Sedation Risk: What You Need to Know About Drug Interactions and Safety
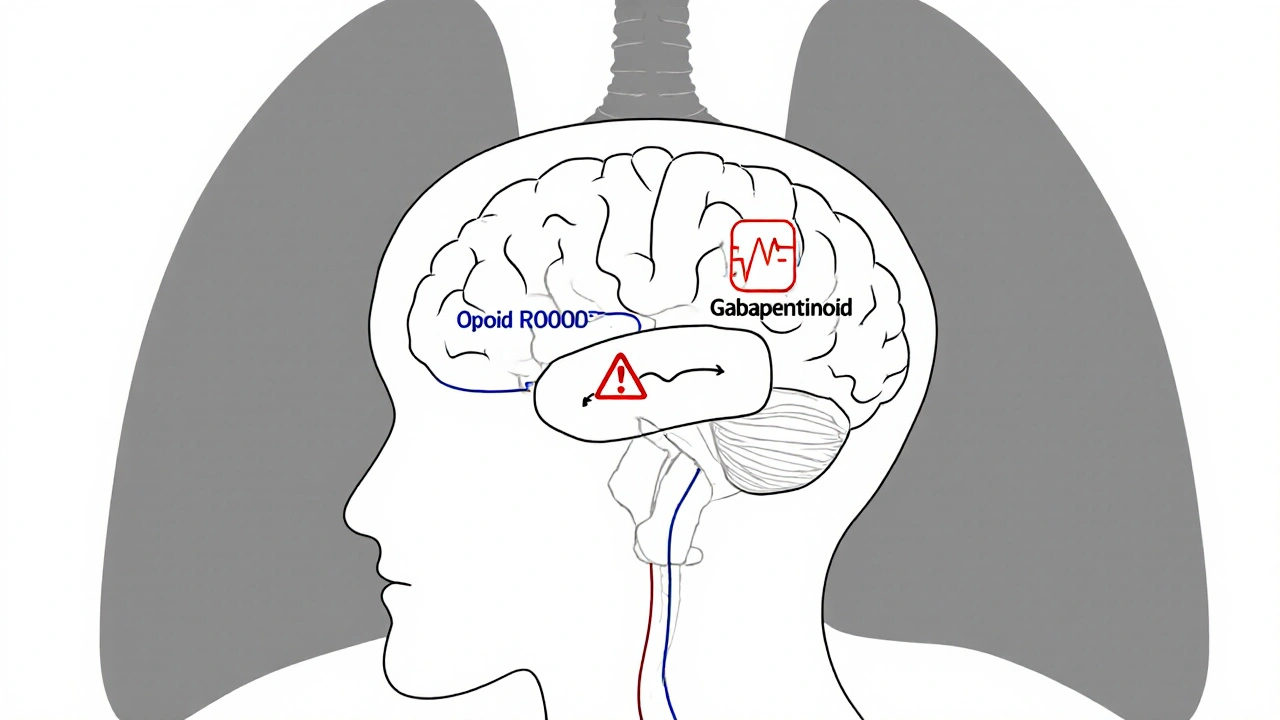
When you hear sedation risk, the chance that a medication or combination of drugs causes dangerous breathing problems, low blood pressure, or unresponsiveness. Also known as anesthesia-related complications, it’s not just about getting sleepy—it’s about whether your body can handle the chemical load. This isn’t theoretical. People end up in emergency rooms every year because they took a sleep aid with their blood pressure pill, or a painkiller with their anxiety med, and didn’t realize the combo could slow their breathing to dangerous levels.
Drug interactions, when one medicine changes how another works in your body are the silent engine behind most sedation risks. Take CYP3A4 interactions, a liver enzyme system that breaks down over half of all prescription drugs. Drugs like lopinavir/ritonavir block it, causing other sedatives to build up to toxic levels. That’s why someone on HIV meds might overdose on a common anxiety pill—even if they took the right dose. It’s not about being careless. It’s about systems most doctors don’t fully explain.
And it’s not just pills. Sedative side effects, the unintended outcomes of drugs meant to calm or induce sleep get worse with age, kidney trouble, or liver disease. Seniors are especially at risk. A single dose of a muscle relaxer or sleep aid can send them into confusion or respiratory failure. That’s why doctors now avoid certain drugs like glyburide or benzodiazepines in older patients—not because they’re bad, but because the body can’t clear them fast enough.
What you can’t see is often the most dangerous. Many people don’t realize their daily supplements—like melatonin, valerian, or even CBD—can add to sedation risk. They think natural means safe. It doesn’t. These substances work on the same brain pathways as prescription sedatives. Combine them, and you’re stacking the deck.
Monitoring matters. If you’re on a drug like esketamine or methadone, you’re not just taking a pill—you’re entering a system that requires blood pressure checks, breathing observation, and follow-up. These aren’t just hospital rules. They’re lifesavers. The same logic applies at home. If you’re starting a new medication, ask: Could this make me too sleepy? Could it clash with what I’m already taking? Don’t assume your pharmacist or doctor knows every combo. They’re juggling hundreds of patients. You’re the only one who knows your full list.
There’s no magic bullet to eliminate sedation risk. But there are clear steps: know your meds, track what you take, and speak up when something feels off. The posts below break down real cases—from HIV treatments that boost sedative levels, to painkillers that trip up older adults, to how even common supplements can turn harmless routines into emergencies. You won’t find fluff here. Just facts, patterns, and what actually works to keep you safe.