Antibiotic Decision Tool
Antibiotic Selection Guide
This tool helps you understand which antibiotics may be most appropriate for specific infections based on medical guidelines. Always consult with your healthcare provider for personal medical advice.
Recommended Antibiotics
Select your infection type and patient factors to see recommendations.
When you or a loved one need an antibiotic, the sheer number of options can feel overwhelming. Levofloxacin is a widely‑prescribed fluoroquinolone that promises broad‑spectrum coverage, but is it always the right choice? This guide breaks down Levofloxacin compare factors, weighs the pros and cons against common alternatives, and gives you a clear picture of when each drug shines or falls short.
What Is Levofloxacin?
Levofloxacin is a synthetic, third‑generation fluoroquinolone antibiotic first approved by the FDA in 1996. It works by inhibiting bacterial DNA gyrase and topoisomerase IV, enzymes essential for DNA replication. The result? Bacteria can’t multiply, and the infection fades.
Levofloxacin’s strengths lie in its oral bioavailability (almost 100%), once‑daily dosing, and activity against a wide range of Gram‑negative and some Gram‑positive organisms. However, the fluoroquinolone class carries a reputation for tendon damage, QT‑prolongation, and growing resistance.
Key Alternatives to Consider
Below are the most common antibiotics doctors turn to when Levofloxacin isn’t ideal. Each belongs to a different class, offering a distinct safety and efficacy profile.
- Ciprofloxacin - another fluoroquinolone, slightly older, with stronger Gram‑negative coverage but weaker Gram‑positive activity.
- Moxifloxacin - a later‑generation fluoroquinolone that adds better activity against atypical pathogens and some anaerobes.
- Azithromycin - a macrolide that’s handy for respiratory infections and has a simpler side‑effect profile.
- Amoxicillin - a β‑lactam penicillin often first‑line for ear, sinus, and throat infections.
- Doxycycline - a tetracycline useful for atypical organisms, Lyme disease, and certain skin infections.
Comparison Table: Levofloxacin and Its Main Rivals
| Antibiotic | Class | Typical Indications | Key Advantages | Major Side Effects / Risks | Resistance Trends (2024) |
|---|---|---|---|---|---|
| Levofloxacin | Fluoroquinolone (3rd gen) | UTI, community‑acquired pneumonia, skin & soft‑tissue infections | Once‑daily dosing, excellent oral bioavailability, broad gram‑negative coverage | Tendon rupture, QT prolongation, CNS effects, C. difficile risk | Increasing resistance in E. coli & Pseudomonas (≈15% US) |
| Ciprofloxacin | Fluoroquinolone (2nd gen) | UTI, gastroenteritis, bone & joint infections | Strong gram‑negative activity, cheap | Same class risks, higher neurotoxicity, poor gram‑positive coverage | High resistance in Enterobacteriaceae (≈25%) |
| Moxifloxacin | Fluoroquinolone (4th gen) | CAP, COPD exacerbations, intra‑abdominal infections | Better atypical/anaerobic coverage, once‑daily | QT prolongation (more pronounced), liver enzyme elevation | Moderate resistance, still <10% for S. pneumoniae |
| Azithromycin | Macrolide | Respiratory infections, chlamydia, traveler's diarrhea | Long half‑life (once‑daily 5‑day course), fewer severe systemic effects | GI upset, potential for antibiotic‑associated arrhythmia, rising macrolide resistance | Macrolide resistance in S. pneumoniae ~30% (2024) |
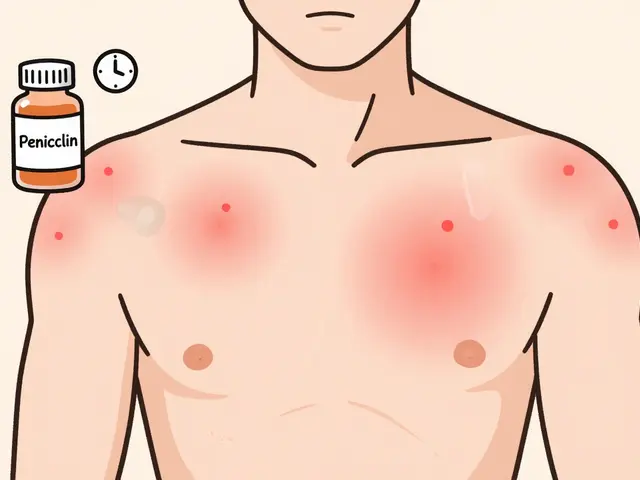
| Amoxicillin | Penicillin (β‑lactam) | Otitis media, sinusitis, streptococcal pharyngitis | Excellent safety, inexpensive, narrow spectrum reduces collateral damage | Allergy risk, limited gram‑negative activity, β‑lactamase resistance | High resistance in H. influenzae (≈35%) |
| Doxycycline | Tetracycline | Lyme disease, acne, atypical pneumonia | Broad coverage of intracellular pathogens, inexpensive | Photosensitivity, esophageal irritation, not for children <8yr | Low resistance overall, but emerging in V. cholerae |
When Levofloxacin Makes Sense
Think of Levofloxacin as the “go‑to” when you need a single pill that tackles a mixed bag of bacteria and you can’t afford multiple drugs. It’s especially handy for community‑acquired pneumonia (CAP) where both typical (Streptococcus pneumoniae) and atypical (Mycoplasma, Chlamydophila) bugs might be present. The once‑daily 750mg regimen also helps patients who struggle with complex dosing schedules.
In the U.S., the Infectious Diseases Society of America (IDSA) still recommends fluoroquinolones as a second‑line option for complicated urinary tract infections (cUTI) when oral β‑lactams aren’t suitable. If a patient has a known allergy to penicillins or macrolides, Levofloxacin often fills the gap.

Scenarios Where Alternatives Beat Levofloxacin
Not every infection needs the firepower of a fluoroquinolone. Overusing Levofloxacin fuels resistance and raises the chance of serious side effects. Here are common situations where you should reach for something else:
- Simple uncomplicated UTIs - Amoxicillin or trimethoprim‑sulfamethoxazole are usually enough and spare you the fluoroquinolone warning labels.
- Childhood ear or sinus infections - pediatric dosing of Azithromycin (or amoxicillin) is safer; fluoroquinolones are not FDA‑approved for children unless no alternative exists.
- Atypical pneumonia in patients with QT concerns - Doxycycline avoids the cardiac risk while covering the same pathogens.
- Patients on warfarin or other QT‑prolonging drugs - co‑prescribing Levofloxacin can tip the balance; a macrolide or a β‑lactam may be gentler.
Safety Profile: What to Watch For
All fluoroquinolones share a black‑box warning. The biggest red flags are tendon rupture (especially Achilles), peripheral neuropathy, and central nervous system disturbances like dizziness or vivid dreams. The risk spikes in people over 60, those on steroids, or patients with renal impairment.
Other antibiotics have their own cautions. Azithromycin can cause temporary hearing loss at very high doses, while Amoxicillin can trigger severe allergic reactions in about 0.1% of users. Knowing the patient’s medical history is the first step toward picking the safest option.
Cost and Accessibility
In Australia, a standard 10‑day pack of generic Levofloxacin runs around AUD30‑40, whereas branded versions can hit AUD80. By contrast, Amoxicillin is often under AUD10 and covered by most PBS listings. Azithromycin sits in the AUD15‑20 range for a 5‑day course.
Insurance formularies frequently place fluoroquinolones in higher tiers, requiring co‑payments. If cost is a major factor, discuss generic alternatives with your GP or pharmacist.

Guidelines and Stewardship
Antimicrobial stewardship programs worldwide urge clinicians to reserve fluoroquinolones for cases where no suitable narrow‑spectrum agent exists. The 2023 WHO AWaRe classification lists fluoroquinolones under the “Watch” category, indicating higher resistance potential.
In practice, that means: start with the narrowest effective drug, reassess after culture results, and de‑escalate if possible. If you’re already on Levofloxacin and cultures later show a penicillin‑sensitive organism, switching to amoxicillin can shorten therapy and reduce side‑effect risk.
Quick Decision Cheat‑Sheet
- Identify infection type (respiratory, urinary, skin, etc.).
- Check patient‑specific factors: age, allergies, cardiac history, renal function.
- Match the organism’s typical susceptibility profile.
- Gram‑negative dominant → consider Levofloxacin or Ciprofloxacin.
- Atypical or intracellular → Azithromycin or Doxycycline.
- Gram‑positive only → Amoxicillin or a cephalosporin.
- Weigh side‑effect profile and cost.
- High tendon‑rupture risk → avoid Levofloxacin.
- QT concerns → choose Doxycycline or Amoxicillin.
- Finalize prescription, document rationale, and plan follow‑up culture review.
Bottom Line
Levofloxacin is a powerful, convenient option for mixed‑organism infections, but it isn’t a one‑size‑fits‑all. Weigh its broad spectrum against the higher safety warnings and rising resistance. In many routine cases, older, cheaper, and gentler drugs like amoxicillin or azithromycin get the job done without the baggage.
Frequently Asked Questions
Can I take Levofloxacin if I’m pregnant?
Levofloxacin is classified as Pregnancy Category C in the U.S., meaning risk cannot be ruled out. Most clinicians avoid it during the first trimester and opt for safer alternatives like amoxicillin unless no other option exists.
How long after stopping Levofloxacin can I safely resume exercise?
Because of the tendon‑rupture warning, doctors usually advise waiting at least two weeks after the last dose before engaging in high‑impact activities.
Is there a generic version of Levoflox?
Yes, generic levofloxacin is widely available and costs considerably less than the brand‑name Levoflox tablets.
What should I do if I develop a rash while on Levofloxacin?
Stop the medication immediately and contact your healthcare provider. A rash could signal an allergic reaction, which may require an antihistamine or a switch to a different antibiotic.
How does antibiotic resistance affect my choice of Levofloxacin?
Rising resistance, especially amongE.coli andPseudomonas, means Levofloxacin may fail where it once succeeded. If you live in an area with high local resistance rates, doctors often favor narrower agents or order a culture before prescribing.




Kristen Moss
Look, if you think levofloxacin is just another foreign‑made pill, think again – the good old U.S. FDA has vetted it for years, and you’re better off trustin’ the home‑grown meds than some overseas knock‑offs. No need to overcomplicate things, just stick with what’s proven here.
Rachael Tanner
Levofloxacin’s pharmacokinetic profile is remarkably favorable; its near‑perfect oral bioavailability translates to consistent plasma concentrations, which is a boon for compliance. Moreover, the drug’s concentration‑dependent killing mechanism ensures rapid bacterial eradication when dosing is optimized. The once‑daily regimen mitigates the risk of missed doses, a common pitfall with multi‑day courses of amoxicillin or doxycycline. Its spectrum, while broad, does exclude certain anaerobes, prompting clinicians to consider metronidazole adjunctively in mixed infections. Resistance trends, however, are a growing concern: surveillance data from 2024 indicate a 15 % resistance rate among community‑acquired E. coli isolates in the United States, underscoring the necessity of antimicrobial stewardship. In contrast, ciprofloxacin, though potent against gram‑negative rods, suffers from higher neurotoxicity and poorer gram‑positive coverage, limiting its utility in skin and soft‑tissue infections. Moxifloxacin, a fourth‑generation fluoroquinolone, expands coverage to atypical pathogens and offers superior lung penetration, yet its propensity for QT prolongation demands electrocardiographic monitoring in at‑risk patients. Azithromycin, while safe and convenient, faces escalating macrolide resistance, particularly in Streptococcus pneumoniae, rendering it suboptimal for empiric therapy in certain regions. Amoxicillin remains a cornerstone for otitis media and sinusitis, but beta‑lactamase‑producing organisms can render it ineffective unless paired with a clavulanate inhibitor. Doxycycline’s utility in atypical infections and its anti‑inflammatory properties make it a versatile agent, though photosensitivity and gastrointestinal upset limit its use in some populations. Clinicians must weigh these nuances against patient‑specific factors such as comorbidities, drug interactions, and adherence potential. Ultimately, the decision matrix for selecting levofloxacin versus its alternatives is multifactorial, integrating microbiological data, pharmacodynamics, safety profiles, and cost considerations. A tailored approach, guided by local antibiograms and patient history, will yield the most favorable outcomes.
Debra Laurence-Perras
Hey everyone, just wanted to add a quick note that while levofloxacin is a solid option, it’s always good to look at the whole picture – think about allergies, other meds you’re on, and the specific bug you’re fighting. If you have any doubts, chatting with a pharmacist can give you a clearer path forward.
dAISY foto
Yo, I totally feel you Debra! levofloxacin is like that super‑charged car you see in movies – looks awesome but you gotta check the brakes first. If you’re worried ‘bout tendons or that QT thing, maybe try a chill macrolide instead. Also, don’t forget that sometimes the simplest penicillin can do the trick, no need to over‑engineer the cure. Keep vibing and stay safe, fam!
Sam Franza
Levo is a good choice for many infections but consider allergies and other meds. Talk to your doctor about the best fit for you.
Raja Asif
Listen, the American medical system has vetted levofloxacin thoroughly – it’s not some half‑baked foreign invention. If you’re still debating, you’re just falling for marketing hype from overseas pharma. Stick with what’s proven in the US.
Cynthia Sanford
Hope you all feel better soon! Levo works great for many, but if you notice any weird side effects, let a doc know right away. Stay positive and take care of yourself!
Yassin Hammachi
It’s interesting how each antibiotic carries its own narrative – levofloxacin’s story is one of convenience, yet also of caution. Balancing efficacy with safety is a philosophical exercise in medicine, reminding us that every choice reflects larger values about risk and reward.
Irene Harty
One must consider, in a world where pharmaco‑economic interests dominate, that levofloxacin’s prominence may be less about clinical superiority and more about covert lobbying orchestrated by multinational conglomerates. The data presented in mainstream journals often omit the darker undercurrents of regulatory capture, leaving patients in the dark about the true risk‑benefit calculations.
Jason Lancer
Levofloxacin is fine.
Brooks Gregoria
Ah, the classic levo‑vs‑alternatives debate – a perfect illustration of how we love to complicate the obvious. Sure, levo works, but isn’t the real question why we keep reaching for broad‑spectrum agents when narrow‑spectrum options could spare our microbiome? Perhaps we should challenge the status quo and re‑evaluate our default prescriptions.