FDA Drug Safety: What You Need to Know About Risk, Monitoring, and Real-World Side Effects
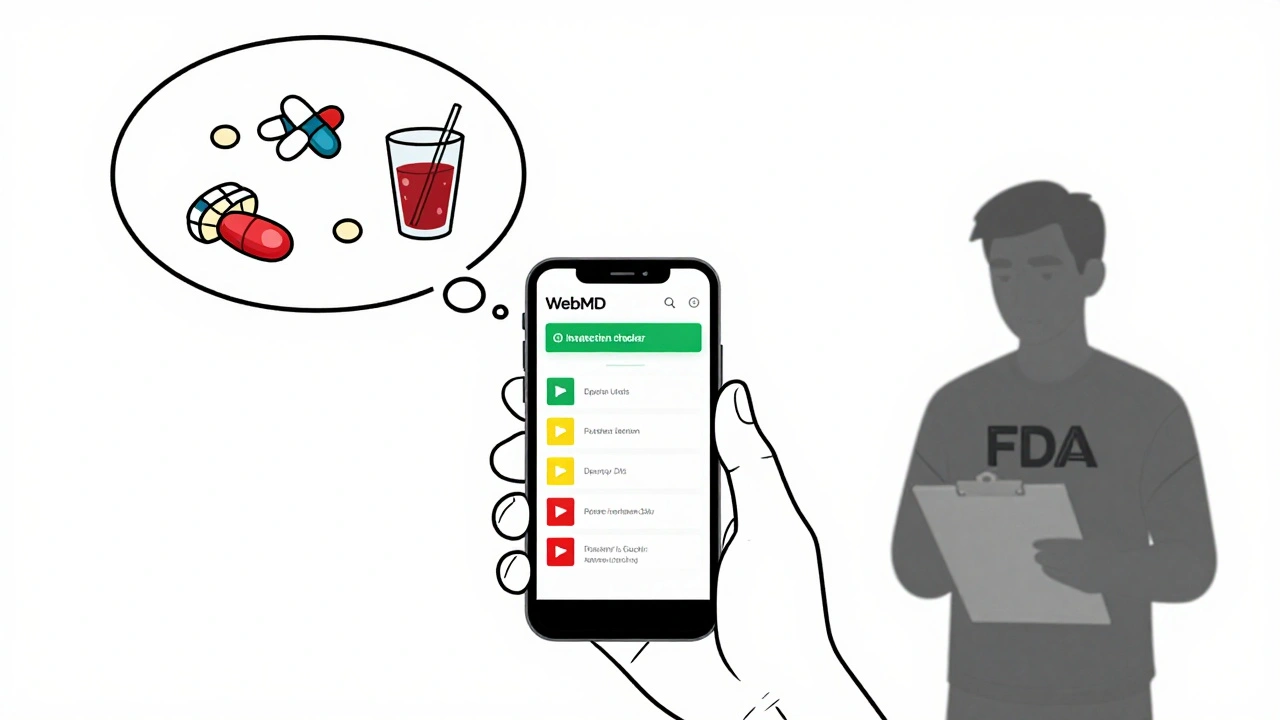
When the FDA drug safety, the system that evaluates and monitors the risks of prescription and over-the-counter medications in the U.S.. Also known as post-market drug surveillance, it’s not just about approving pills—it’s about spotting what goes wrong after millions start taking them. Most people think if a drug gets FDA approval, it’s completely safe. That’s not true. Approval means the benefits outweigh the risks in clinical trials. But real life? It’s messier. People take multiple drugs. They have other health issues. They forget doses. That’s where drug interactions, when two or more medications affect each other’s behavior in the body, often leading to unexpected side effects. come in. A drug that’s fine alone can turn dangerous when mixed with statins, antidepressants, or even common painkillers like acetaminophen. Black cohosh, for example, isn’t banned—but it can wreck your liver when paired with other meds. That’s not a fluke. It’s exactly the kind of risk the FDA tracks after approval.
Then there’s medication monitoring, the ongoing process of checking drug levels, organ function, and symptoms to catch problems before they become emergencies.. Cyclosporine, used after transplants, can silently destroy kidneys. Tolvaptan for hyponatremia can cause liver damage if not watched. Insulin pumps need precise settings—wrong basal rates can kill. These aren’t edge cases. They’re routine. The FDA doesn’t just rely on doctors to report problems. They dig into real-world data: ER visits, pharmacy records, patient forums. That’s how they found gabapentinoids and opioids together cause deadly breathing problems. That’s how they flagged that restarting opioids after a break can lead to overdose—because your body forgot how to handle the dose. And that’s why therapeutic equivalence, the idea that a generic drug works just like the brand name, down to how your body absorbs it. matters. Not all generics are equal. Some have different fillers. Some are made in different factories. A small difference in absorption can mean the difference between control and crisis, especially with narrow-therapeutic-index drugs like warfarin or cyclosporine.
What you’ll find here isn’t theory. It’s what people actually deal with: how relative risk numbers in ads hide the truth, why seniors on opioids fall more, how hair thinning from exemestane is real but manageable, and why your insurance copay might not be helping your deductible. These aren’t abstract concepts. They’re daily decisions. And they all tie back to one thing: FDA drug safety isn’t a stamp on a bottle. It’s a living system—and you’re part of it. Know what to ask. Know what to watch. Know how to protect yourself.