What Exactly Is Pneumonia?
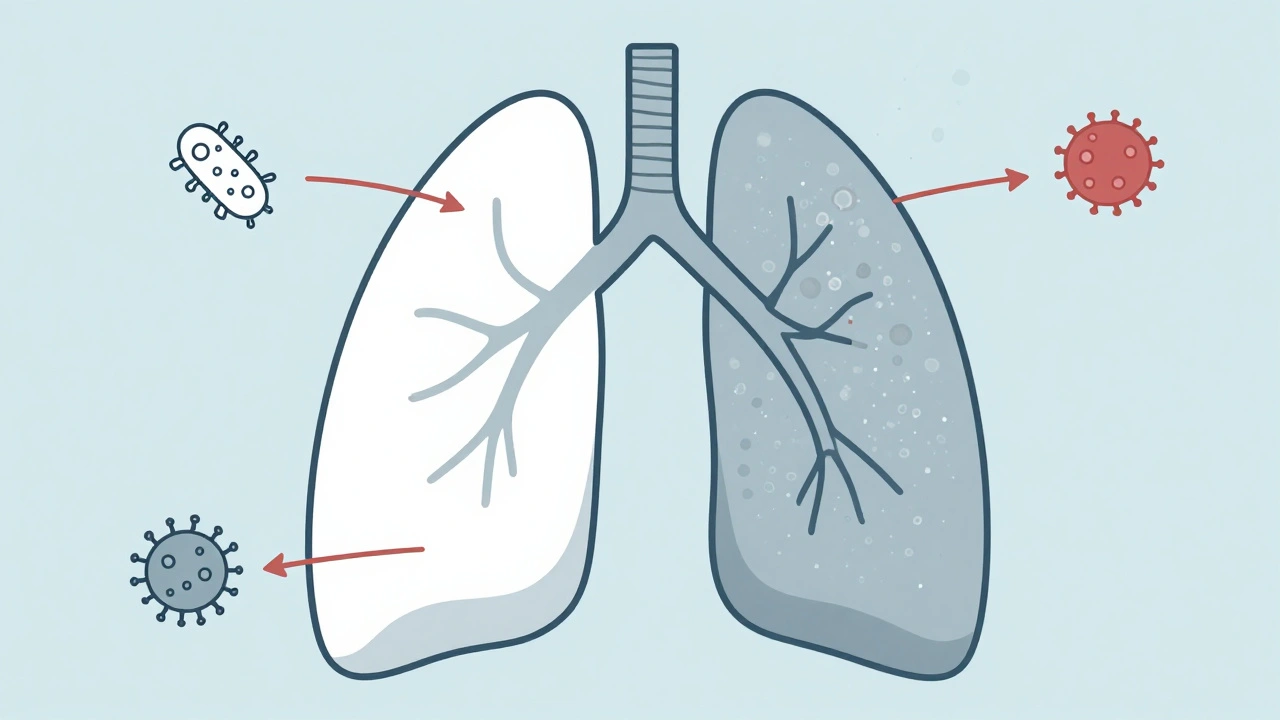
Pneumonia isn’t just a bad cold that won’t go away. It’s an infection that fills the tiny air sacs in your lungs-called alveoli-with fluid or pus. This makes it hard to breathe, lowers your oxygen levels, and can leave you feeling wrecked for days or even weeks. The good news? Not all pneumonia is the same. The type you get depends on what’s causing it: bacteria, viruses, or fungi. And knowing which one you’re dealing with changes everything-from how you’re treated to how likely you are to recover.
Bacterial Pneumonia: The Sudden Onset
Bacterial pneumonia hits fast. One day you might feel fine, the next you’re running a high fever-102°F or higher-and coughing up thick, yellow or green mucus. Chest pain is sharp, especially when you breathe in or cough. Your lips or fingernails might turn blue because your body isn’t getting enough oxygen. This is the kind of pneumonia that lands people in the hospital.
The biggest culprit? Streptococcus pneumoniae. It’s responsible for about half of all community-acquired cases worldwide. Other common bacteria include Haemophilus influenzae, Staphylococcus aureus, and Mycoplasma pneumoniae-the one that causes "walking pneumonia," a milder version that lets people keep going, even if they feel awful.
On a chest X-ray, bacterial pneumonia shows up as a solid white patch in one lobe of the lung. That’s because the infection is localized, not spread out. Your immune system responds with a flood of neutrophils-white blood cells that swarm the bacteria like reinforcements in a battle. Antibiotics are the go-to treatment. Penicillin, macrolides like azithromycin, or fluoroquinolones like levofloxacin can knock it out in days if caught early.
But here’s the problem: too many people get antibiotics when they don’t need them. If you have a virus and get a prescription for amoxicillin, it won’t help-and it makes superbugs stronger. The CDC says nearly 30% of outpatient antibiotic prescriptions are unnecessary. That’s why getting the right diagnosis matters.
Viral Pneumonia: The Slow Burn
Viral pneumonia creeps in. You start with a runny nose, sore throat, maybe a low-grade fever. By day three or four, you’re coughing more, feeling achy, exhausted. Unlike bacterial pneumonia, your fever rarely spikes above 102°F. You don’t usually cough up thick mucus-your cough is dry, hacking, and persistent.
The usual suspects? Influenza A and B, RSV (especially in kids and older adults), and SARS-CoV-2 (the virus behind COVID-19). Rhinovirus and parainfluenza can also cause it. During flu season, about one in three pneumonia cases is viral.
On an X-ray, viral pneumonia looks totally different. Instead of one white patch, you’ll see a hazy, scattered pattern across both lungs. That’s because the virus attacks the walls between air sacs, not the sacs themselves. Your body’s immune response is more about inflammation than pus. There’s no quick fix with antibiotics. Treatment is mostly rest, fluids, and oxygen if needed.
Antivirals like oseltamivir (Tamiflu) can help if you catch the flu early. For severe COVID-19 pneumonia, remdesivir might be used. But most of the time, your immune system has to fight it off on its own. That’s why vaccines are so important. The flu shot cuts your risk of pneumonia by 40-60% in a good match year. The COVID-19 vaccine reduces pneumonia risk by up to 90% in the first few months after getting it.
Here’s a scary twist: viral pneumonia often opens the door to bacterial pneumonia. About 25-30% of people with severe flu develop a secondary bacterial infection-usually from Streptococcus pneumoniae or Staphylococcus aureus. That’s why doctors watch closely after a viral illness. If your symptoms suddenly get worse after a few days, it could mean a bacterial invader has moved in.
Fungal Pneumonia: The Hidden Threat
Fungal pneumonia doesn’t usually affect healthy people. If you’re young, active, and not on any immune-suppressing meds, you’re probably fine. But if you have HIV, are getting chemotherapy, took an organ transplant, or are on long-term steroids-you’re at risk.
The fungi that cause it live in the soil, bird droppings, and bat guano. In the U.S., three are most common:
- Coccidioides-found in the Southwest (Arizona, California). Causes Valley fever. Around 20,000 cases a year.
- Histoplasma-common in the Ohio and Mississippi River valleys. About 65% of people in those areas have been exposed at some point.
- Blastomyces-lives in moist soil near rivers. Causes blastomycosis. About 1-2 cases per 100,000 people annually.
People who work outside-farmers, landscapers, construction workers-are 2-3 times more likely to inhale these spores. You might not feel sick right away. Symptoms can mimic a cold: fever, cough, chills, even nausea. But it can take weeks or months to get worse.
Standard tests won’t catch it. You need special lab work: fungal cultures, antigen tests, or PCR panels. Chest X-rays look like bacterial or viral pneumonia, so it’s easy to miss. The big red flag? No improvement after antibiotics. If you’re not getting better-and you’ve been around soil or dust-fungal pneumonia should be on the radar.
Treatment? Not antibiotics. You need antifungals. For serious cases, amphotericin B is used. For milder ones, azoles like itraconazole or fluconazole work over weeks or months. Recovery takes time. And relapses are common if treatment stops too soon.
How Doctors Tell Them Apart
There’s no single test you can do at home. But doctors use a mix of clues:
| Feature | Bacterial | Viral | Fungal |
|---|---|---|---|
| Onset | Sudden, hours to a day | Gradual, days | Very slow, weeks |
| Fever | High (102-105°F) | Mild to moderate (100-102°F) | Moderate, often persistent |
| Cough | Productive, thick sputum | Dry, hacking | Productive, sometimes with blood |
| Chest X-ray | Lobar consolidation (one white patch) | Diffuse, bilateral haze | Similar to bacterial or viral-hard to tell |
| Response to Antibiotics | Improves in 48-72 hours | No improvement | No improvement |
| High-Risk Groups | All ages, especially elderly | Children, elderly, pregnant | Immunocompromised, outdoor workers |
Now, new tools are helping. Multiplex PCR tests can check one sputum sample for 20+ viruses and bacteria at once-with 95% accuracy. That’s a game-changer. Instead of guessing, doctors can know within hours whether it’s flu, RSV, or Streptococcus pneumoniae.
Who’s Most at Risk?
Anyone can get pneumonia. But some people are far more vulnerable:
- Children under 2-their immune systems are still developing.
- Adults over 65-lungs weaken with age.
- Smokers-they’re 2.3 times more likely to get it.
- People with chronic diseases-COPD, heart failure, diabetes, or asthma.
- Immunocompromised-HIV, cancer treatment, transplant drugs.
And yes, location matters. If you live in Arizona or Texas, you’re more likely to breathe in Coccidioides spores. If you work in a barn or dig soil in the Midwest, Histoplasma is a real risk. Knowing your environment helps your doctor think faster.
Prevention: What Actually Works
There’s no magic shield, but you can stack the odds in your favor:
- Pneumococcal vaccines-Prevnar 20 protects against 20 strains of Streptococcus pneumoniae. It’s recommended for kids under 2 and adults 65+. Efficacy? Up to 80% in adults.
- Annual flu shot-cuts pneumonia risk by half during flu season.
- COVID-19 boosters-still the best defense against severe lung infection.
- Quit smoking-your lungs start healing within weeks.
- Wear a mask in dusty environments-especially if you’re immunocompromised.
- Wash your hands-simple, but still one of the top ways to stop viruses.
Here’s the hard truth: even with vaccines, only 68% of adults over 65 in the U.S. are protected against pneumococcal pneumonia. That’s a gap. And it’s deadly. Every year, pneumonia causes 50,000 deaths in the U.S. alone. Most of those are preventable.

When to Worry-And When to Wait
Not every cough needs an ER visit. But if you have:
- High fever that won’t break
- Chest pain that gets worse when you breathe
- Difficulty breathing or shortness of breath at rest
- Lips or fingers turning blue
- Confusion or dizziness (especially in older adults)
-get checked. Don’t wait. Pneumonia can turn deadly fast, especially in high-risk groups.
And if you’ve been on antibiotics for three days and feel worse? That’s a red flag. It might mean you have a virus or fungus-and the antibiotics aren’t helping. Time to go back to your doctor.
What’s Next in Pneumonia Care?
Researchers are working on ways to tell bacterial from viral infections using just a blood test. If it works, we could cut down on unnecessary antibiotics by 40%. That’s huge for stopping drug-resistant superbugs.
Next-gen vaccines are coming too. More serotypes, better coverage, longer protection. And for fungal pneumonia? Better diagnostics are in the works-faster, cheaper tests that can be done in a doctor’s office.
For now, the best tool you have is awareness. Know your risks. Get vaccinated. Don’t ignore symptoms. And if you’re not getting better-ask: could this be something other than a cold?
Can you get pneumonia from the flu shot?
No. The flu shot contains dead or inactivated virus particles-it can’t cause pneumonia or the flu. Some people feel achy or run a low fever after the shot, but that’s your immune system responding, not an infection. If you get sick right after the shot, you were probably exposed to a virus before getting vaccinated.
Is fungal pneumonia contagious?
No. Fungal pneumonia isn’t spread from person to person. You catch it by breathing in spores from the environment-soil, bird droppings, decaying wood. You can’t catch it from someone else’s cough or sneeze. That’s why it’s not a public health threat like the flu or COVID-19.
Can children get fungal pneumonia?
It’s extremely rare in healthy children. Fungal pneumonia mostly affects people with weakened immune systems. Children with cancer, HIV, or those on long-term steroids are at risk, but otherwise, their immune systems handle the spores just fine.
Do antibiotics work on viral pneumonia?
No. Antibiotics kill bacteria, not viruses. Taking them for viral pneumonia won’t help you feel better-it just increases your risk of side effects like diarrhea or yeast infections. Worse, it contributes to antibiotic resistance, making future bacterial infections harder to treat.
How long does pneumonia last?
It depends. Bacterial pneumonia often improves in 3-5 days with antibiotics, but fatigue can linger for weeks. Viral pneumonia usually takes 1-3 weeks to clear. Fungal pneumonia? That can take months. Recovery isn’t just about the fever going down-it’s about your lungs healing completely. Don’t rush back to work or exercise too soon.
Final Thought: Don’t Guess-Get Tested
Pneumonia isn’t one illness. It’s three very different infections with the same symptoms. Mistaking one for another can delay treatment, waste time, or even put you in danger. If you’re sick with a lung infection, don’t assume it’s just a cold or the flu. Ask your doctor: "Could this be bacterial, viral, or something else?" And if you’re high-risk-ask about testing. Your lungs are worth it.





Kurt Russell
Bro this is the most useful thing I’ve read all year. I had no idea fungal pneumonia was a thing until I saw the part about Arizona soil. My uncle got it after landscaping - thought it was just a bad cold for months.
Got tested after his doctor finally said, 'Wait, have you been around bird poop?' Yeah. Turns out, yes.
Antifungals saved his life. Don’t ignore persistent coughs. Seriously.
Wesley Phillips
Antibiotics for viral pneumonia is like using a chainsaw to cut butter. You're not helping anyone except Big Pharma.
Also 'walking pneumonia' is a marketing term invented by doctors to make people feel better about being sick. It's not walking. You're crawling.
Kyle Oksten
The real issue here isn't diagnosis - it's systemic neglect. We have the tools to detect these infections accurately, but we don't prioritize them.
Why? Because profit-driven medicine rewards volume over precision. Antibiotics are cheap. PCR panels are expensive.
We're not failing because we lack knowledge. We're failing because we lack will.
Sam Mathew Cheriyan
wait but whats the real truth? i heard the gov is spraying spores in the air to make people sick so they buy vaccines lol. also why do they say fungal pneumonia isnt contagious if its in the air? sounds sus. my cousin got it after a concert in texas. maybe the air conditioning was rigged?
Ernie Blevins
So let me get this straight. You’re telling me if I get a cough and I’m not on chemo, I’m fine? What about my dog? He coughs sometimes. Is he gonna die? I’m just asking.
Ryan Sullivan
The conflation of community-acquired pneumonia with nosocomial variants remains a persistent epistemological flaw in public health discourse.
Furthermore, the efficacy metrics cited for pneumococcal vaccines are derived from phase III trials with selection bias toward low-risk cohorts.
One must interrogate the underlying epidemiological assumptions before endorsing blanket vaccination mandates.
Desmond Khoo
This literally saved me. I thought I had the flu, but my cough wouldn’t quit. Went to the doc, got tested, turned out it was fungal. 🙌
Got on antifungals and now I’m back to hiking. 🏔️❤️
PS: If you’re out in the dirt, wear a mask. Your lungs will thank you. 🫡
Louis Llaine
Wow. A whole article about pneumonia and not one mention of 5G. I’m shocked.