Every year, thousands of people are harmed because two drugs look or sound too much alike. It’s not a mistake in judgment. It’s not carelessness. It’s a system failure-and it’s happening most often with generic medications.
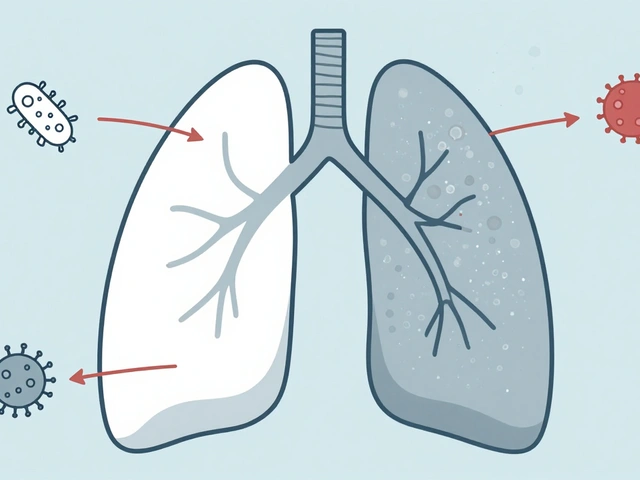
Picture this: a nurse hears a doctor say, "Give 5 mg of atenolol." But the label on the vial says "albuterol." Both start with "a," end with "ol," and sound nearly identical when spoken quickly in a busy ER. The patient gets the wrong drug. Their heart rate plummets. They’re rushed to ICU. This isn’t fiction. It’s a documented case from a U.S. hospital in 2021.
These aren’t rare glitches. They’re predictable, preventable, and shockingly common. About 25% of all medication errors worldwide come from look-alike, sound-alike (LASA) drug names. And generics? They’re the biggest contributors.
Why Generics Are the Main Culprit
Generic drugs are supposed to be cheaper, safer versions of brand-name medicines. But when multiple companies make the same generic, there’s no rule forcing them to make the pills look different. One company’s 10 mg hydroxyzine capsule might be white and round. Another’s hydralazine capsule? Also white and round. Same size. Same shape. Same color.
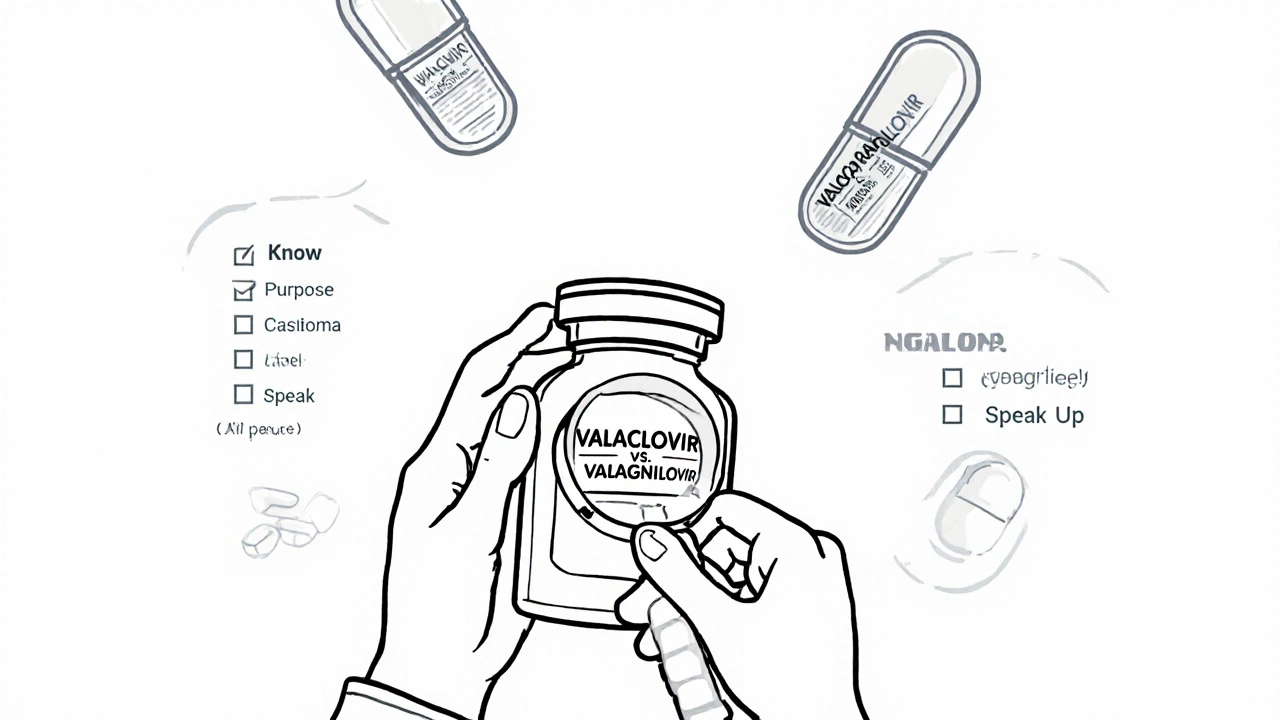
And the names? They’re often built from the same root. Valacyclovir and valganciclovir. Both start with "val." Both are used in transplant patients. One treats herpes. The other fights CMV. Mix them up? You’re not just giving the wrong drug-you’re risking organ rejection or deadly infection.
The problem isn’t the science. It’s the packaging. It’s the labeling. It’s the way names are chosen. Drug companies don’t test names for confusion. Regulatory agencies approve them based on chemical structure, not how they sound on a busy pharmacy counter.
The Real Cost of Confusion
It’s not just about patient harm. It’s about money. Medication errors cost the global health system $42 billion a year. LASA errors make up a big chunk of that.
In the U.S., 1 in 10 hospital patients experiences a medication error. Around 10% of those are LASA-related. In Australia, data from the Australian Commission on Safety and Quality in Health Care shows similar trends: over 200,000 medication incidents reported in a single year, with hundreds leading to serious injury or death.
And it’s not just hospitals. Pharmacies, nursing homes, even home care settings are at risk. A pharmacist filling a prescription for hydroxyzine (an antihistamine) might grab hydralazine (a blood pressure drug) because the bottles look identical and the names are just one letter apart.
One study found that 78% of pharmacists encounter LASA errors at least once a month. One in three reports near-misses weekly. That’s not luck. That’s a broken system.
Tall Man Lettering: A Simple Fix That Works
There’s a proven solution: tall man lettering.
It’s not fancy. It’s not expensive. It’s just using capital letters to highlight the parts of drug names that are different.
Instead of writing "prednisone" and "prednisolone," you write:
- PREDNISONE
- PREDNISOLONE
That small change makes a huge difference. A 2020 study across 12 hospitals showed a 67% drop in LASA errors after implementing tall man lettering in electronic prescribing systems and on drug labels.
It works because your brain doesn’t read every letter. It scans for patterns. When "SONE" and "SOLONE" are in bold caps, your eyes catch the difference before your fingers reach for the bottle.
The U.S. FDA and the European Medicines Agency both recommend tall man lettering. Yet, many hospitals still don’t use it. Why? Because it takes effort. Training. System updates. And someone has to care enough to make it happen.
Technology Is Finally Catching Up
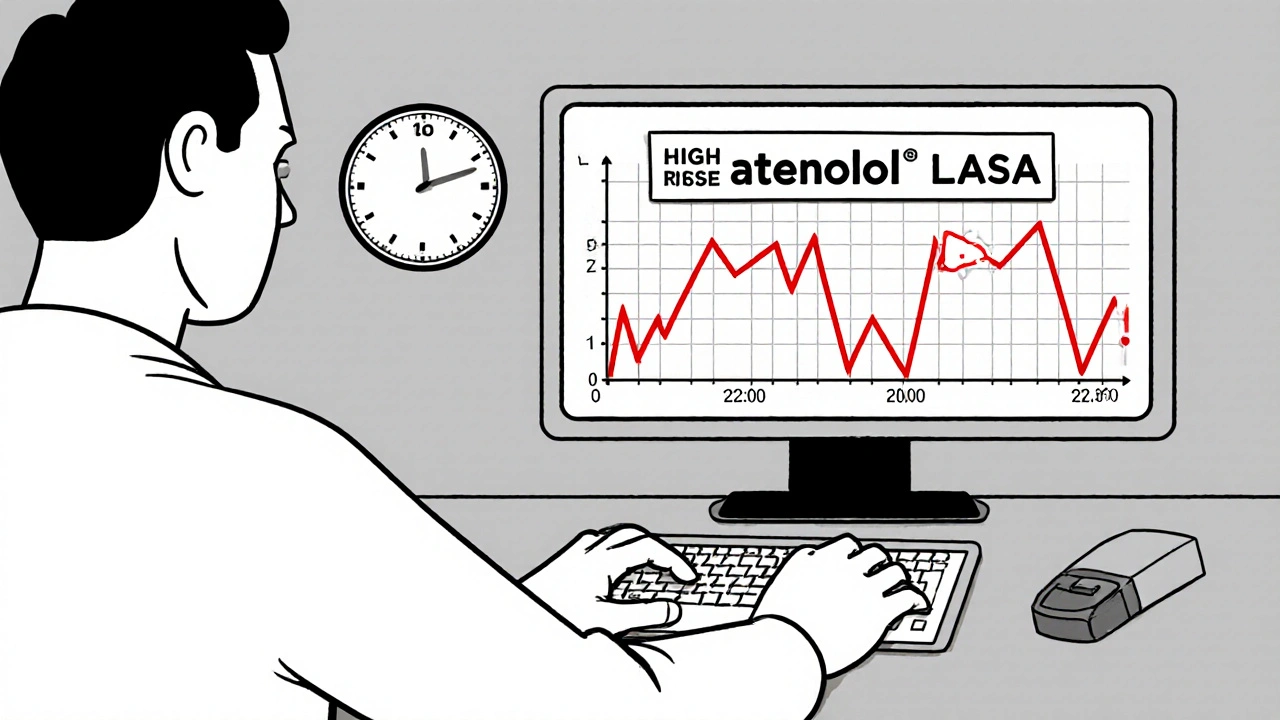
Artificial intelligence is now helping catch these errors before they happen.
Some hospital systems have embedded AI tools directly into their electronic health records (EHRs). When a doctor types "atenolol," the system flags: "Did you mean albuterol? High-risk LASA pair. Patient has asthma. Administering atenolol could cause bronchospasm."
One 2023 study in three major hospitals found that AI-powered alerts reduced LASA errors by 82%. The system flagged 98.7% of potential mistakes-and only gave false alarms in 1.3% of cases.
That’s not perfect. But it’s far better than nothing.
These tools don’t replace human vigilance. They support it. They give nurses and pharmacists a second set of eyes. And in high-stress moments-like during a code blue or at 2 a.m. when you’re running on three hours of sleep-that second set of eyes can mean the difference between life and death.
What You Can Do-Even If You’re Not a Doctor
You don’t need a medical degree to protect yourself or your loved ones from LASA errors.
Here’s what works:
- Know the purpose of your medication. If you’re given a new pill, ask: "What is this for?" If the answer is vague, push back. "I’m on hydroxyzine for anxiety. Why am I getting hydralazine?"
- Check the label every time. Don’t assume it’s the same as last month. Generic manufacturers change. Packaging changes. Names might look the same, but the pill inside could be different.
- Use the full name. Ask for both the generic and brand name. "Is this hydroxyzine, or is it Vistaril?" That extra step forces clarity.
- Speak up if something looks off. If the pill looks different, or the bottle feels wrong, say something. Pharmacists and nurses appreciate it. They’ve seen what happens when no one speaks up.
- Keep a list. Write down every medication you take-name, dose, purpose. Show it to every new provider. It’s your safety net.
Why This Isn’t Getting Fixed Faster
There’s a reason LASA errors keep happening. It’s not because no one knows how to fix them. It’s because fixing them requires coordination across industries.
Drug manufacturers don’t want to redesign packaging. Pharmacies don’t want to retrain staff. EHR vendors don’t prioritize it unless hospitals demand it. Regulators approve names without testing for confusion.
And here’s the hardest truth: we blame the person who made the mistake. The nurse. The pharmacist. The doctor. But Dr. David Bates from Harvard put it best: "LASA errors are a systems failure, not an individual error."
Blaming the frontline worker doesn’t stop the next mistake. Fixing the system does.
The Road Ahead
The World Health Organization’s "Medication Without Harm" campaign aims to cut severe medication errors by 50% by 2025. That’s ambitious. But possible.
Some places are already succeeding. Magnet-designated hospitals-those with the highest nursing standards-use an average of six LASA prevention strategies. Non-Magnet hospitals? Two.
The difference? Culture. Leadership. Investment.
When hospitals make LASA safety a priority, the numbers drop. When pharmacies use tall man lettering, barcode scanning, and AI alerts, errors vanish.
It’s not about more rules. It’s about better design. Better tech. Better communication.
And it starts with awareness.
If you’re taking generics-and most of us are-you’re at risk. But you’re not powerless. Know your meds. Ask questions. Speak up. And demand better from the system.
Because no one should die because two pills look too much alike.
What are look-alike, sound-alike (LASA) drugs?
Look-alike, sound-alike (LASA) drugs are medications with names or packaging that are visually or phonetically similar, making them easy to confuse. For example, hydroxyzine and hydralazine look alike in spelling and packaging, while albuterol and atenolol sound alike when spoken. These similarities can lead to dangerous prescribing, dispensing, or administration errors, especially with generic drugs where multiple manufacturers produce similar-looking products.
Why are generic drugs more prone to LASA errors?
Generic drugs are often made by multiple manufacturers, and there are no strict rules requiring standardized packaging, color, or shape. This means two different companies’ versions of the same generic drug can look identical. Plus, generic names often share common roots (like "val" in valacyclovir and valganciclovir), making them harder to distinguish. Brand-name drugs usually have unique names chosen to avoid confusion, but generics don’t have that same protection.
How common are LASA medication errors?
About 25% of all medication errors worldwide are caused by look-alike, sound-alike drug names, according to the World Health Organization and multiple peer-reviewed studies. In hospitals, these errors contribute to thousands of preventable injuries and hundreds of deaths each year. Pharmacists report encountering LASA errors at least once a month, with many seeing near-misses weekly.
What is tall man lettering, and does it work?
Tall man lettering uses capital letters to highlight the parts of drug names that differ. For example, PREDNISONE vs. PREDNISOLONE. This helps the brain quickly spot differences instead of scanning entire names. Studies show it reduces LASA errors by up to 67% in hospitals that implement it consistently. It’s simple, low-cost, and recommended by the FDA and WHO-but still not universally used.
Can technology help prevent LASA errors?
Yes. AI-powered clinical decision support systems in electronic health records can flag potential LASA errors in real time. One 2023 study showed an 82% reduction in errors after deploying these systems. They work by comparing prescribed names against known high-risk pairs and alerting clinicians before the medication is given. While not perfect, they’re one of the most effective tools available today.
What should I do if I think I’ve been given the wrong generic drug?
Don’t take it. Check the label against your prescription and medication list. Look at the pill’s color, shape, and imprint. Ask the pharmacist: "Is this the same as what I got last time?" If it looks different or the name seems confusing, ask for clarification. If you’re still unsure, call your doctor. It’s better to delay taking the medication than risk a dangerous mistake.
Are there any drugs I should be extra careful with?
Yes. High-risk LASA pairs include: hydroxyzine/hydralazine, albuterol/atenolol, clonidine/clonazepam, and valacyclovir/valganciclovir. These are frequently confused because of similar names and overlapping uses. If you take any of these, make sure you know the exact purpose of your prescription and double-check the label every time you refill it.
Why don’t drug companies change the names to avoid confusion?
Changing drug names is expensive and complicated. Brand-name drugs get unique names approved by regulators, but generic names are based on chemical structure, not safety. Once a generic is approved, changing its name requires re-filing with regulators, updating all labeling, and retraining staff-costs most manufacturers avoid unless forced. The FDA has rejected 34 drug names since 2021 due to LASA risks, but this only applies to new drugs, not existing ones.



Erika Puhan
Let’s be real-this isn’t about ‘human error.’ It’s about pharmaceutical capitalism prioritizing profit over patient safety. Generic manufacturers don’t redesign packaging because it costs money. Regulators don’t enforce naming standards because lobbying is easier than accountability. And hospitals? They’d rather blame the nurse than upgrade their EHR systems. We’re not talking about a glitch. We’re talking about a systemic betrayal dressed up as ‘efficiency.’
Edward Weaver
USA has the best healthcare tech in the world and we’re still letting pharmacists mix up hydroxyzine and hydralazine? Come on. We spend billions on fighter jets but can’t implement tall man lettering? This is why other countries laugh at us. Fix the damn system or stop pretending we’re #1.
Lexi Brinkley
THIS. IS. UNACCEPTABLE. 😡 I had a cousin almost die from this exact thing. They gave her clonidine instead of clonazepam. She went into seizures. Now she’s on disability. Why isn’t this on the news? Why isn’t Congress freaking out? 🤬
Kelsey Veg
so like… why dont we just call them diff names? like instead of valacyclovir and valganciclovir… why not like… ‘herpes pill’ and ‘cmv pill’? its not that hard. stop overcomplicating things. i mean… come on.
Alex Harrison
I work in a rural pharmacy and we use tall man lettering and barcode scanning. It’s not perfect but it cuts down on the near-misses. I’ve seen it work. The problem isn’t the tech-it’s the culture. Staff don’t get trained properly. Management doesn’t prioritize it. It’s not rocket science. It’s just… consistent effort. And nobody wants to do the work.
Jay Wallace
Let me be clear: this isn’t a ‘system failure.’ It’s a failure of intellectual rigor. If you can’t distinguish between ‘prednisone’ and ‘prednisolone’-you shouldn’t be handling medications. We’ve had 40 years of pharmacology education. If you’re still confusing ‘atenolol’ and ‘albuterol’… maybe you’re in the wrong profession. Technology is a crutch. Competence is the solution.
Lashonda Rene
I just want to say I really appreciate this post because I’ve been scared to take my meds for years now. I don’t trust the labels anymore. I used to just take what they gave me but after my grandma got the wrong thing and ended up in the hospital… I started writing everything down. I keep a little notebook in my purse. I show it to every pharmacist. I ask the same questions every time. It’s exhausting but I’d rather be annoying than dead. I wish more people did this.
Andy Slack
Change is possible. Look at Canada-they mandated tall man lettering in 2018. Errors dropped 60% in two years. We have the tools. We have the data. We just need leaders who care enough to push for it. This isn’t about blame. It’s about action. And I’m tired of waiting.
Rashmi Mohapatra
lol so you want us to believe that a country that can’t even fix its own healthcare system is gonna fix drug names? please. in india we just get the same pill in 5 different boxes with same name and same color. no one cares. you think america is better? haha. you’re dreaming.
Ankit Yadav
Thank you for writing this. I’m a nurse in Mumbai and we deal with this daily. We don’t have AI alerts or barcode scanners. We have memory, repetition, and each other. I ask my colleagues to say the full name out loud before handing over any med. It’s slow. It’s awkward. But it saves lives. Small steps matter. Don’t underestimate the power of asking, ‘Are you sure?’
Meghan Rose
Wait-so you’re saying I should double-check my meds every time? Even if I’ve taken them for 10 years? Isn’t that a little… paranoid? I mean, aren’t pharmacists supposed to be the experts? Why do I have to be my own safety net? This feels like gaslighting.
Steve Phillips
Let’s be dramatic for a second: this is the quiet genocide of the American middle class. A grandmother dies because a pharmacist grabbed the wrong bottle. A child goes into cardiac arrest because a nurse misheard a name. And who gets punished? NO ONE. The CEOs get bonuses. The regulators get promoted. The families get grief. This isn’t an error. It’s a crime-and it’s being covered up with PowerPoint slides and ‘best practices.’
Rachel Puno
My mom’s on hydroxyzine for anxiety. Last month, she got hydralazine by accident. She didn’t notice until her blood pressure dropped to 80/50. She called me crying. I’m so glad she spoke up. I’m so glad she had the list. Please, everyone-make a list. Write it down. Show it. Don’t assume. You’re not being difficult. You’re being smart.
Clyde Verdin Jr
Ugh. Another ‘woke’ healthcare post. Next you’ll tell us to hold hands and sing kumbaya while we dispense meds. Look-I’ve been in this field 20 years. People mess up. That’s life. You can’t eliminate human error. You can only blame the system when you’re too lazy to train your staff. Tall man lettering? Cute. But it won’t fix a dumb nurse who doesn’t pay attention.