Ototoxic Antibiotics: What They Are and Which Ones Can Damage Your Hearing
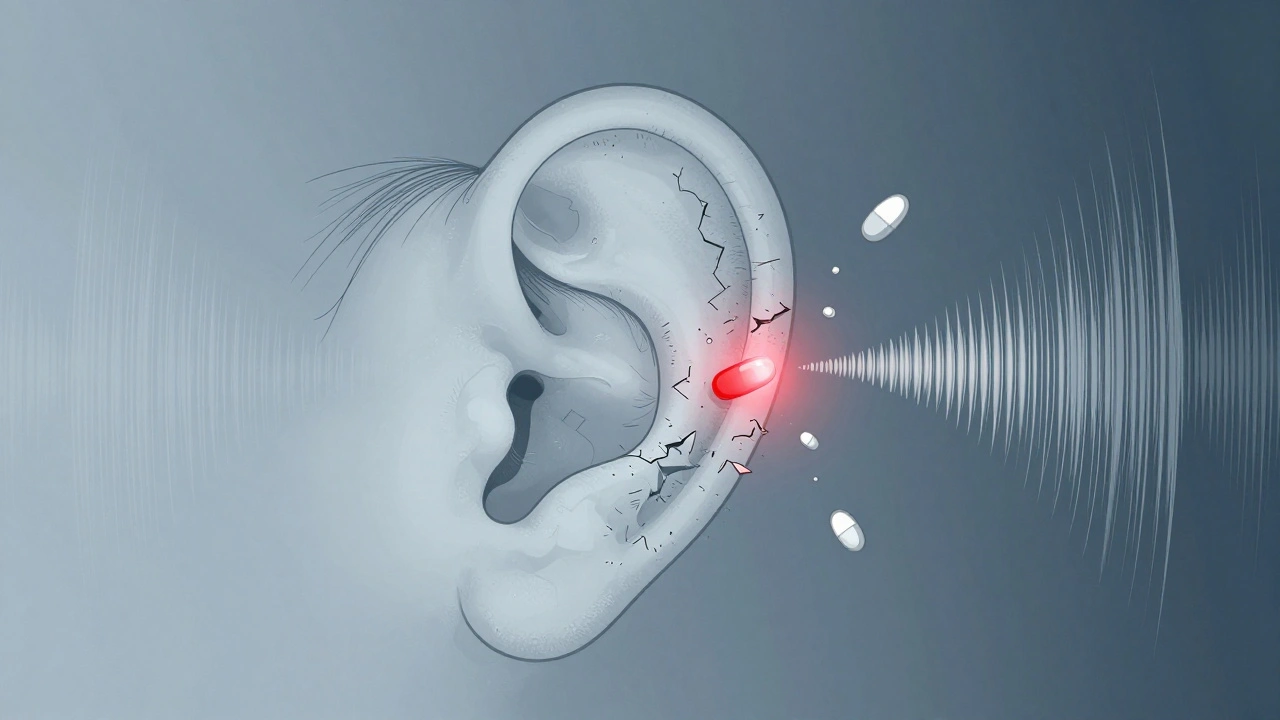
When you take an ototoxic antibiotic, a type of medication that can harm the inner ear and cause hearing loss or balance problems. Also known as ear-damaging antibiotics, these drugs don’t just fight infection—they can quietly wreck the tiny hair cells in your cochlea that turn sound into signals your brain understands. It’s not common, but it’s real—and it doesn’t always show up right away. Some people notice ringing in their ears weeks after finishing a course. Others lose high-pitched sounds first, like birds chirping or children’s voices, and don’t realize it’s the medicine, not aging.
Not all antibiotics are risky, but the big ones to watch for include aminoglycosides, a class of powerful antibiotics used for serious infections like sepsis or pneumonia, often given in hospitals. Examples are gentamicin, tobramycin, and amikacin. They’re effective, but they stick around in your inner ear long after they’ve cleared your bloodstream. Then there’s vancomycin, a last-resort antibiotic for resistant infections like MRSA, often linked to hearing loss when used with other ototoxic drugs. Even high doses of certain macrolides like erythromycin can cause temporary tinnitus or dizziness in sensitive people.
Why does this happen? These drugs build up in the fluid around your inner ear and poison the cells that don’t regenerate. Once they’re gone, they’re gone. Risk goes up if you’re older, have kidney problems, take multiple ototoxic drugs at once, or have a family history of hearing loss. It’s not just about the dose—it’s about how long you’re on it, how fast your body clears it, and whether you’re already dealing with noise exposure or other meds like loop diuretics or chemotherapy drugs.
You won’t always feel it coming. There’s no warning pain. No swelling. Just a slow, silent fade. That’s why doctors monitor hearing during long treatments—especially in ICU patients or those with cystic fibrosis. But if you’re taking one of these at home, pay attention: if your ears start ringing, sounds feel muffled, or you feel unsteady on your feet, don’t wait. Talk to your provider. It might not be the infection returning—it could be the cure.
The posts below dig into real cases and science behind these risks. You’ll find how doctors test for early damage, which antibiotics are safer alternatives, and how to protect your hearing when you have no choice but to use these drugs. Some articles show how drug interactions make the risk worse—like combining vancomycin with NSAIDs or diuretics. Others break down what lab values and hearing tests actually mean. You’ll also see how people manage life after hearing loss from antibiotics, and what’s being done to make these drugs safer.