When your heart arteries are clogged, two main options exist: PCI and CABG. One is a quick procedure through a wrist artery. The other is open-heart surgery. Choosing between them isn’t about which is better overall-it’s about which is better for you.
Percutaneous Coronary Intervention (PCI), commonly called angioplasty with stenting, is a minimally invasive way to open blocked coronary arteries. A thin tube is threaded through an artery in your wrist or groin, guided to the blockage, and a tiny balloon is inflated to widen it. Then, a metal mesh stent-usually coated with medicine-is left in place to keep the artery open. Most people go home the next day. Recovery is fast. You’re back to light activities in days.
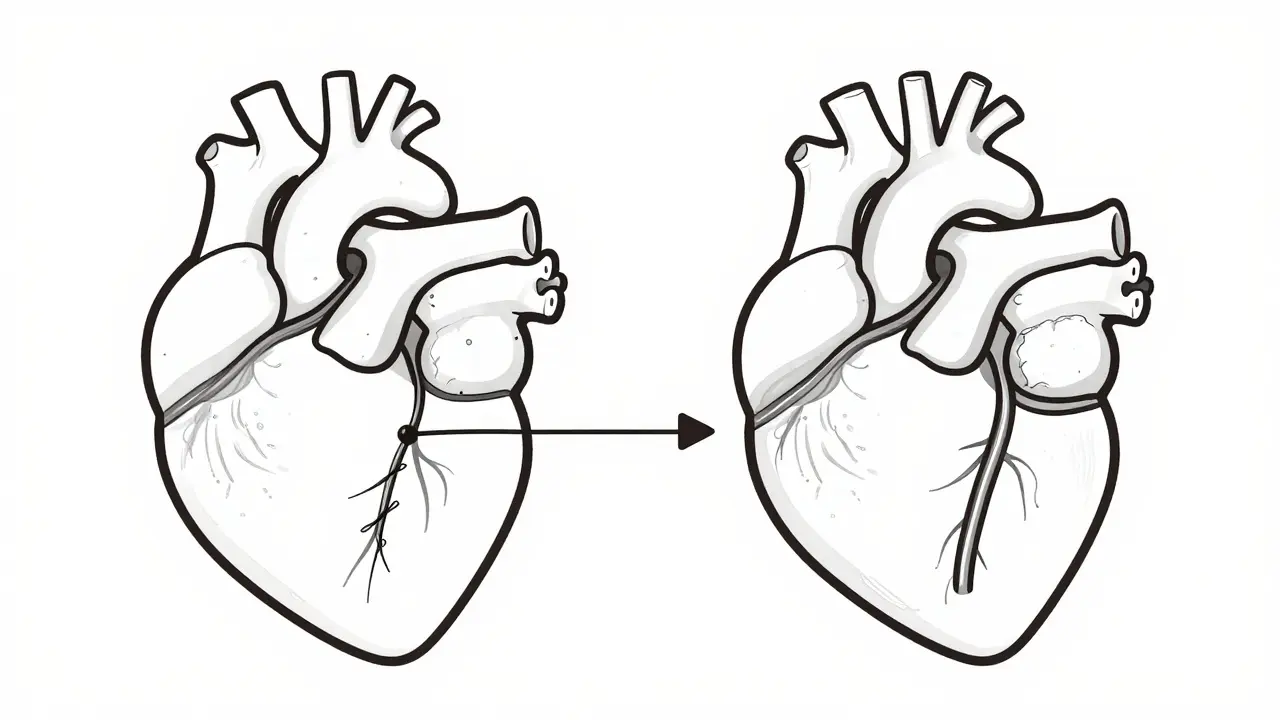
Coronary Artery Bypass Grafting (CABG), or bypass surgery, is different. It’s open-heart surgery. The surgeon takes a healthy blood vessel-often from your chest, leg, or arm-and uses it to create a detour around the blocked artery. Your heart is temporarily stopped, and a machine keeps your blood flowing. Recovery takes weeks. You’ll feel sore for months. But the results last longer.
Both procedures relieve chest pain and improve quality of life. But only one has been shown to help certain people live longer.
How doctors decide: It’s not just about the blockage
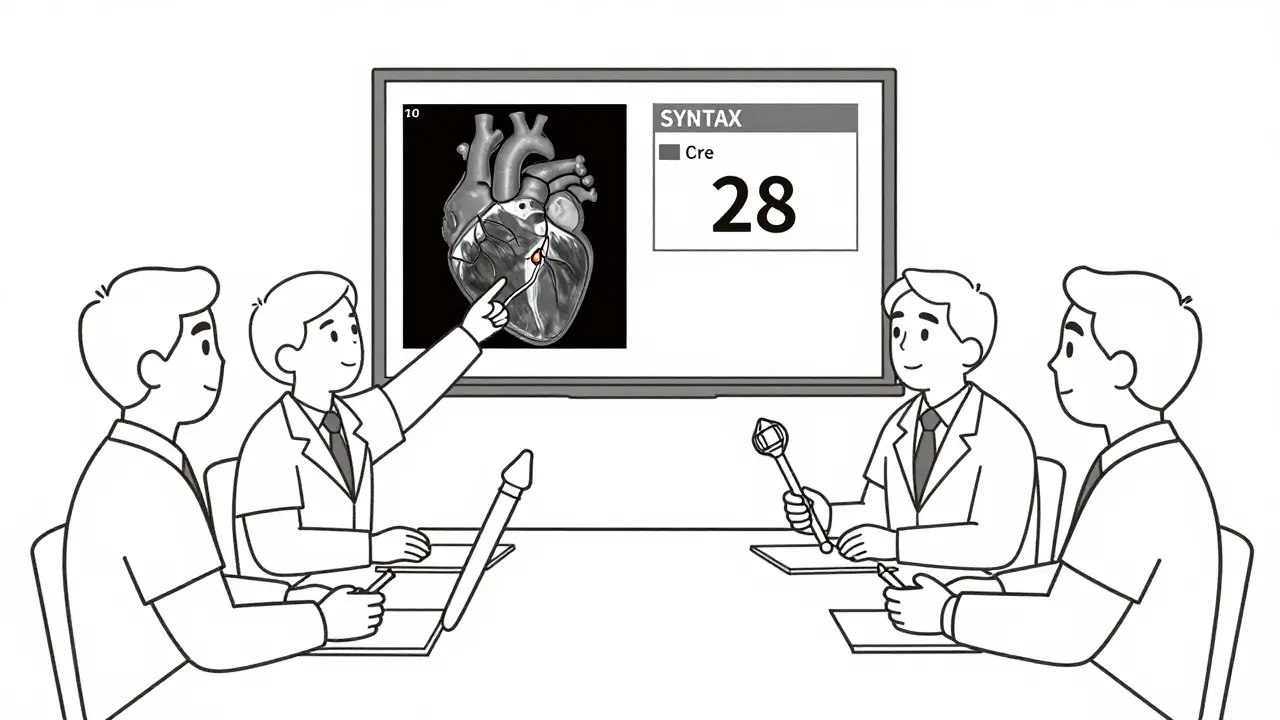
Doctors don’t pick PCI or CABG based on gut feeling. They use tools, data, and guidelines. The most important tool is the SYNTAX score. It measures how complex your artery disease is by looking at the number, location, and severity of blockages on an angiogram.
If your SYNTAX score is below 22-meaning your blockages are simple-you’re likely a good candidate for PCI. If it’s above 32-meaning your arteries are severely damaged-you’re much better off with CABG. Scores between 22 and 32? That’s where things get personal.
But the score isn’t everything. Diabetes changes everything. If you have diabetes and multiple blocked arteries, especially if the main left artery is involved, CABG cuts your risk of dying by nearly half compared to PCI. The FREEDOM trial showed this clearly: 16.4% of diabetic patients who got PCI died within five years. Only 10% of those who had CABG did.
Left main disease is another key factor. If the main artery feeding your heart is narrowed, CABG has a long-term survival edge. The EXCEL trial found that while PCI and CABG had similar results in the first three years, after five years, CABG patients were 61% less likely to have a heart attack or need another procedure.
Even your heart’s pumping strength matters. If your left ventricle is weak, CABG gives better long-term outcomes. Your age, kidney function, and other health problems also play a role.
What happens during each procedure
PCI is done in a cath lab. You’re awake but sedated. The doctor accesses your artery through your wrist (radial approach) or groin (femoral). A tiny balloon is inflated at the blockage, then a stent is placed. The whole thing takes one to two hours. You’re usually home the next morning. Side effects? Minor bruising, rare bleeding. The big risk? The artery re-narrows. But modern drug-coated stents have cut that risk to 5-10% over five years.
CABG is done in an operating room. You’re under general anesthesia. The surgeon makes a cut down your chest, opens your ribcage, and connects you to a heart-lung machine. Then, they harvest a blood vessel-most often from your chest wall-and sew it onto your coronary artery, bypassing the blockage. The surgery takes three to six hours. You’ll stay in the hospital for five to seven days. Recovery takes six to eight weeks. You’ll have a long scar. Your chest will ache. You might feel foggy for a few weeks.
Some surgeons now do off-pump CABG-keeping your heart beating during surgery. Others use robotic assistance. But even with these advances, it’s still major surgery.
Long-term results: Which lasts longer?
PCI’s biggest weakness is durability. Stents work well for years, but they can’t match the longevity of a bypass graft. Arterial grafts-especially the one taken from your chest wall-stay open over 90% of the time after ten years. Vein grafts, often taken from your leg, have a higher failure rate-about 40% close within ten years.
PCI has a much higher chance of needing another procedure. The SYNTAX trial found that 16% of PCI patients needed another revascularization within five years. Only 7% of CABG patients did. The NOBLE trial showed similar results: 16% of PCI patients needed repeat procedures. Only 3% of CABG patients did.
But CABG has its own trade-off: stroke risk. During CABG, clots can break loose and travel to the brain. About 1.7% of CABG patients have a stroke within 30 days. For PCI, it’s just 1%. That’s why PCI is often preferred for older patients or those with high stroke risk.
Meta-analyses of over 11,000 patients show CABG reduces heart attacks and repeat procedures significantly. But it increases stroke risk slightly. The net result? A 2% absolute survival advantage for CABG at five years. That might sound small, but in heart disease, even 2% matters.
Quality of life: Fast recovery vs lasting relief
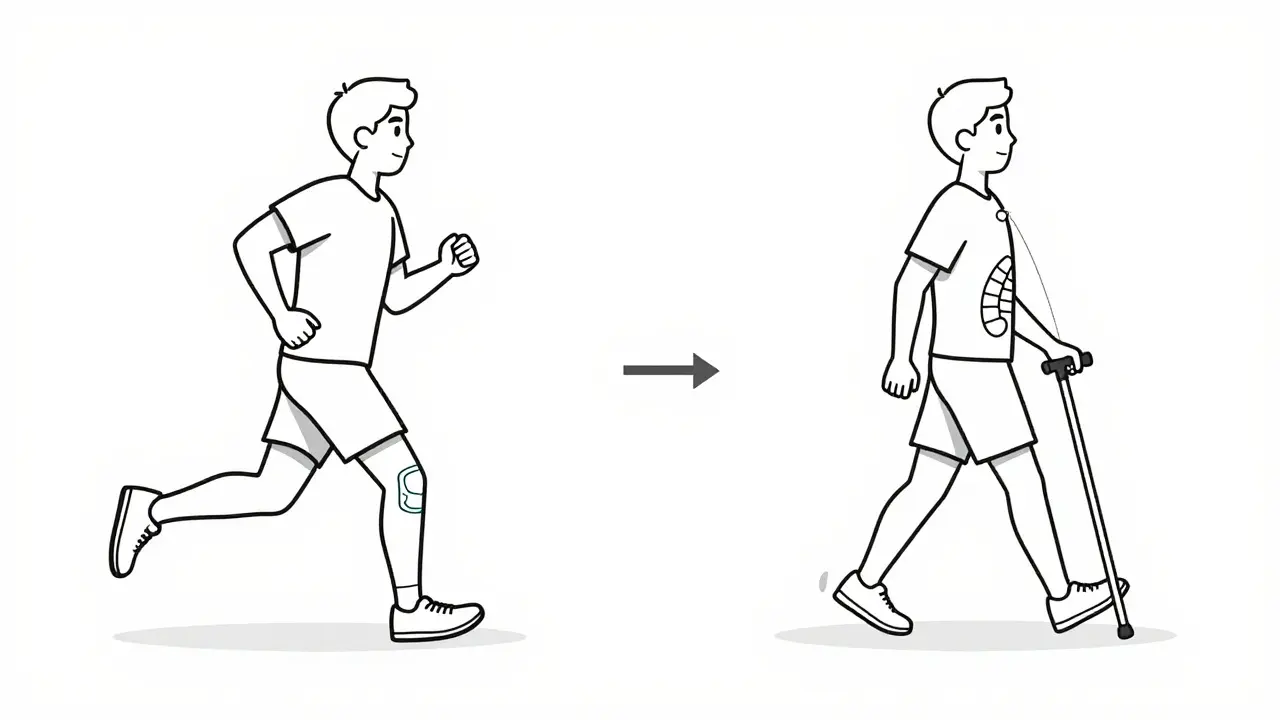
Right after the procedure, PCI wins. At 30 days, 78% of PCI patients say they’re back to normal daily life. Only 52% of CABG patients can say the same. Many return to work in under two weeks.
But over time, CABG often wins. At one year, 92% of CABG patients report complete relief from chest pain. Only 85% of PCI patients do. The ROSETTA trial found CABG patients had better quality-of-life scores, even if their recovery was slower.
Many people who get stents come back with the same chest pain months later. They need another stent. Or two. One Reddit user wrote: "Back to work in 3 days. Needed another stent after 18 months." That’s not rare. About 15-20% of PCI patients need repeat procedures within five years.
CABG patients often deal with chest pain from the incision. About 45% feel it at three months. But by a year, that drops to 12%. Some report memory issues or brain fog after surgery-about 18% at six weeks. Most of those improve within a year.
Who should get what? Real-world decision rules
Here’s how most heart teams decide today:
- Choose PCI if: You have simple blockages (SYNTAX score <22), are not diabetic, have single-vessel disease, or are too high-risk for surgery. You want the fastest recovery and are okay with possible repeat procedures.
- Choose CABG if: You have diabetes and multivessel disease, left main disease with SYNTAX score >32, poor heart function, or complex blockages. You’re willing to endure a longer recovery for a better long-term outcome.
- Consider both if: Your SYNTAX score is between 22 and 32. Your age, lifestyle, and preferences matter more here. Talk to both your cardiologist and cardiac surgeon.
There’s one more rule: the heart team. Guidelines require that decisions be made by a group-cardiologist, cardiac surgeon, and sometimes a nurse or anesthesiologist. This isn’t bureaucracy. It’s safety. A cardiologist might lean toward PCI. A surgeon might lean toward CABG. Together, they weigh the data, your health, and your goals.
What’s changing? New tech and future trends
PCI technology keeps improving. New stents are thinner, more flexible, and coated with better drugs. Bioresorbable scaffolds-stents that dissolve over time-are being tested again after earlier failures. They might one day offer the benefits of stenting without the long-term metal risk.
CABG is also evolving. Surgeons are using more arterial grafts-not just one, but two or even three. Early data shows this can boost 10-year survival to 82%. Robotic-assisted CABG is becoming more common, reducing incision size and recovery time.
Hybrid procedures are on the horizon. Imagine getting a minimally invasive CABG to bypass your main artery, then a stent for other blockages. That’s already happening in top centers. Experts predict it could become standard in five to seven years.
But here’s the reality: no matter how advanced the tech gets, the best choice still depends on your body, your health, and your goals. The number of PCI procedures keeps rising-600,000 a year in the U.S. But CABG isn’t disappearing. It’s stabilizing. About 300,000 are done yearly. Why? Because for the right patient, it still saves lives.
What to ask your doctor
Don’t just accept a recommendation. Ask these questions:
- What’s my SYNTAX score? Can you show me the angiogram?
- Am I diabetic? Does that change the recommendation?
- What’s the chance I’ll need another procedure in five years?
- What’s my stroke risk with each option?
- Will you be using an arterial graft? How many?
- Can I meet with both the cardiologist and surgeon together?
If your doctor won’t involve both specialists-or won’t explain your SYNTAX score-get a second opinion. This isn’t a decision to rush.
Bottom line: No one-size-fits-all
PCI is faster. CABG lasts longer. PCI has lower short-term risk. CABG has lower long-term risk for certain people. Neither is "better." The best choice is the one matched to your anatomy, your health, and your life.
For many, PCI is perfect. For others-especially those with diabetes, complex blockages, or left main disease-CABG isn’t just an option. It’s the smarter, longer-lasting choice. The data doesn’t lie. But only you and your heart team can decide what’s right for you.
Is PCI better than CABG for everyone?
No. PCI is less invasive and has a faster recovery, but it doesn’t offer the same long-term survival benefits as CABG for certain patients. People with diabetes, multivessel disease, or complex blockages (SYNTAX score >32) live longer with CABG. PCI is best for simpler cases or patients who can’t tolerate surgery.
How long do stents last compared to bypass grafts?
Stents last well for five to ten years, but about 5-10% of them re-narrow over that time. Arterial bypass grafts-especially from the chest wall-stay open in 85-90% of cases after ten years. Vein grafts from the leg have a higher failure rate, with about 40% closing by the ten-year mark.
Why is CABG recommended for diabetics?
Diabetics have more diffuse, complex artery disease. The FREEDOM trial showed that after five years, 16.4% of diabetics who had PCI died, compared to only 10% who had CABG. CABG also reduces the chance of heart attack and repeat procedures in this group, making it the preferred option.
Can I have a heart attack after CABG or PCI?
Yes, but the risk is lower after either procedure than before. CABG reduces the risk of future heart attacks more than PCI, especially in complex cases. The meta-analysis by Palmerini et al. showed a 33% lower risk of heart attack with CABG over five years.
What’s the recovery time difference?
After PCI, most people return to normal activities in 3-7 days. After CABG, it takes 6-8 weeks to fully recover. You’ll need help at home for the first few weeks. Driving is restricted for 4-6 weeks. Returning to work depends on your job-desk jobs may allow 4-6 weeks, physical jobs may take 3 months.
Does CABG cause memory problems?
Some patients report brain fog or memory issues after CABG, especially in the first few weeks. Studies show about 18% experience this at six weeks, but it drops to 5% by one year. It’s likely due to tiny clots or inflammation during surgery. Most people recover fully. PCI has almost no risk of this.
Is a heart team really necessary?
Yes. Guidelines require it. A cardiologist sees the blockages. A surgeon sees the surgical risks. Together, they weigh your age, diabetes, kidney function, and overall health. Studies show heart teams reduce unnecessary procedures and improve outcomes. If your doctor doesn’t offer a team meeting, ask for one.
What if I’m too old for surgery?
Age alone doesn’t rule out CABG. Many patients in their 80s do well with it. But if you have severe lung disease, frailty, or other high-risk conditions, PCI may be safer. Your doctor will assess your biological age-not just your calendar age-using tests like exercise tolerance and muscle strength.



Bret Freeman
This post is basically a sales pitch for CABG disguised as neutral advice. PCI is perfect for most people. Why risk open-heart surgery for a few percentage points? The data cherry-picks high-risk cases to scare people into the operating room. I've seen too many patients get CABG and regret it for years. Just because you're diabetic doesn't mean you need your chest cracked open.
Lindsey Kidd
I'm so glad this post exists 🙏 My dad had CABG last year and honestly? He's a different person now. No chest pain, sleeping through the night, even started gardening again. Yeah, recovery was brutal - 6 weeks of crying in the shower, forgetting his keys, that weird brain fog - but it was worth it. For him, it wasn't just about living longer. It was about living well. If you're on the fence, talk to someone who's been through it. Not just a doctor.
Austin LeBlanc
You people are so naive. PCI is a money grab. Hospitals make way more off stents. The drug companies fund the studies. The SYNTAX score? A marketing tool. I know a cardiologist who admitted to pushing PCI on patients who clearly needed CABG because the hospital gets paid $20K more per procedure. Don't trust the system. Get a second opinion - from someone who doesn't work at a hospital.
niharika hardikar
The clinical evidence is unequivocal. In patients with multivessel coronary artery disease and concomitant diabetes mellitus, coronary artery bypass grafting confers a statistically significant survival advantage over percutaneous coronary intervention, as demonstrated by the FREEDOM trial (HR 0.61, 95% CI 0.45–0.83). Furthermore, the NOBLE trial corroborates lower rates of major adverse cardiac events at five-year follow-up. The decision-making framework must be evidence-based, not anecdotal.
Andrea Di Candia
I think what’s missing here is the human side. It’s not just about SYNTAX scores and survival stats. It’s about who you are - your job, your family, your fear of surgery, your tolerance for pain, your belief in medicine. My uncle got PCI because he was a truck driver and couldn’t afford to be out for months. My aunt got CABG because she wanted to see her grandkids graduate. Neither was ‘right’ or ‘wrong.’ They were right for them. Medicine should help you choose, not dictate.
Dan Gaytan
This is such a good breakdown. I’m a nurse and I see this decision every day. The thing no one talks about? The emotional toll of waiting. People stress over whether they’re ‘worthy’ of CABG or ‘too weak’ for it. It’s not about being brave or lazy - it’s about matching the tool to the problem. If you’re scared, ask for time. Talk to a survivor. Don’t rush. You’ve got this.
Raja P
I'm from India and we don't have the same access to heart teams here. My brother got PCI because that's all the hospital could afford. Two years later, he needed another. I wish we had the same options. This info is gold. Sharing it with my family.
Abby Polhill
CABG feels like something from the 90s. I get why it works, but the idea of cutting open your chest in 2025? Wild. I’m waiting for the day we can just inject nanobots to clear the plaque. Until then, I’ll stick with PCI. My dad’s scar still gives me nightmares.
Bartholomew Henry Allen
American healthcare is broken. CABG should be free for all citizens. PCI is a profit scheme. We are the most advanced nation on earth yet we let corporations decide who lives and who dies based on insurance tiers. Shameful. Fix the system before you lecture patients on SYNTAX scores.
Harsh Khandelwal
They don't want you to know this but stents are made with Chinese steel coated in corporate poison. CABG is the real deal - but only if you get the surgeon who doesn't take bribes from Medtronic. I heard a guy in Mumbai got his graft from a goat vein. No joke. Google it. The system is rigged.
Andy Grace
I had a stent last year. Fast recovery, back to surfing in a week. No regrets. But I know a mate who had CABG after a heart attack and he says it saved his life. Different strokes. Just wish we had more data on long-term mental health outcomes. The brain fog thing worries me.
Delilah Rose
I think the real issue isn’t PCI vs CABG - it’s that we don’t talk enough about prevention. Why are we waiting until someone’s arteries are 90% blocked before we say something? Why aren’t we pushing plant-based diets, stress reduction, and daily movement as the first line of defense? Both procedures are band-aids on a wound caused by decades of processed food, sitting all day, and ignoring our bodies. I’m not saying don’t do the surgery - I’m saying let’s stop pretending this is just a mechanical problem. It’s a cultural one. We treat the heart like a car engine instead of a living organ that needs love, not just metal.
Spencer Garcia
SYNTAX score + diabetes = CABG. Simple. If you’re unsure, get a second opinion from a surgeon who doesn’t do stents. No drama. Just facts.