them. Non-drug options like paced breathing, cognitive behavioral therapy, and acupuncture have been shown to reduce hot flashes by 50% or more. Lifestyle changes-avoiding alcohol, spicy foods, and hot environments-also help. These alternatives carry far less risk than black cohosh.
How often should I get my liver tested if I take black cohosh?
If you choose to use black cohosh despite the risks, get a baseline liver function test before starting. Then repeat it at 8 weeks and again at 16 weeks. Many cases of injury show up between 2 and 6 months. If any liver enzyme rises above 3 times the normal level, stop immediately. Most doctors don’t monitor this-so you have to ask.
Why is black cohosh still sold if it’s dangerous?
In the U.S., dietary supplements like black cohosh are regulated under DSHEA (1994), which means manufacturers don’t need to prove safety before selling. The FDA can only act after harm is proven and reported. That’s why products with known risks stay on shelves. In contrast, the European Union requires warning labels and batch testing. The market is driven by demand, not safety oversight.
Do all black cohosh products carry the same risk?
There’s no way to know for sure. Products vary in purity, concentration, and even ingredients. Some have been found to contain other plants or contaminants. Even reputable brands have had issues. The liver injury risk appears linked to the plant’s active compounds, not just contamination. So while better manufacturing helps, it doesn’t eliminate the biological risk in susceptible individuals.
If you’re considering black cohosh, remember: natural doesn’t mean safe. And when it comes to your liver, there’s no second chance. Ask questions. Get tested. Choose safer options. Your body will thank you.




James Kerr
Man, I took this stuff for a year and never felt a thing. But now I’m paranoid every time I take Tylenol. 😅
Rashi Taliyan
My aunt took black cohosh after her hysterectomy-ended up in the ER with jaundice. No one asked her what supplements she was on. Doctors assume ‘natural’ = safe. It’s terrifying. 🙏
Rashmin Patel
As someone who’s been managing menopause with acupuncture and daily breathwork for 3 years, I can’t believe people still gamble with their liver over a herb that’s basically a placebo with side effects. I used to take it too-until my ALT spiked. Now I just do yoga at 5 a.m., drink peppermint tea, and call it a win. No labs, no panic, no regrets. 🌿✨
bobby chandra
Let’s be real-this isn’t about black cohosh. It’s about a broken system where ‘natural’ is a marketing buzzword and the FDA sits on its hands until someone dies. We regulate aspirin like it’s plutonium but let a plant extract with 50+ documented liver failures be sold next to gummy vitamins. The hypocrisy is nauseating. 🤬
Archie singh
Of course it’s dangerous. Anyone with a pulse and a brain knows supplements are unregulated snake oil. You’re not a scientist just because you read a blog. Stop pretending your herbal tea is medicine. #WokeNutrition #LiverDeathTrap
Kara Bysterbusch
As an Indian-American woman who’s navigated both Western medicine and Ayurvedic traditions, I find this deeply unsettling. In India, we’ve long understood that ‘natural’ doesn’t mean ‘innocent’-turmeric can thin blood, neem can harm kidneys, and yes, black cohosh can fry your liver. The problem isn’t the herb-it’s the cultural disconnect. We treat supplements like candy because we’ve lost the wisdom of context, dosage, and individual constitution. Let’s honor both science and tradition-but with humility, not hype.
Joykrishna Banerjee
While the data presented is statistically compelling, one must interrogate the epistemological framework underpinning the attribution of hepatotoxicity. The case series cited exhibit significant selection bias, conflating temporal association with causal inference. Furthermore, the absence of controlled pharmacokinetic profiling in these reports renders the mechanistic claims-particularly those regarding CYP450 modulation-speculative at best. One cannot, in good scientific conscience, generalize population-level risk from N=50 anecdotal reports lacking standardized exposure metrics or genetic stratification. The AASLD classification of ‘probable’ is precisely that: probabilistic, not deterministic. To conflate this with clinical certainty is to engage in medical alarmism.
Myson Jones
I appreciate how thorough this post is-and I want to thank you for highlighting the real risks. I’m a nurse, and I’ve seen too many patients come in with liver damage from ‘just a little herb.’ The sad part? They never thought to mention it. If you’re on meds, over 50, or have any liver history, please talk to your provider. We’re not here to judge-we’re here to help you stay safe. You’re not alone in this.
Albert Essel
There’s a critical gap in public health communication here. The narrative around herbal supplements is polarized: either they’re ‘miracle cures’ or ‘deadly poisons.’ The truth lies in the middle. Black cohosh has potential benefits for some, but its risk profile is real, unpredictable, and poorly understood. We need better labeling, mandatory liver enzyme warnings on packaging, and mandatory provider education-not bans. Knowledge, not fear, should drive decisions.
Cindy Lopez
So… you’re saying I should stop taking my ‘natural’ menopause pills? But they’re from Whole Foods. And the bottle says ‘non-GMO.’ That’s gotta mean something, right?
Chloe Madison
My mom took this for 6 months and didn’t know her liver was failing until she collapsed. She’s fine now, but she’s on meds for life. I’m not letting anyone in my family touch this stuff. If you’re thinking about it-just don’t. There are better, safer ways. You don’t need to suffer to feel better. And you definitely don’t need to risk your liver.
vinoth kumar
Big respect for putting this out there. I’m from Delhi and we use herbs all the time-but we also know when to stop. My cousin’s friend took ashwagandha and got hepatitis. Same thing. Natural doesn’t mean gentle. I shared this with my mom’s book club-everyone’s stopping now. Thanks for the wake-up call.
Vincent Soldja
Post is well-researched. However, the conclusion lacks nuance. While the data is concerning, blanket avoidance may deprive some of symptom relief. A risk-stratified approach-screening, monitoring, education-is preferable to fear-based abstinence. Also, the FDA’s inaction is systemic, not individual. Blaming consumers ignores regulatory failure.