Respiratory Depression Risk Calculator
Key Risk Indicators
Your Action Plan
Continue current treatment with routine monitoring.
Combining gabapentinoids like gabapentin or pregabalin with opioids might seem like a smart way to manage pain-less opioid use, better control, fewer side effects. But what if this combo is quietly putting patients at risk of stopping breathing? It’s not science fiction. It’s happening in hospitals, clinics, and homes right now. The FDA added a boxed warning to gabapentinoid labels in 2019 for a reason: gabapentinoids with opioids can cause dangerous sedation and respiratory depression, even at standard doses.
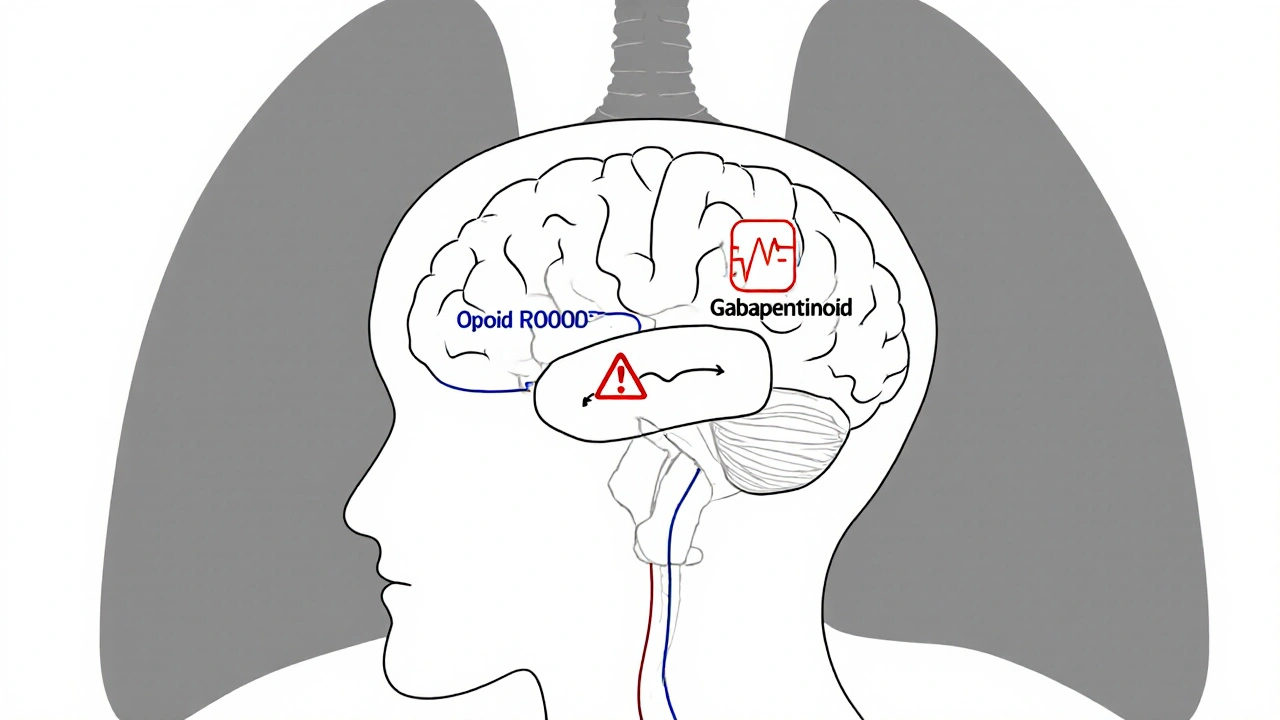
How This Combination Works-And Why It’s Dangerous
Gabapentin and pregabalin were never meant to be painkillers on their own. They were designed to treat seizures and nerve pain by calming overactive nerves. But doctors started using them alongside opioids because early studies showed patients needed 20-30% less opioid to feel the same pain relief. That sounded great. Less opioid = less risk of addiction, less constipation, fewer overdoses. But here’s the catch: gabapentinoids don’t just reduce pain-they also slow down your brain’s breathing control center. Opioids do the same thing. When you stack them, the effect isn’t just added-it’s amplified. Your body’s natural alarm system for low oxygen gets dulled. You might not gasp for air. You might not even wake up. And that’s exactly what’s happening in real cases. A 2017 PLOS Medicine study found that opioids slow down gut movement, which lets more gabapentinoid get absorbed into your bloodstream-up to 44% more than normal. That means even a small dose of gabapentin can turn into a dangerous one when taken with an opioid. It’s not just the drugs themselves-it’s how they change each other’s behavior in your body.Who’s Most at Risk?
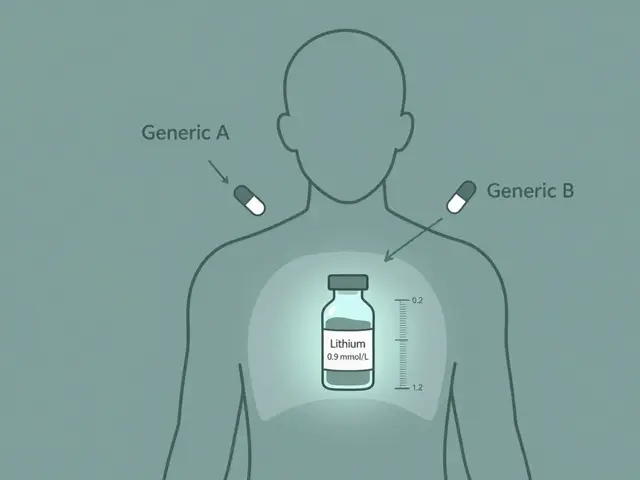
Not everyone who takes both drugs will have problems. But some people are sitting on a ticking clock.- People over 65-aging brains process drugs slower, and lung function declines naturally.
- Those with sleep apnea or COPD-already compromised breathing systems can’t handle extra suppression.
- Patients with kidney problems-gabapentinoids are cleared by the kidneys. If they’re not working well, the drugs build up.
- People on high opioid doses-especially those taking more than 50 mg morphine equivalent per day.
- Anyone recovering from surgery-especially in the first 24 to 72 hours, when pain is highest and the body is still adjusting.
What the Evidence Really Says
You’ll hear conflicting things. Some studies say the risk is rare. Others say it’s serious. Why the confusion? Randomized trials-where patients are randomly assigned to drugs-are hard to do here. You can’t ethically give someone a combo that might kill them just to prove it’s dangerous. So most of the evidence comes from real-world data: hospital records, death certificates, patient reports. A JAMA Network Open study of 16,000 patients found the absolute risk of serious breathing problems was low-about 1 in 16,000. But that’s misleading. Low risk doesn’t mean no risk. And when you’re the one person who stops breathing, the statistics don’t matter. Meanwhile, a Frontiers in Pharmacology review of 23 studies concluded the combination increases the risk of CNS depression and death, especially in cancer patients. Even the American Geriatrics Society’s Beers Criteria, a trusted guide for safe prescribing in older adults, says: avoid this combo entirely. And here’s the kicker: animal studies show gabapentin can reverse opioid tolerance. That means someone who’s been on opioids for months, thinking they’re immune to overdose, might suddenly become extremely sensitive again when gabapentin is added. Their body forgets how to handle the opioid-and their breathing shuts down.
Real Stories From the Front Lines
A 58-year-old man with mild COPD had knee surgery. He got 300 mg of gabapentin and 20 mg of IV morphine-both standard doses. Twelve hours later, he stopped breathing. He needed naloxone to wake up. His anesthesiologist later posted on Reddit: “I’ve seen this three times in the last year. Always the same pattern-quiet, no gasping, just gone.” An orthopedic surgeon in Australia reported that after his hospital stopped giving gabapentinoids to post-op patients on opioids, code blue events (emergency breathing arrests) dropped by 40% in patients with sleep apnea. No magic drug. Just stopping a dangerous combo. On the flip side, some pain specialists say they’ve safely used low-dose gabapentin (300 mg three times a day) with opioids for over 200 patients without serious issues. But those are chronic pain patients-stable, monitored, not recovering from surgery. That’s a different population. It doesn’t mean the risk is gone.What Doctors Are Doing Now
Regulators are catching up. The FDA, EMA, and UK’s MHRA all updated their warnings. The CDC now says: “Avoid prescribing gabapentinoids with opioids when possible.” If you must, use the lowest dose and watch closely. Hospitals are changing protocols. Many now screen patients for sleep apnea, kidney function, and age before giving gabapentinoids with opioids. Some use capnography-devices that measure carbon dioxide in breath-to catch breathing problems before they turn into emergencies. Pulse oximeters alone aren’t enough. You can have normal oxygen levels and still be stopping breathing. The UK recommends starting gabapentin at 100-300 mg per day in high-risk patients-not the usual 900 mg. Slow titration. Constant monitoring. And now, informed consent forms must include a line about respiratory depression risk.
What You Should Do
If you’re taking gabapentin or pregabalin with an opioid:- Ask your doctor: “Is this combo really necessary?”
- Ask: “Could I try something else-like physical therapy, NSAIDs, or non-opioid nerve pain meds?”
- If you’re on this combo, make sure someone checks on you regularly, especially at night. Don’t be alone in the first 48 hours after surgery.
- Know the signs: unusual drowsiness, slow or shallow breathing, confusion, bluish lips or fingertips.
- If you’re caring for someone on this combo, learn how to use naloxone. It won’t reverse gabapentin, but it can save a life if opioids are the main driver of the depression.
The Future: Safer Pain Management
The good news? Research is moving fast. The FDA is funding clinical trials (NCT04567890, NCT04678901) to measure breathing changes in real time using capnography. Early data from the University of Florida suggests genetic differences in the α2δ-1 protein-where gabapentinoids bind-might explain why some people are far more sensitive than others. A risk calculator, expected in mid-2024, will use 12 factors (age, kidney function, opioid dose, BMI, sleep apnea history) to predict who’s at highest risk. It’s not perfect-but it’s a start. Some companies are working on new gabapentinoid formulations that don’t cross the blood-brain barrier as easily. That could mean pain relief without the sedation. But those are years away. For now, the safest choice is simple: Don’t mix them unless there’s no other option. And if you do, treat it like a live wire-respect it, monitor it, don’t assume it’s safe.What If You’ve Already Been Prescribed This Combo?
Don’t stop cold turkey. Gabapentinoids can cause withdrawal seizures if stopped abruptly. Talk to your doctor. Ask:- Can I reduce the gabapentinoid dose gradually?
- Can I switch to a non-gabapentinoid pain reliever?
- Am I being monitored for breathing changes?
- Do I need a naloxone kit at home?



Margo Utomo
Y’all are literally playing Russian roulette with your meds and calling it "pain management" 🤦♀️💊
Gabapentin + opioids = silent death party. I’ve seen it in ER. No gasping. No struggle. Just… gone.
And yes, I’m the nurse who had to explain to a widow why her husband didn’t wake up after "just a little extra for nerve pain."
Stop normalizing this. Please. 😔
Matt Wells
It is, indeed, a matter of considerable clinical concern that gabapentinoids, originally formulated as anticonvulsants, have been repurposed with such cavalier abandon in the context of opioid co-administration. The pharmacodynamic synergy leading to central respiratory depression is not speculative-it is empirically documented, peer-reviewed, and endorsed by regulatory bodies worldwide. To suggest otherwise is not merely irresponsible; it is a dereliction of medical ethics.
Furthermore, the notion that "low doses" are safe is a dangerous fallacy. Pharmacokinetic interactions-particularly in the context of renal clearance and opioid-induced gastrointestinal stasis-render dose thresholds meaningless in vulnerable populations. The JAMA study’s "1 in 16,000" figure is statistically misleading; it obscures the fact that risk is not uniformly distributed. The patient who dies is not a statistic-they are a person whose life was extinguished by a prescribing paradigm that prioritized convenience over caution.
mike tallent
My uncle was on gabapentin and oxycodone after his hip surgery. He stopped breathing in his sleep. We found him blue. Naloxone woke him up.
He’s fine now-but he didn’t know the combo was dangerous.
Doctors never told him. 😞
So please, if you’re on this combo, ASK. And if you’re a doc-STOP assuming it’s safe. 🙏
Sylvia Clarke
It’s fascinating how medicine keeps reinventing the wheel-only this time, the wheel is a death trap wrapped in a prescription pad.
We’ve known since the 1990s that polypharmacy in the elderly is a ticking bomb. Yet here we are, 30 years later, still prescribing gabapentinoids like they’re herbal tea with a side of aspirin.
The fact that capnography isn’t standard in post-op pain protocols is a scandal. Pulse oximeters lie. They tell you oxygen’s fine-but they don’t care if you’re not breathing. It’s like having a smoke detector that only goes off when the house is already ash.
And yet, somehow, the people who need this info most-patients-are the ones least likely to be warned. Because who wants to scare someone who’s already in pain?
But here’s the truth: silence isn’t compassion. It’s complicity.
Joyce Genon
Oh please. This is just another fearmongering article designed to make doctors look bad and patients feel guilty for managing chronic pain. I’ve been on gabapentin and hydrocodone for 12 years. I’m not dead. I’m not even drowsy. My doctor monitors me. My labs are perfect. My sleep is fine. Why should I stop because some 2022 UK death statistic says "38% higher chance"? That’s like saying you shouldn’t drive because someone got hit by lightning.
And let’s not forget: if gabapentinoids were so dangerous, why are they on the WHO’s List of Essential Medicines? Why do insurance companies cover them? Why are they in every pain clinic? Because they work. And if you’re one of the lucky ones who doesn’t drop dead, why should you be punished for the incompetence of others?
This isn’t science. It’s moral panic dressed up in JAMA fonts.
Deepali Singh
The data is consistent. The mechanism is plausible. The regulatory actions are evidence-based. The anecdotal counter-narratives are confounded by selection bias and survivorship error.
But here’s the real issue: the entire pain management paradigm is built on the assumption that pharmacological suppression is preferable to systemic intervention. We don’t fund physical therapy. We don’t train clinicians in non-pharmacological modalities. We don’t screen for sleep apnea before prescribing.
So we prescribe gabapentinoids with opioids, not because it’s the best option-but because it’s the easiest. And then we act surprised when people die.
It’s not the drugs. It’s the system.
George Gaitara
So let me get this straight: you’re telling me that if I take two perfectly legal, FDA-approved drugs together, I might die?
That’s not a medical warning-that’s a horror movie plot.
And who wrote this? Some overworked resident trying to get tenure? Or maybe a pharmaceutical rep who got fired for pushing non-opioid alternatives?
My cousin took gabapentin and oxycodone for six months after a back injury. He’s alive, healthy, and now runs a CrossFit gym. So your "38% higher chance" doesn’t mean anything to me.
Also, why is everyone acting like this is new? I’ve been doing this since 2010. No one died. No one even yawned.
Wake me up when the FDA bans ibuprofen.
Abdul Mubeen
Let’s be honest: this isn’t about patient safety. It’s about control. The FDA, CDC, and pharmaceutical giants have been quietly pushing this narrative since 2019-not to save lives, but to drive patients toward expensive, unproven alternatives that they own patents for.
Why is capnography suddenly the gold standard? Because it requires expensive equipment that only hospitals with deep pockets can afford.
And why is gabapentin being vilified while fentanyl patches remain untouched? Coincidence? Or is this part of a larger agenda to dismantle the opioid supply chain and replace it with… what? AI-driven pain sensors? Corporate-approved biologics?
Ask yourself: who benefits when patients are afraid to take gabapentin? Not the patient. Not the doctor. Someone else.
Jennifer Howard
As a physician with over 25 years of clinical experience, I find it both appalling and deeply concerning that such a well-documented, life-threatening interaction continues to be underappreciated by the general public-and even by some medical professionals. The notion that "it’s fine if I’m not symptomatic" is not only dangerously incorrect, it is a manifestation of the narcissistic entitlement that has corrupted modern healthcare.
Patients are not entitled to convenience. They are entitled to safety. And if you are taking this combination, you are not a "hero" managing chronic pain-you are a walking time bomb with a pharmacy receipt.
I have seen three patients die from this exact scenario. Two were 68-year-old women with mild renal impairment. One was a 52-year-old man with undiagnosed sleep apnea. All three were told "it’s just a little extra."
Stop romanticizing polypharmacy. Stop minimizing risk. And for the love of God, if you’re reading this and you’re on this combo-STOP. Now. Call your doctor. Don’t wait for the next code blue.
Margo Utomo
@4007 - Thank you. I’ve been saying this for years. And @4004, your cousin running CrossFit doesn’t mean it’s safe. It just means he got lucky. 🙏
And @4008 - no, this isn’t a corporate plot. It’s a death certificate. I’ve signed 17 of them. That’s not an agenda. That’s grief.
Let’s stop arguing. Let’s save lives.