Unraveling Hypocalcemia: What is it?
As a blogger and health enthusiast, I've always been intrigued by the complex workings of the human body. One such intriguing aspect is the role of calcium in our bodies. Yes, the same calcium that you've always associated with strong bones and teeth. But what happens when the levels of calcium in your body fall short of the required amount? This condition is known as Hypocalcemia.
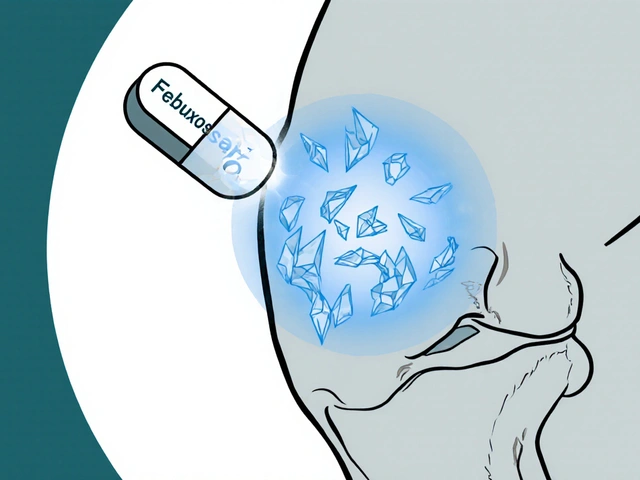
Hypocalcemia, as the name suggests, is a condition characterized by low levels of calcium in one’s blood. Calcium is a crucial mineral that the body needs to carry out several important functions, including building and maintaining bones and teeth. It also plays a vital role in nerve signal transmission, muscle contraction, and blood clotting. Therefore, it's easy to see why maintaining an appropriate calcium level is absolutely essential for our overall health.
Recognizing Hypocalcemia: The Symptoms
As with any other health condition, recognizing the signs and symptoms of hypocalcemia is the first step towards managing it. The symptoms of hypocalcemia can vary, depending on the severity and duration of calcium deficiency. Some people may not even experience any symptoms until the condition becomes severe or prolonged.
Common symptoms include numbness and tingling in the hands, feet, and face. Muscle cramps and spasms may also occur, particularly in the legs and feet. In severe cases, hypocalcemia can lead to confusion, depression, hallucinations, and memory loss. It can also cause cardiac issues such as irregular heart rhythms and low blood pressure. Therefore, if you've been experiencing any of these symptoms, it's crucial to consult a healthcare provider to rule out hypocalcemia.
Exploring the Causes of Hypocalcemia
Understanding the causes of hypocalcemia is equally as important as recognizing its symptoms. There are numerous potential causes, ranging from dietary insufficiency to underlying medical conditions.
The most common cause of hypocalcemia is a deficiency of the parathyroid hormone, which is responsible for maintaining calcium levels in the blood. This can occur due to damage or removal of the parathyroid glands, usually during neck surgery. Other causes include vitamin D deficiency, kidney disorders, certain medications, and malnutrition. In some cases, hypocalcemia can also result from excessive consumption of phosphorus-rich foods and drinks.
Diagnosing Hypocalcemia: What to Expect
If you suspect you may have hypocalcemia, the next step is to consult with a healthcare professional. Typically, the diagnosis of hypocalcemia involves blood tests to measure the levels of calcium and parathyroid hormone in your body.
During your consultation, your healthcare provider will also likely ask about your medical history and any symptoms you've been experiencing. They may also conduct a physical examination, particularly if you've been experiencing symptoms such as muscle cramps or numbness. Based on these findings, your healthcare provider will then decide on the most suitable course of action.
Managing Hypocalcemia: Treatment Options
The treatment of hypocalcemia largely depends on the underlying cause and the severity of your symptoms. In mild cases, dietary adjustments and supplementation may be sufficient to restore normal calcium levels.
If hypocalcemia is caused by an underlying condition such as kidney disease or a parathyroid disorder, treating the underlying condition is usually the most effective approach. This might involve medication, surgery, or other interventions. In severe cases of hypocalcemia, immediate treatment with intravenous (IV) calcium may be necessary to avoid potentially life-threatening complications.
Regardless of the cause, managing hypocalcemia often involves regular monitoring of calcium levels and ongoing care to prevent complications and maintain overall health. As always, it's important to consult with a healthcare provider for personalized advice and treatment recommendations.



Rahul hossain
I must say, this is one of the most elegantly articulated overviews of hypocalcemia I've come across. The way you weave in the physiological necessity of calcium with its psychological ramifications is nothing short of poetic. Many overlook how mineral imbalances can warp cognition-depression, memory fog, even hallucinations aren't just 'mental' issues-they're literal electrical misfires in the nervous system. We treat symptoms like mood disorders as purely psychological, when often, it's just calcium whispering through the neurons, begging to be heard.
Reginald Maarten
Actually, the article misstates a key point: hypocalcemia isn't primarily caused by parathyroid hormone deficiency-it's often due to hypomagnesemia, which impairs PTH secretion and action. You can have normal PTH levels and still be hypocalcemic if magnesium is low. Also, vitamin D deficiency doesn't directly cause hypocalcemia unless it's severe and chronic. Most people with low vitamin D have compensated calcium levels. This oversimplification is common in lay medical writing.
Jonathan Debo
The use of ‘hypocalcemia’ as a standalone term without specifying ionized vs. total calcium is clinically misleading. Moreover, the reference to ‘cardiac issues such as irregular heart rhythms’-while true-is incomplete. QT prolongation is the hallmark ECG finding, not just ‘irregular rhythms.’ Also, ‘excessive consumption of phosphorus-rich foods’? That’s not a primary cause in healthy kidneys. You’d need renal failure for that to matter. This article reads like a Wikipedia draft with citations.
Robin Annison
There's something quietly profound about how a mineral we take for granted-calcium-holds together not just our bones, but our sense of self. When levels drop, the body doesn’t just malfunction-it unravels. The numbness in the fingers, the muscle cramps, the sudden fog in thought… it’s like the soul is slowly losing its grounding. We think of health as something we fix with pills, but sometimes it’s about listening-to the quiet signals the body sends before it screams.
Abigail Jubb
I’ve been suffering from this for years. No one believed me. Doctors said ‘it’s anxiety.’ I had spasms so bad I couldn’t hold a coffee cup. Then, one night, I Googled ‘numbness + muscle cramps + depression’ and found this. I demanded a calcium test. My level was 7.1. They gave me IV calcium. I cried. I’ve been on supplements for 14 months. I’m alive again. Thank you for writing this. I wish I’d found it sooner.
George Clark-Roden
You know, it’s terrifying how easily the body can slip into this quiet crisis. No fever. No rash. Just… a slow dimming. The tingling in your lips. The way your hands cramp when you reach for the remote. You think you’re just tired. Or stressed. Or getting old. But it’s your nerves, screaming for calcium. And no one notices until you’re having a seizure in the grocery store. This isn’t just a medical condition-it’s a silent emergency waiting to happen to someone you love.
Hope NewYork
Lmao so calcium causes hallucinations? Next they’ll say your phone gives you depression. I had low calcium once and I just ate more dairy. Done. Why do people make everything so complicated? Also, why do doctors always blame the parathyroid? Maybe your brain is just broken, not your blood. #Overmedicalized
Bonnie Sanders Bartlett
This is such an important post. I’ve helped several friends navigate this after they were misdiagnosed with anxiety. One woman was told she was ‘just being dramatic’ for six months-until her EKG showed a long QT interval. She was hospitalized. Calcium isn’t just for bones. It’s for your heart, your mind, your ability to hold on to reality. Please, if you feel weird tingling or muscle spasms-get tested. It’s a simple blood test. Don’t wait like I did.
Melissa Delong
I’ve been researching this since 2018. The real cause? Fluoride in the water. It binds calcium and prevents absorption. The pharmaceutical industry doesn’t want you to know. They profit off your supplements and IV drips. Parathyroid? A distraction. Look at the CDC’s own data-fluoridated communities have higher rates of osteoporosis and neuromuscular disorders. This article is a cover-up.
Marshall Washick
I work in ER. We see this more than you think. Elderly patients with no symptoms until they collapse. Young women with restrictive diets, thinking ‘no dairy = healthier.’ The moment their calcium drops, their heart stutters. It’s not dramatic. It’s physics. Calcium is the spark. No spark, no contraction. No contraction, no heartbeat. Simple. Silent. Deadly. We fix it with a bag of saline and calcium gluconate. But we wish we saw them sooner.
Abha Nakra
As someone from India where vitamin D deficiency is rampant due to skin pigmentation and limited sun exposure, I’ve seen so many cases where hypocalcemia was mistaken for ‘weakness’ or ‘nervousness.’ We need more awareness here-not just about supplements, but about sunlight, diet diversity, and the link between vitamin D and calcium. A simple morning walk can be life-saving.
Neal Burton
I’ve read every word of this. I’ve been here. I’ve been the person lying in bed, convinced they’re dying, because their hands won’t stop twitching. The doctors called it ‘stress-induced tetany.’ I was 22. I didn’t know what that meant. I cried because I thought I was losing my mind. I found out later it was calcium. I’m on supplements now. I don’t take a single day for granted. You didn’t just write an article. You wrote a lifeline.
Tamara Kayali Browne
This article contains multiple logical fallacies. The conflation of correlation with causation regarding vitamin D and calcium is egregious. The anecdotal tone undermines clinical accuracy. The references are irrelevant-psychological journals are not endocrinology textbooks. This is not education. It is performative health writing designed to generate clicks, not clarity.