Vitamin D Analog Selection Guide
Find Your Ideal Vitamin D Analog
Answer a few questions about your condition and treatment goals to get personalized recommendations based on clinical evidence.
When your doctor prescribes a vitamin D analog, you want to know why that specific drug was chosen and whether there are other options that might work better for you. Rocaltrol alternatives is a question many patients with chronic kidney disease or secondary hyperparathyroidism ask during appointments.
What is Rocaltrol (Calcitriol)?
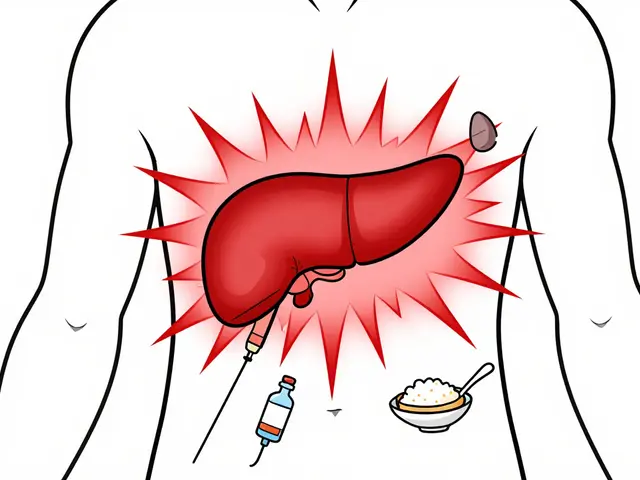
Rocaltrol (Calcitriol) is a synthetic form of the active hormone calcitriol, the hormonally active metabolite of vitamin D3 (cholecalciferol). It binds to the vitamin D receptor (VDR) in intestinal cells, kidneys, and bone, boosting calcium and phosphate absorption and suppressing parathyroid hormone (PTH) release. Approved by the FDA in 1995, Rocaltrol is mainly used to treat hypocalcemia caused by renal failure and to manage secondary hyperparathyroidism in patients on dialysis.
Why consider alternatives?
Even though Rocaltrol is effective, it isn’t a one‑size‑fits‑all solution. Its short half‑life, risk of hypercalcemia, and need for frequent dosing can be inconvenient. Some patients also experience high treatment costs or drug interactions that make other vitamin D analogs more attractive. Below we explore the most common alternatives and when they might be a better fit.
Key Alternative Vitamin D Analogs
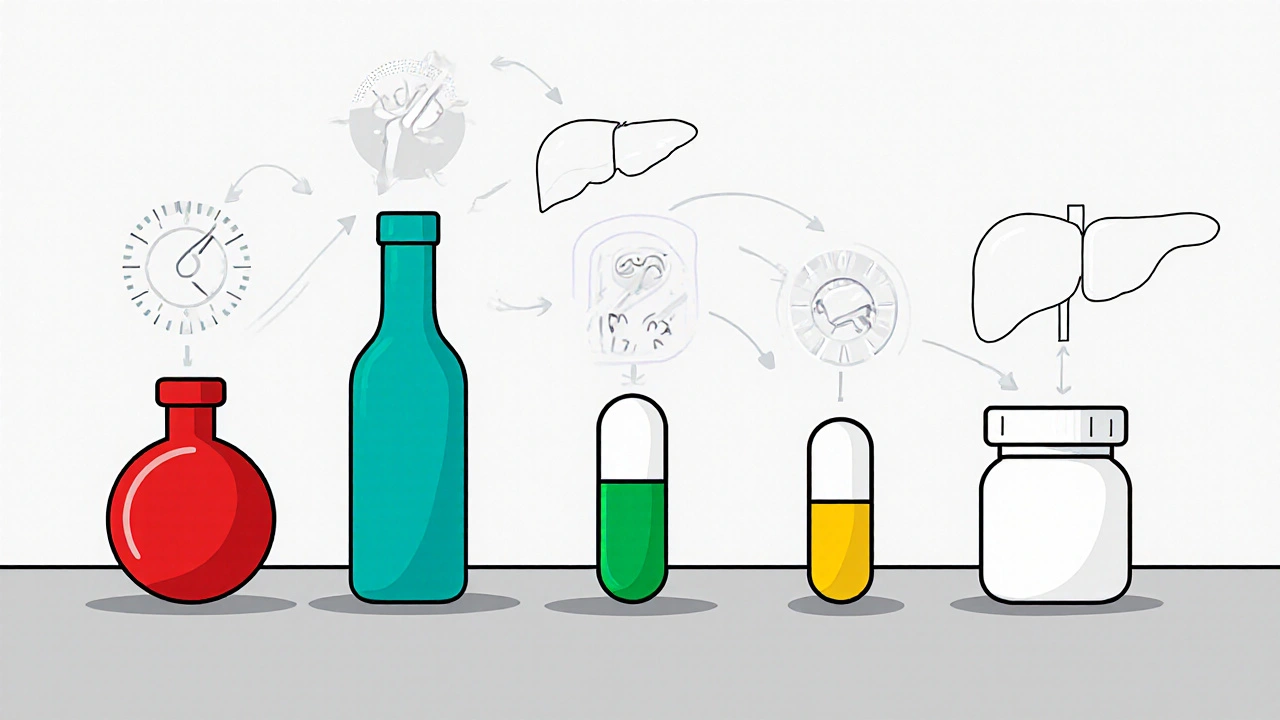
Each alternative shares the goal of activating the VDR but differs in potency, pharmacokinetics, and approved uses.
- Doxercalciferol is a synthetic analog of vitamin D2 that requires 25‑hydroxylation in the liver before becoming active. It’s often preferred in patients with high calcium levels because it produces a more gradual rise in serum calcium.
- Paricalcitol is a selective VDR activator designed to suppress PTH with a lower risk of hypercalcemia. It’s widely used in dialysis centers for secondary hyperparathyroidism.
- Alfacalcidol is a 1‑hydroxyvitamin D3 that requires only 25‑hydroxylation in the liver, making it useful for patients with liver impairment.
- Vitamin D3 (Cholecalciferol) is the natural form of vitamin D obtained from sunlight and diet. It must be hydroxylated in the liver and kidney to become active, so it’s less reliable in advanced kidney disease.
- Vitamin D2 (Ergocalciferol) is plant‑derived and follows the same activation pathway as D3 but is less potent and has a shorter duration of action.
Comparison Table: Rocaltrol vs Alternatives
| Attribute | Rocaltrol (Calcitriol) | Doxercalciferol | Paricalcitol | Alfacalcidol | Cholecalciferol (Vit D3) |
|---|---|---|---|---|---|
| Origin | Synthetic active vitamin D3 | Synthetic vitamin D2 analog | Synthetic selective VDR activator | 1‑hydroxyvitamin D3 | Natural vitamin D3 from skin/diet |
| Activation Needed? | No (already active) | Yes (liver 25‑hydroxylation) | No (direct VDR activation) | Yes (liver 25‑hydroxylation) | Yes (liver & kidney hydroxylation) |
| Half‑life (hours) | ≈6-8 | ≈12-14 | ≈15-20 | ≈8-10 | ≈15-20 (after conversion) |
| Typical Dose Form | Oral drops, capsules | Oral capsules | Oral capsules, IV | Oral capsules | Softgel, tablets |
| Primary Indication | Hypocalcemia, secondary hyperparathyroidism | Secondary hyperparathyroidism (dialysis) | Secondary hyperparathyroidism (dialysis) | Renal osteodystrophy, hypocalcemia | General vitamin D deficiency |
| Risk of Hypercalcemia | High | Moderate | Low to moderate | Moderate | Low (unless overdose) |
| Cost (US, 2025) | $30‑$45 per month | $40‑$55 per month | $45‑$60 per month | $25‑$40 per month | $10‑$20 per month |
When Rocaltrol Makes Sense
If you have:
- Documented hypocalcemia that needs a rapid rise in serum calcium,
- Early‑stage chronic kidney disease where the kidneys can still convert vitamin D
- An intolerance or contraindication to liver‑dependent analogs,
then the direct activity of Rocaltrol can be a real advantage. Its quick onset can prevent dangerous muscle cramps or cardiac arrhythmias that sometimes accompany low calcium levels.
Scenarios Where an Alternative Beats Rocaltrol
Consider swapping to another analog if you face any of these challenges:
- Frequent hypercalcemia: Paricalcitol’s selective receptor activation reduces calcium spikes.
- Liver dysfunction: Doxercalciferol and Alfacalcidol rely on liver hydroxylation; in severe liver disease, direct active forms like Rocaltrol may still be needed, but dosing becomes tricky.
- Cost constraints: Over‑the‑counter vitamin D3 supplements are far cheaper, though they aren’t sufficient for advanced CKD‑MBD.
- Convenience: Longer‑acting agents (Paricalcitol IV, Doxercalciferol) can be given three times a week instead of daily dosing.
Side‑Effect Profile Comparison
All vitamin D analogs share a core set of possible adverse events-mainly hypercalcemia and hyperphosphatemia. However, the incidence varies.
- Rocaltrol: Hypercalcemia reported in 15‑20% of dialysis patients; nausea and vomiting can accompany high calcium.
- Doxercalciferol: Hypercalcemia in 10‑12%; lower risk of sudden spikes due to slower activation.
- Paricalcitol: Hypercalcemia in 5‑8%; also associated with mild hypotension when given IV.
- Alfacalcidol: Similar to Rocaltrol but slightly less frequent calcium elevations.
- Cholecalciferol: Overdose can cause severe hypercalcemia, but therapeutic doses are rarely a problem.
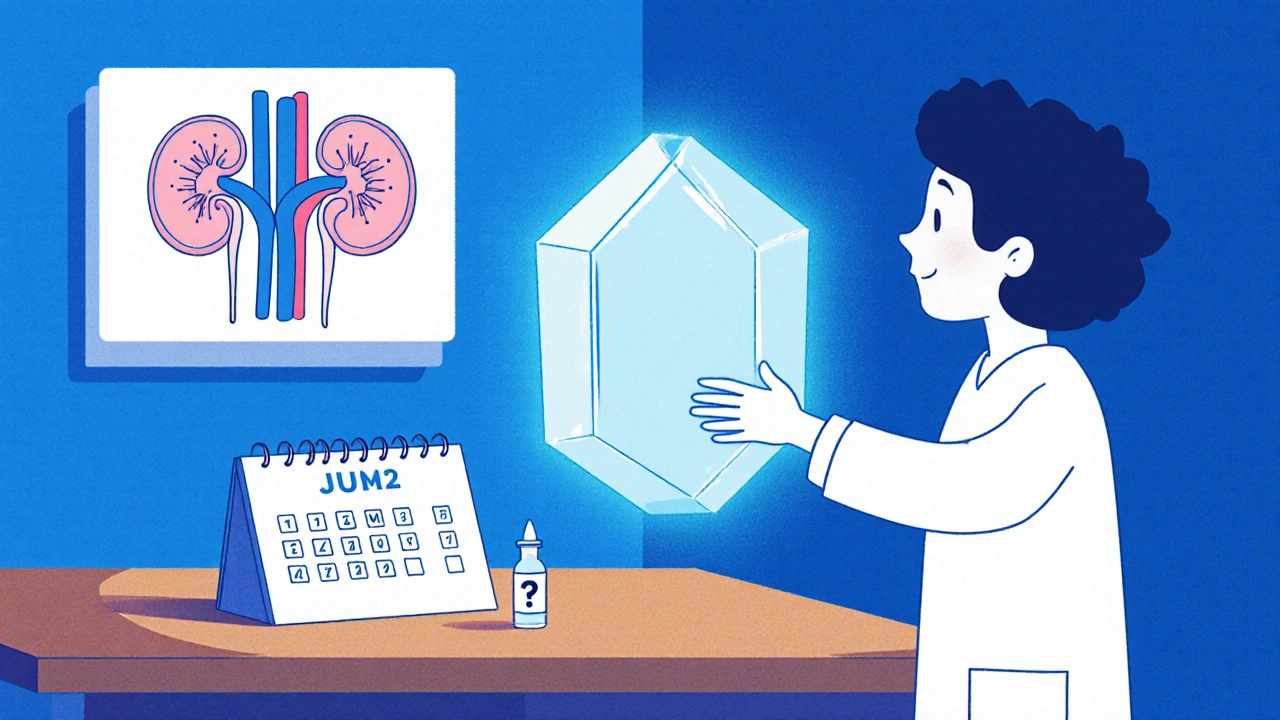
How to Choose the Right Agent
Think of the decision as a small checklist. Ask yourself:
- What is my primary goal-raise calcium quickly or gently suppress PTH?
- Do I have liver or kidney limitations that affect activation?
- Can I afford daily dosing or would a three‑times‑weekly schedule be better?
- Am I being closely monitored for calcium and phosphate levels?
Answering these questions with your nephrologist or endocrinologist will usually land you on the most suitable drug.
Practical Tips for Patients on Vitamin D Analogs
- Schedule blood tests every 1-3 months to catch calcium changes early.
- Take oral doses with meals to improve absorption.
- Avoid high‑calcium foods (e.g., fortified dairy) on days you receive a high dose.
- Report any new muscle weakness, heart palpitations, or unexplained nausea immediately.
- Keep a medication list handy; many phosphate binders interact with vitamin D analogs.
Future Directions: Newer Vitamin D Receptor Modulators
Research in 2024-2025 is exploring selective VDR modulators (SVDMs) that aim to keep PTH suppression while virtually eliminating hypercalcemia. Early‑phase trials of compounds like “Eldecalcitol” show promise, but they’re not yet FDA‑approved for the US market. When they become available, the comparison landscape will shift again, making it essential to stay informed.
Can I switch from Rocaltrol to an over‑the‑counter vitamin D supplement?
Only if your doctor confirms you no longer have renal‑related bone disease. Over‑the‑counter vitamin D3 cannot replace the active hormone needed for dialysis patients.
Why does Paricalcitol cause less hypercalcemia than Rocaltrol?
Paricalcitol is designed to activate the VDR in the parathyroid gland preferentially, so it suppresses PTH without driving excessive calcium absorption in the gut.
Is there a dosage advantage to using Alfacalcidol over Rocaltrol?
Alfacalcidol requires only one liver hydroxylation step, which can be useful in liver disease, but its dosing frequency is similar to Rocaltrol. The choice depends on individual metabolism.
How often should calcium levels be checked on these medications?
Initial monitoring is every 2‑4 weeks after a dose change, then every 3‑6 months once stable. Your clinician may adjust frequency based on risk factors.
Do any of these drugs interact with phosphate binders?
Yes. Calcium‑based binders can add to the calcium load from vitamin D analogs, raising hypercalcemia risk. Non‑calcium binders (e.g., sevelamer) are often preferred when using active vitamin D.



Terell Moore
Ah, the grand symposium of vitamin D analogs, where every manufacturer proudly parades its latest "innovation" as if the world needed another synthetic hormone. One can only marvel at the sheer optimism of prescribing Rocaltrol without first interrogating the pharmacokinetic labyrinth that separates it from its more "elegant" cousins. Yet, the article dutifully lists half‑life, cost, and hypercalcemia risk like they're exotic travel destinations.
Lennox Anoff
It is a moral outrage that clinicians continue to hand out Rocaltrol as a first‑line solution while ignoring the nuanced patient narratives that beg for personalized care. The so‑called “short half‑life” is not a flaw but a reminder that medicine is not a one‑size‑fits‑all industry. We must champion the quieter heroes-paricalcitol and doxercalciferol-who respect the delicate calcium equilibrium our bodies strive to maintain. Ignoring these alternatives feels like an ethical compromise of the highest order.
Abby W
Honestly, I’ve been on Rocaltrol for months and the occasional “calcium spikes” feel like a roller‑coaster ride 🎢. My roommate, who isn’t even on dialysis, asked if he could “borrow” my drops because he thought they’d boost his mood-yeah, that’s a boundary I’ve happily ignored 😅. If you’re juggling diet, phosphate binders, and an ever‑changing lab panel, just remember that every analog has its quirks, and sometimes a splash of humor is the best side‑effect you can tolerate.
Sarah Keller
Let’s cut to the chase: the choice of vitamin D analog is a strategic decision, not a whimsical preference. When you align the pharmacodynamics with the patient’s residual renal function, you empower the clinician to suppress PTH without catapulting calcium into dangerous territory. I recommend constructing a decision matrix-include liver function, calcium trends, dosing convenience, and cost-and then execute with the confidence of a surgeon wielding a scalpel. Do not settle for “good enough”; demand the optimal regimen for each individual.
Veronica Appleton
Check calcium every month and adjust dose as needed
krishna chegireddy
What the pharma giants don’t tell you is that they deliberately push Rocaltrol because it locks patients into a pricey, daily ritual. The alternative analogs are cheaper and safer, yet they stay in the shadows like secret weapons. Imagine a world where doctors were free to prescribe the best drug without a lobby pulling the strings. Until that day, we must read between the lines of every clinical guideline and question who truly benefits.
Nathan Comstock
When we examine the United States' regulatory landscape, it becomes evident that the approval of vitamin D analogs is as much a political theater as it is a scientific process. The Food and Drug Administration, praised for its rigor, often expedites drugs that align with domestic pharmaceutical interests, sidelining foreign alternatives that could offer comparable efficacy at a fraction of the cost. This bias fosters a dependency on homegrown products like Rocaltrol, even when international studies suggest that paricalcitol may reduce hypercalcemia incidents more effectively. Moreover, the reimbursement policies of Medicare and private insurers are structured to favor higher‑priced formulations, creating a financial incentive for clinicians to prescribe the costlier option. Patients, many of whom already grapple with the economic burden of dialysis, find themselves trapped in a cycle of recurring prescriptions that drain their wallets. The allied health community, aware of these dynamics, sometimes resorts to off‑label use of over‑the‑counter vitamin D3 in an attempt to mitigate expenses, albeit at the risk of suboptimal therapeutic outcomes. It is crucial to recognize that the pharmacokinetic profile of each analog dictates not only clinical efficacy but also the frequency of monitoring-a factor that can either alleviate or exacerbate the clinical workload. For instance, the longer half‑life of paricalcitol translates to fewer dosing intervals, which, in turn, reduces the logistical strain on dialysis centers. Conversely, the rapid turnover of Rocaltrol necessitates tighter surveillance, demanding more frequent lab draws and clinician interventions. From a nationalistic perspective, one might argue that supporting domestic drug manufacturers preserves American jobs and fosters innovation. Yet, such patriotic rhetoric should not eclipse the ultimate goal of patient‑centered care, which prioritizes safety, efficacy, and affordability above all else. In practice, a nuanced approach-leveraging the strengths of each analog while remaining vigilant about potential conflicts of interest-offers the most balanced pathway forward. The bottom line is that clinicians must wield both scientific evidence and critical awareness of systemic influences to navigate this complex therapeutic landscape. Only then can we ensure that the choice of vitamin D analog truly serves the patient, rather than the profit margins of corporate stakeholders.
Abhinav B.
From my experience both in India and abroad i see that the way we talk about vitamin d analogs is often missing the cultural context. Patients in different regions have varying diets, sunlight exposure, and traditional remedies that all influence their baseline levels. So when you hear someone say “just pick the cheapest drug” you are ignoring a whole tapestry of beliefs and practices that shape how they respond to therapy. I strongly suggest doctors ask about these factors before writing a script.
Lisa Woodcock
I hear that many of you feel overwhelmed by the sheer number of options and the constant monitoring required. It’s completely normal to feel that way, especially when you’re already managing dialysis and other meds. Remember that you’re not alone; there are support groups and patient advocates who can help you navigate these choices at your own pace.
Tamara Schäfer
Wow, this article really opened my eyes to how many variables are at play! I was always assuming that the cheapest option was automatically the best, but now i see the importance of half‑life and liver function. Let’s keep the conversation going and maybe we can find even more creative solutions together. :)
Tamara Tioran-Harrison
One must, with the utmost solemnity, applaud the comprehensive nature of this discourse while simultaneously lamenting the pervasive reliance upon Rocaltrol, a substance whose very nomenclature suggests a regal yet misguided sovereignty over calcium homeostasis. 😊
kevin burton
In summary, each vitamin D analog has its own set of strengths and weaknesses. Choose the one that fits your lab results, lifestyle, and budget, and keep an eye on calcium levels regularly.
Max Lilleyman
Honestly, if you’re still debating between Rocaltrol and paricalcitol after reading this, you might need a refresher course on endocrinology. 📚
Jonah O
Some say the guidelines are just a veil, a smokescreen crafted by unseen hands to steer our prescriptions toward predetermined ends. Yet we must question whether the true philosophy behind these recommendations is health or profit, and perhaps even something far more obscure that we are not yet ready to comprehend.