Fungal Pneumonia: Causes, Risks, and How It's Treated
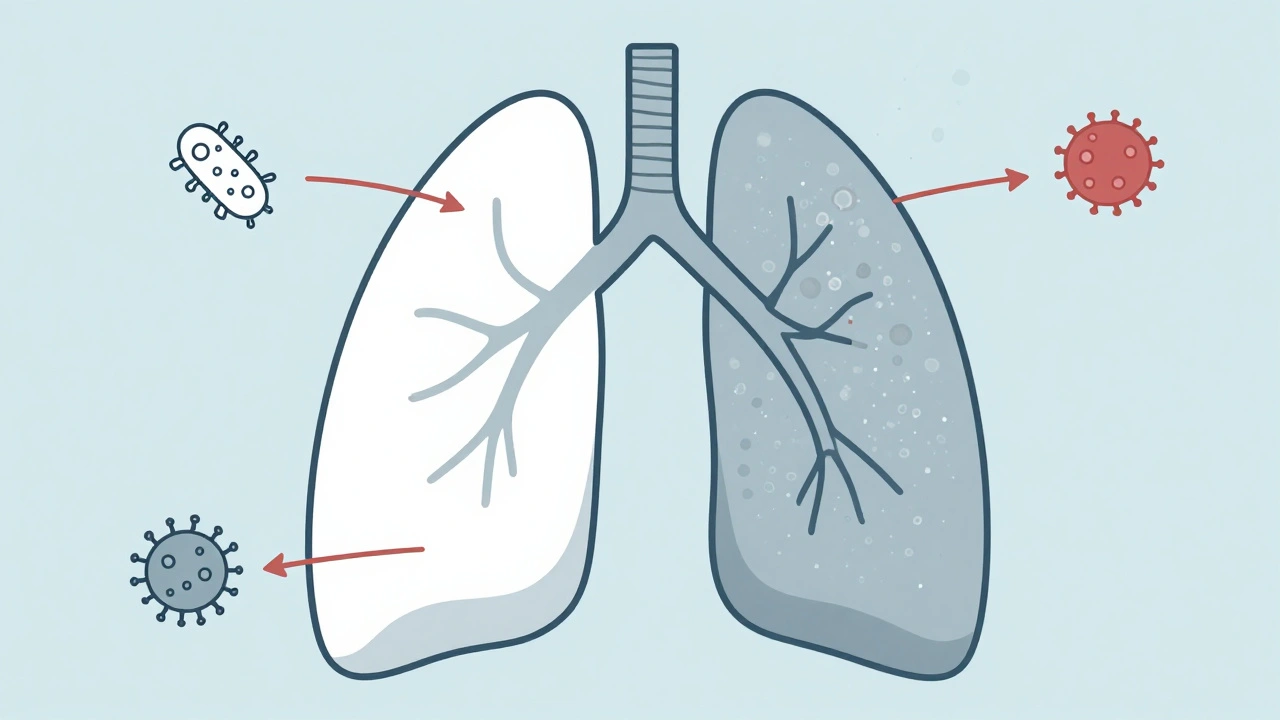
When you hear "pneumonia," you probably think of bacteria or viruses. But fungal pneumonia, a lung infection caused by fungi that enter the lungs through breathing. Also known as fungal lung infection, it’s rare in healthy people but can be life-threatening for those with weakened immune systems. Unlike bacterial pneumonia, it doesn’t spread from person to person. Instead, it comes from breathing in spores from soil, bird droppings, or decaying organic matter—especially in places like the Ohio River Valley or the Southwest U.S.
Fungal pneumonia isn’t one disease—it’s a group of infections. The most common types are caused by Histoplasma, a fungus found in soil enriched with bird or bat droppings, Coccidioides, common in dry, dusty areas like Arizona and California, and Aspergillus, a mold that grows on rotting vegetation and can trigger allergic or invasive reactions. People with HIV, cancer, organ transplants, or long-term steroid use are at highest risk. Even healthy people can get sick after heavy exposure—like construction workers, farmers, or spelunkers.
Treating fungal pneumonia isn’t like treating a cold. Antibiotics won’t touch it. You need antifungal drugs, medications designed to kill or slow down fungi—often taken for weeks or months. Common ones include voriconazole, amphotericin B, and itraconazole. Some patients need IV treatment in the hospital; others can manage with pills at home. The key is catching it early. Symptoms like persistent cough, fever, chest pain, and shortness of breath that don’t improve after a few weeks might be fungal—not just a stubborn cold.
What makes fungal pneumonia tricky is that it often looks like other lung problems on X-rays or CT scans. Doctors rely on lab tests—blood, sputum, or tissue samples—to confirm the fungus. If you’ve been in a high-risk area and have a weakened immune system, don’t ignore lingering respiratory symptoms. Delayed diagnosis can lead to severe complications, including lung damage or spread to other organs.
Below, you’ll find real-world guidance on how these infections are diagnosed, treated, and prevented. You’ll see how drug interactions, immune status, and environmental exposure shape outcomes. Whether you’re managing a chronic condition, caring for someone immunocompromised, or just want to understand why a simple cough won’t go away, these posts give you the facts—not the fluff.