How many ear infections is too many? If your child gets pneumonia twice in a year, is that normal? What about thrush that won’t go away after age one? These aren’t just annoying health bumps-they could be warning signs of something deeper. Recurrent infections aren’t always bad luck or a weak immune system from cold weather. Sometimes, they’re the body screaming that it can’t fight off germs the way it should. And when that happens, waiting it out can cost precious time-and even life.
When Recurrent Infections Aren’t Just Kids Being Kids
It’s normal for young children to get sick. A preschooler might have six to twelve colds, ear infections, or sore throats in a year. That’s part of building immunity. But when infections start hitting the same spots again and again, or get worse instead of better, that’s when you need to look closer.
The red flags aren’t vague. They’re specific. Four ear infections in 12 months? That’s one. Two sinus infections that require antibiotics? Another. Two pneumonias in a year? That’s not normal. And if your child needs IV antibiotics just to clear an infection, or if they’ve been on oral antibiotics for two months with no improvement, that’s a clear signal.
Some signs are harder to miss. Oral thrush after age one? That’s not typical. Fungal infections on the skin that won’t heal? Deep abscesses in organs like the liver or lungs? These aren’t run-of-the-mill bugs. They’re opportunistic invaders that only thrive when the immune system is broken. And if your child isn’t gaining weight or growing properly-despite eating well-that’s a major clue. Failure to thrive in kids with recurrent infections isn’t just a symptom. It’s a diagnostic anchor.
What Doctors Look For Beyond the Infections
Physical exam findings can be just as telling as the infection history. If a child has no tonsils or lymph nodes you can feel, that’s unusual. In severe combined immunodeficiency (SCID), 78% of cases show absent lymphoid tissue. That’s not a coincidence. It means the body’s immune cells aren’t developing properly.
Skin changes matter too. Telangiectasias-those tiny red spider veins on the face or eyes-are found in 95% of kids with ataxia-telangiectasia, a rare but serious PID. Persistent thrush has an 89% specificity for antibody deficiency. That means if a child over one has thrush that won’t clear, there’s a very high chance their body isn’t making the right antibodies to fight fungi.
And then there’s family history. If a sibling died young from an infection, or a cousin had a rare immune disorder, that’s not just background noise. It’s a genetic breadcrumb. One in 1,200 people in the U.S. has a primary immunodeficiency. Many go undiagnosed for years because no one connects the dots.
The First Steps in the Workup: Blood Tests That Matter
Before you jump to expensive genetic tests, start with the basics. A complete blood count (CBC) with manual differential is the first test. In kids over one, a lymphocyte count under 1,500 cells/μL raises a red flag. In babies under a year, anything under 3,000 is suspicious. Low lymphocytes mean T-cells or B-cells aren’t being made-or are being destroyed.
Next, immunoglobulins. IgG, IgA, IgM. These are the antibodies your body uses to neutralize bacteria and viruses. But you can’t just compare a child’s level to an adult’s normal range. A 3-month-old with an IgG of 243 mg/dL is normal. At 6 months, it’s 558 mg/dL. By age five, it hits adult levels: 700-1,600 mg/dL. If an 8-year-old has an IgG of 420 mg/dL, that’s not “just below normal.” That’s severely low for their age. And yet, many doctors miss this because they’re used to seeing adult ranges.
Low IgG alone isn’t enough. You need to know if the body can make antibodies when challenged. That’s where vaccine testing comes in. After giving tetanus and diphtheria vaccines, you wait four to six weeks and check IgG levels again. A protective level for tetanus is 0.1 IU/mL. For pneumococcal polysaccharides, it’s 1.3 μg/mL. If the body doesn’t respond, you’re looking at a functional antibody deficiency-likely Common Variable Immunodeficiency (CVID).
Flow Cytometry and the Hidden Players
Flow cytometry sounds fancy, but it’s just a way to count and sort immune cells. It measures CD3 (T-cells), CD4 (helper T-cells), CD8 (killer T-cells), CD19 (B-cells), and CD56 (NK cells). A CD3 count under 1,000 cells/μL in a child over two years is abnormal. Low CD4? That’s a red flag for HIV or SCID. Low CD19? Could be X-linked agammaglobulinemia, which affects boys almost exclusively.
These numbers aren’t just for diagnosis. They guide treatment. If a child has low B-cells and no antibodies, they’ll need lifelong immunoglobulin replacement. If T-cells are missing, they might need a bone marrow transplant. You don’t treat a low IgG the same way you treat a low CD4 count. Misreading this leads to wrong treatments-and sometimes, dangerous ones.
Don’t Mistake Transient Problems for Permanent Ones
One of the biggest mistakes in primary care? Treating transient hypogammaglobulinemia of infancy (THI) as CVID. THI happens in 2-5% of infants. Their IgG dips low between 3 and 6 months, then climbs back up by age two. It’s temporary. But 41% of pediatricians in one survey started IVIG therapy for these kids anyway. That’s unnecessary, expensive, and carries risks.
How do you tell the difference? Time. And repeat testing. If IgG is low at 8 months but normal at 24 months, it’s THI. If it’s still low at age four, and the child still can’t respond to vaccines, then it’s CVID. Rushing to treatment without confirmation does more harm than good.
What Else Could Be Going On? Ruling Out the Mimics
Not every recurrent infection is immune-related. Up to 43% of cases in kids are caused by anatomical problems. Cystic fibrosis accounts for 12%. Chronic sinusitis from deviated septums or nasal polyps? That’s 31%. Foreign bodies in the airway? They show up in 18% of kids with recurrent pneumonia.
And then there are secondary causes. Autoimmune diseases like lupus can eat away at antibodies. Cancer treatments, especially chemotherapy, suppress immunity. Even long-term steroid use can lower IgG. One study found that 30% of patients diagnosed with CVID actually had another condition causing their low antibodies. That’s why you don’t just treat the number-you investigate the cause.
What Happens If You Wait Too Long?
Delaying diagnosis isn’t just inconvenient. It’s dangerous. In SCID, the survival rate jumps from 69% to 94% if diagnosed before 3.5 months of age. Why? Because before that, the child hasn’t been exposed to enough germs to trigger fatal infections. Once they get a bad virus or bacteria, it’s often too late.
Long-term damage piles up. Repeated pneumonia can scar the lungs. Chronic sinus infections can destroy nasal tissue. Fungal infections can spread to the brain. Growth delays become permanent. And every year without treatment adds to the cost-not just in money, but in quality of life.
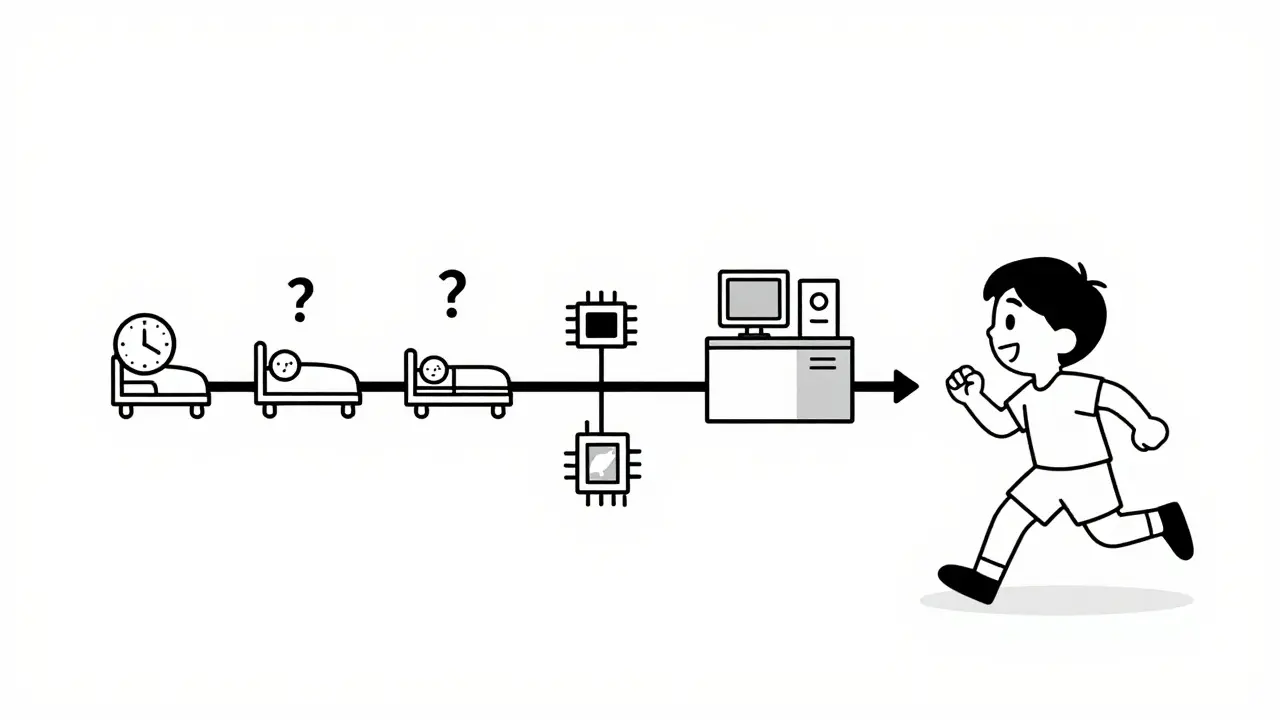
On average, it takes 9.2 years to diagnose a PID in the U.S. That’s nearly a decade of missed school, hospital visits, missed work for parents, and fear. But when clinics use the 10-warning-signs checklist, that drops to 2.1 years. That’s not a small win. That’s life-changing.
The Future Is Faster-and More Accessible
Next-generation gene panels now screen for 484 immune-related genes. They find the cause in 35% of suspected cases-nearly double the old methods. The FDA approved one such test in 2023. It costs $2,450, but it can end a diagnostic odyssey in weeks instead of years.
And it’s not just high-tech solutions. The WHO added lymphocyte flow cytometry to its Essential Diagnostics List for low-resource settings. That means clinics in rural areas or developing countries will soon have access to basic immune testing. New point-of-care tools are in development by PATH and the Gates Foundation-tools that could one day give a result from a single drop of blood.
Within five years, whole exome sequencing may become the first test for suspected immunodeficiency in developed nations. Imagine: a baby gets sick, a blood test runs, and within days, you know if it’s SCID, CVID, or something else. No more guessing. No more delays.
What You Can Do Now
If you’re a parent and your child has multiple red flags, don’t wait. Ask your doctor: “Could this be an immunodeficiency?” Request a CBC, immunoglobulins, and a referral to an immunologist. Don’t accept “they’re just getting sick” as an answer.
If you’re a clinician, learn the 10 warning signs. Know the age-adjusted IgG ranges. Don’t treat low IgG without checking vaccine response. And if you’re unsure-refer. You don’t need to be an immunologist to recognize the signs. You just need to know when to look.
Recurrent infections aren’t always just infections. Sometimes, they’re the first symptom of a hidden problem. And catching it early? That’s the difference between a child who grows up healthy-and one who never gets the chance.





Emma Hooper
Okay but let’s be real - if your kid gets thrush after age one, you’re not just dealing with a bad diaper change. That’s not ‘oh they ate too much sugar’ - that’s your immune system waving a white flag. I had a cousin who got diagnosed with CVID at 7 after years of ‘just a stubborn cold.’ Now she’s on monthly IVIG and can’t go to birthday parties without planning for a hospital trip. It’s not dramatic. It’s life.
Bennett Ryynanen
My daughter had 5 ear infections in 8 months. Pediatrician said ‘they grow out of it.’ I said ‘nope, I’m calling an immunologist.’ Turned out her IgG was half what it should’ve been. They put her on antibiotics for 6 months before even testing. That’s malpractice. Don’t wait. Demand the CBC and IgG. No excuses.
Deepika D
As a pediatric nurse in Mumbai, I’ve seen this too many times. Parents think fever + cough = flu. But when a child has recurrent fungal skin infections, abscesses, or fails to gain weight despite eating like a horse - that’s not nutrition. That’s immunity screaming. We don’t have flow cytometry in every clinic here, but we do CBC and IgG. If lymphocytes are low and IgG is below age-adjusted norms? Refer. Always. Even if you’re in a rural clinic. You don’t need a fancy lab to save a life - just the will to ask the right questions.
And yes, THI gets misdiagnosed as CVID ALL THE TIME. I’ve seen kids get IVIG for 18 months only to find out their IgG normalized at age 2. It’s heartbreaking. Test. Wait. Re-test. Don’t rush to treatment. Let time be your ally.
Chandreson Chandreas
Man… I remember my little brother. Always sick. No tonsils. Always thrush. We thought he was just ‘fragile.’ Turned out he had SCID. Got diagnosed at 14 months. Got the transplant at 16. Now he’s 22 and plays soccer. 🙏
But if we’d waited another 6 months? He wouldn’t be here. This post? It’s a lifeline. Share it. With every mom, every uncle, every grandma who says ‘kids get sick, it’s normal.’ It’s not always normal.
Frank SSS
Look, I get it. Doctors are busy. But this isn’t ‘maybe it’s allergies.’ This is ‘your child’s immune system is basically offline.’ And yet, 9 years to diagnose? That’s not a system failure - that’s a cultural failure. We treat symptoms like they’re the problem. But when infections keep coming back like a broken record? The record player’s broken. Not the song.
I’ve seen parents get gaslit for years. ‘It’s just daycare.’ ‘You’re overreacting.’ ‘He’ll grow out of it.’ Bullshit. If your kid needs IV antibiotics to clear a sinus infection? That’s not a cold. That’s a red alert. And if your doctor doesn’t know that? Find a new one.
Lawver Stanton
Okay, so let me get this straight - if your kid gets pneumonia twice, you’re supposed to panic and run to a specialist? What about all the kids who get sick because they’re around other sick kids? Daycare? School? Public transit? You’re telling me every kid with two pneumonias has a genetic disorder? That’s absurd. And don’t even get me started on IgG levels - kids aren’t little adults. You can’t just plug numbers into a spreadsheet and call it science. This whole thing feels like overdiagnosis dressed up as ‘awareness.’
I’m not saying immunodeficiencies don’t exist. But 1 in 1,200? That’s 270,000 kids in the US alone. Do you really think that many are walking around undiagnosed? Or is this just a way to sell more tests, more IVIG, more genetic panels? I’ve seen too many parents get scared into spending thousands on tests that lead nowhere. Sometimes, kids just get sick. And sometimes, that’s okay.
And what about the kids who get IVIG for THI? Yeah, it’s expensive. But it’s also safe. Why risk a child getting sepsis just to ‘wait and see’? You’re playing Russian roulette with a 6-month-old’s life. I’d rather be overcautious than underprepared. You want to save money? Then stop treating every kid like a lab rat.
And don’t even get me started on ‘flow cytometry.’ That’s a $500 test. In a country where half the population can’t afford a $20 co-pay, you’re telling parents to get this done? That’s not medicine. That’s elitism with a stethoscope.
I’m not denying that some kids have real immune problems. But this post reads like a pharmaceutical ad. ‘Here’s 10 signs you’re a walking medical mystery!’ No. Some kids are just unlucky. And that’s okay. Not every infection is a red flag. Sometimes, it’s just life.
Urvi Patel
So if your kid gets thrush after one you’re supposed to assume it’s immunodeficiency? What about kids in India who eat dirt and drink unfiltered water? Thrush is common there. It’s not a genetic disorder it’s hygiene. You westerners think every problem needs a gene test. We fix things with clean water and soap. Not expensive labs. This is cultural arrogance wrapped in science
anggit marga
Why is every article about kids getting sick just about the US? In Nigeria we have kids who get pneumonia every season because they sleep on concrete floors and their mothers have no access to antibiotics. You think they’re gonna get flow cytometry? You think they care about IgG levels? This is rich people medicine. Meanwhile, millions of kids die from preventable infections because the system doesn’t care. Stop pretending this is about science. It’s about privilege
Joy Nickles
Ugh. I just read this whole thing and now I’m crying. My son had 7 ear infections by age 2. They told me to wait. I didn’t. I demanded the CBC. IgG was 380. They laughed. I cried. I went to a different doctor. He said ‘you’re right. This isn’t normal.’ We found out he had CVID. Now he’s on IVIG every 3 weeks. I’m so mad at the first doctor. I’m so proud of myself for pushing. But why did it take 18 months? Why didn’t they know? I feel like I had to fight for my kid’s life. And I’m not even a doctor. I’m just a mom.
Marilyn Ferrera
One sentence: If your child needs IV antibiotics to clear an infection, you’re not being paranoid - you’re a good parent.
Harriet Hollingsworth
It’s so frustrating how doctors dismiss parents. ‘They’re just getting sick.’ Like it’s a character flaw. My daughter had fungal infections on her scalp for 10 months. Pediatrician said ‘maybe she’s just sweaty.’ I looked it up. Fungal infections in toddlers? Not normal. Took me 6 months to get a referral. When we finally got to the immunologist? She had CVID. And now? She’s thriving. But I had to become a medical detective because no one else would. Don’t let anyone make you feel crazy for asking. You’re not crazy. You’re the only one who knows your child.
Martin Viau
Let’s be precise: the 10 warning signs are evidence-based, validated by the Jeffrey Modell Foundation, and endorsed by AAAAI and WAO. The median diagnostic delay for CVID is 9.2 years - that’s not anecdotal, it’s from the 2019 USIDNET registry. And yes, IgG thresholds are age-adjusted - the 2023 JACI guidelines explicitly state that pediatric norms differ from adult values. The notion that this is ‘overdiagnosis’ ignores decades of peer-reviewed literature. If you’re skeptical, read the 2021 Lancet review on PID diagnostics. But don’t confuse your ignorance with scientific rigor.
Darren Pearson
While the clinical utility of the 10 warning signs is well-documented, one must acknowledge the inherent limitations of population-based thresholds. The age-adjusted IgG norms, for instance, are derived from cross-sectional cohorts that may not account for socioeconomic confounders such as nutritional status or environmental pathogen load. Furthermore, the reliance on flow cytometry and vaccine response testing presupposes a level of healthcare infrastructure that is neither globally equitable nor universally accessible. To assert that early diagnosis is universally achievable without addressing systemic disparities in diagnostic access is, frankly, ethically problematic.
Kayla Kliphardt
I’m a nurse in rural Ohio. We don’t have immunologists nearby. But we do have CBC machines. I’ve started asking parents: ‘Has your child ever needed IV antibiotics?’ ‘Any thrush after age one?’ ‘Any family history of early death from infection?’ If they say yes, I order the IgG and refer. I don’t wait for a specialist to tell me what to do. I just do it. Because I’ve seen what happens when you wait. And I won’t let another kid be another statistic.
Lawver Stanton
Wow. I just read your comment, Joy. And I’m sorry you went through that. I was the one who laughed at you. I thought you were overreacting. I was wrong. I’m not proud of it. I’m going to go back to my clinic tomorrow and update our screening protocol. No more ‘wait and see.’ No more dismissing parents. I’m going to start asking the 10 questions - even if the parent doesn’t bring it up. You saved your kid. Now I’ll try to save others. Thank you.