HIV Protease Inhibitors: How They Stop the Virus and What You Need to Know
When you hear HIV protease inhibitors, a class of antiviral drugs that stop HIV from making new copies of itself by blocking a key enzyme called protease. Also known as PIs, they’ve been a backbone of HIV treatment since the 1990s and still play a vital role today, especially in resource-limited settings. These drugs don’t cure HIV, but they keep the virus under control so the immune system can recover and stay strong.
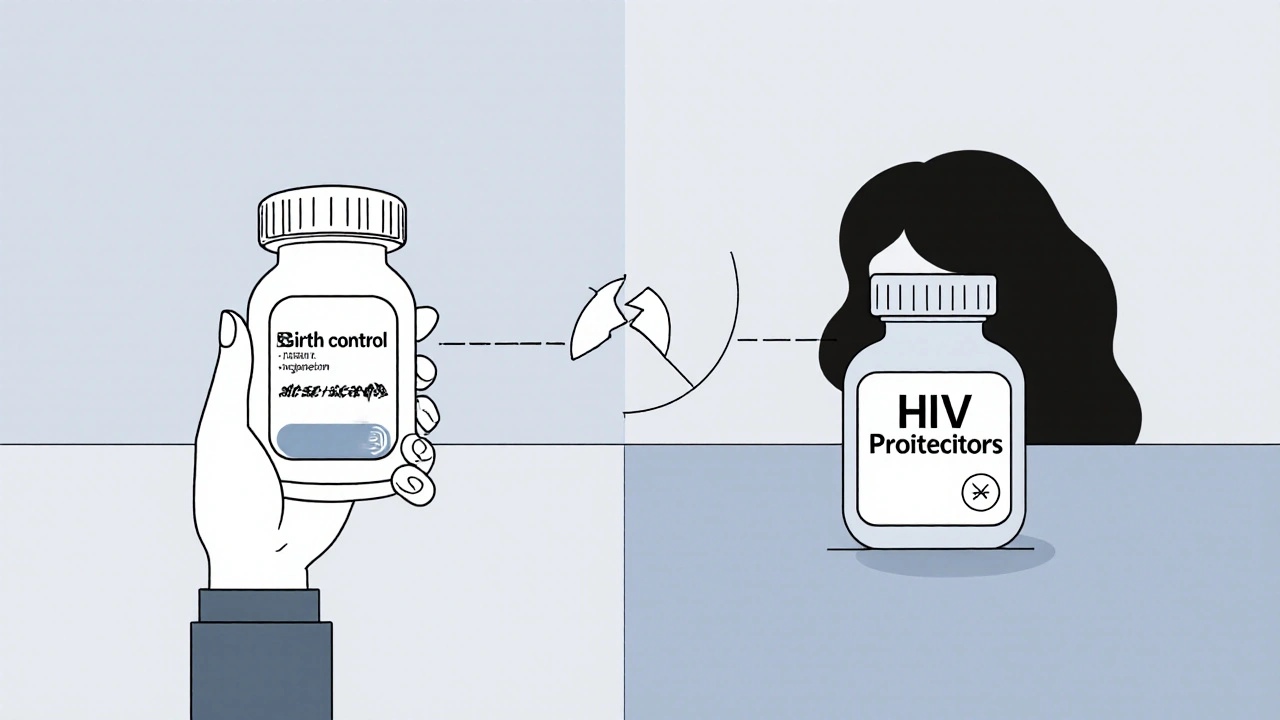
They work by jamming the HIV protease enzyme — the virus’s molecular scissors — so it can’t cut long protein chains into the pieces it needs to build new infectious particles. Without that, the virus can’t mature or spread. But here’s the catch: many HIV protease inhibitors, like lopinavir/ritonavir, a combination where ritonavir boosts lopinavir’s effect by slowing its breakdown in the liver, rely on something called CYP3A4 inhibition. That’s why they cause so many dangerous drug interactions, conflicts with other medications that share the same metabolic pathway. For example, mixing them with certain statins, sedatives, or even some heart meds can lead to overdose or organ damage. That’s why doctors still use them — not because they’re the safest, but because they’re affordable, effective, and work when other options aren’t available.
What you’ll find in this collection isn’t just a list of drug names. It’s a real-world look at how these drugs fit into daily care. You’ll read about how ritonavir boosting shapes outcomes, why some patients still use older PIs despite newer options, and how drug interactions can turn a simple prescription into a life-threatening mix. There’s also coverage on how these treatments connect to broader topics like liver health, medication safety, and the real challenges of managing HIV long-term. Whether you’re someone on treatment, a caregiver, or just trying to understand how HIV meds work, this isn’t theory — it’s what happens in clinics, pharmacies, and homes around the world.