Chronic pain doesn’t just hurt-it steals your life. You can’t sleep, walk, work, or even hug your kids without flinching. Medications stop working. Injections give temporary relief. Surgery feels too risky. That’s where spinal cord stimulation comes in-not as a cure, but as a way to take back control when everything else has failed.
What Is Spinal Cord Stimulation?
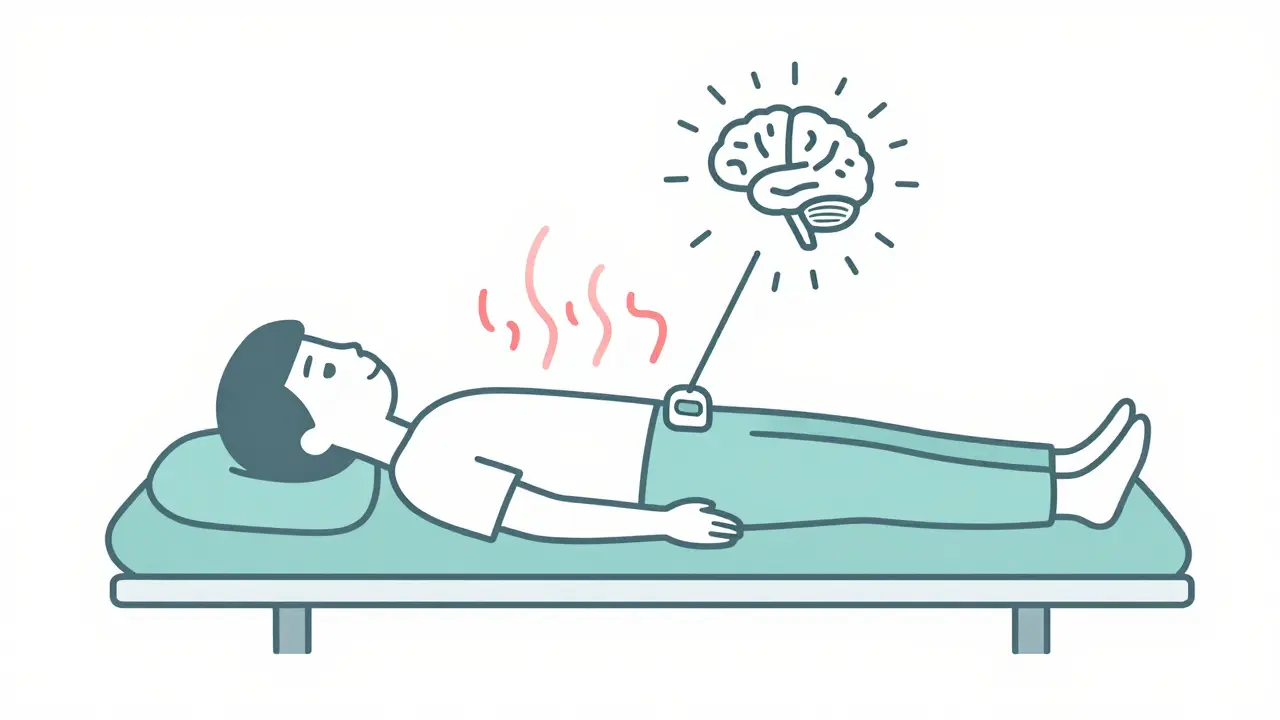
Spinal cord stimulation (SCS) is a medical device implanted under the skin that sends mild electrical pulses to your spinal cord. These pulses don’t fix the source of your pain-they interrupt the pain signals before they reach your brain. Think of it like a noise-canceling headset for your nerves. Instead of screaming "I’m in pain!" to your brain, the signal gets softened, turned into a tingling sensation, or sometimes, silenced entirely.
This isn’t new. The first SCS device was implanted in 1967 by Dr. C. Norman Shealy. Back then, it was crude. Today’s systems are smart, rechargeable, and customizable. Modern devices like Boston Scientific’s WaveWriter Alpha™ Prime, Medtronic’s Intellis™, and Abbott’s Proclaim™ let you choose between different waveforms: traditional tingling-based stimulation, high-frequency pulses that work without any tingling, or burst patterns that mimic how your nerves naturally fire.
Most systems use constant current delivery, which keeps the pulse steady even if your body’s resistance changes. About 68% of patients in one Mayo Clinic study said they preferred this over constant voltage because it felt more natural and gave better relief.
Who Is a Good Candidate for SCS?
Not everyone with chronic pain is a candidate. SCS isn’t for backaches from lifting too much or sore knees from arthritis. It’s for specific, stubborn nerve-related pain that hasn’t responded to anything else.
The best candidates typically:
- Have had chronic pain for 12 to 24 months
- Have tried physical therapy, medications, injections, and maybe even surgery-with little or no lasting relief
- Have a clear diagnosis like failed back surgery syndrome, complex regional pain syndrome (CRPS), or persistent leg pain after spine surgery
- Can pass a trial stimulation (more on that below)
- Are mentally and emotionally ready to manage a device
Psychological health matters as much as physical health. Studies show patients with untreated depression have a 35% lower chance of success. If you’re struggling with anxiety, trauma, or mood disorders, those need to be addressed before implant. It’s not about being "strong enough"-it’s about making sure your brain is in a position to respond to the therapy.
Also, you need to be able to operate the device. That means understanding how to turn it on/off, adjust settings, and recognize when something’s wrong-like if the stimulation suddenly stops or shifts location. About 22% of SCS failures are due to patients not using the device properly.
How the Trial Works
Before you commit to a permanent implant, you get a trial. This is non-negotiable. No reputable doctor will implant a device without one.
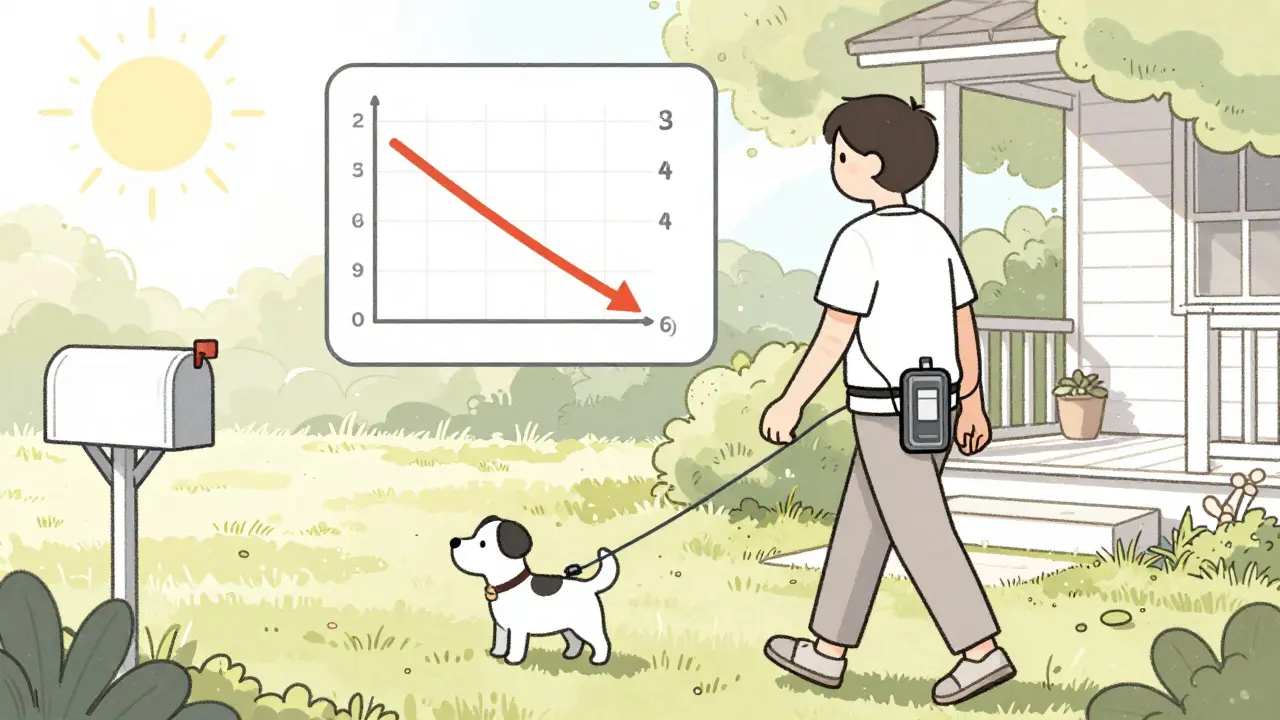
The trial lasts 5 to 7 days. Thin wires (leads) are threaded into your epidural space through a needle-no major surgery. The leads connect to an external battery pack you wear on your belt or clip to your waist. You go home and use it normally: walking, sitting, even sleeping. You track your pain levels, mobility, and sleep quality.
The trial is a success if your pain drops by at least 50%. If you only feel 30% better? The device won’t be implanted. Too many people skip this step and end up disappointed. The trial isn’t a formality-it’s the gatekeeper to real results.
What Happens During Implantation?
If the trial works, you schedule the permanent implant. It’s a same-day outpatient procedure under light sedation. The surgeon places the leads in the exact spot on your spine that matches your pain pattern. Then, a small device-about the size of a stopwatch-is tucked under your skin, usually in your buttock, abdomen, or upper hip.
The whole thing takes about 60 to 90 minutes. Most people go home the same day. Recovery is quick: avoid heavy lifting for 4 to 6 weeks, keep the incision clean, and watch for signs of infection-redness, swelling, fever, or pus.
It takes 2 to 4 weeks to get used to the device. Your brain needs time to adjust to the new signals. You’ll likely need at least one follow-up visit to fine-tune the settings. What felt perfect in the clinic might feel too weak or too strong at home. Programming is part of the process-not a one-time fix.
Real Results: What Patients Actually Experience
On average, 56% to 85% of well-selected patients get at least 50% pain reduction. That’s not a cure, but for someone who used to rate their pain at 9/10, dropping to 4/10 means you can finally sleep through the night. You can walk to the mailbox. You can stop taking opioids.
A 2021 JAMA study found SCS patients cut their opioid use by 57% in a year and 63% by year two. One patient on Reddit said her monthly medication bill dropped from $800 to $40. Another said he went from using a cane to walking his dog for 20 minutes a day.
But it’s not perfect. About 1 in 3 patients need a second surgery within two years. The most common reasons? Lead migration (the wires shift out of place), infection, or battery failure. One user on the Pain News Network forum had two revision surgeries in 18 months because his leads kept moving.
Device batteries last 5 to 9 years. When they die, you need another surgery to replace them. Some newer models, like Boston Scientific’s WaveWriter Alpha™ Prime, last up to 24 months on a single charge-but you still have to recharge them weekly.
SCS vs. Other Options
How does SCS stack up against other pain treatments?
| Treatment | Pain Relief (Avg.) | Invasiveness | Cost (USD) | Long-Term Use |
|---|---|---|---|---|
| Spinal Cord Stimulation (SCS) | 50-85% | Surgical (implant) | $25,000-$45,000 | Years (with revisions) |
| Opioid Medications | 30-50% (declines over time) | Non-invasive | $1,200-$5,000/year | Months (risk of dependence) |
| TENS Unit | 20-40% | Non-invasive | $50-$200 | Days to weeks |
| Peripheral Nerve Stimulation | 65-81% (for limbs) | Surgical (localized) | $20,000-$35,000 | Years |
| Back Surgery | 40-60% | Highly invasive | $50,000-$100,000 | Variable (often fails) |
SCS beats opioids in long-term safety and reduces dependency. It’s far more effective than TENS units, which are great for temporary relief but not chronic conditions. Compared to other nerve stimulators, SCS works better for back and leg pain but not as well for isolated arm or foot pain.
Limitations and Risks
SCS isn’t magic. It has real downsides:
- 18.7% of patients need revision surgery within two years
- 3.8% to 7.2% get infections that require device removal
- Lead migration happens in 15% of cases within six months
- Only 52% of patients still get strong pain relief after five years
- Out-of-pocket costs can hit $15,000-$25,000 even with insurance
And not everyone qualifies. You can’t get SCS if you’re pregnant, can’t operate the device, or failed the trial. Some systems are MRI-compatible, but not all. Boston Scientific’s Precision Montage™ MRI is safe for full-body scans at 1.5T and 3.0T. Older models? Not so much. You’ll need to check your device’s specs before any scan.
Who Should Avoid It?
SCS isn’t for people who:
- Want a quick fix
- Expect to be completely pain-free
- Can’t commit to follow-up visits and device management
- Have untreated mental health conditions
- Are on blood thinners and can’t stop them
- Have an active infection
It’s also not ideal for people whose pain is mostly in their arms or hands. Peripheral nerve stimulation works better there.
The Future of SCS
The field is moving fast. New systems like Boston Scientific’s Evoke® use closed-loop technology-they sense your nerve activity and adjust stimulation automatically. Early results show 83% of patients got meaningful relief at 12 months.
Devices are getting smaller, batteries are lasting longer, and waveforms are becoming smarter. High-frequency stimulation (10,000 Hz) is now mainstream and eliminates the tingling sensation that turned some people off.
But the biggest challenge isn’t technology-it’s selection. Too many patients get implanted without proper screening. The best outcomes come from careful evaluation: physical diagnosis, psychological screening, and a successful trial.
Final Thoughts
Spinal cord stimulation isn’t for everyone. But for the right person, it’s life-changing. It doesn’t erase pain. It gives you back your life. You might still have discomfort, but you won’t be trapped by it. You’ll sleep. You’ll move. You’ll stop relying on pills that make you dizzy, nauseous, or addicted.
If you’ve been living with chronic pain for years and nothing has worked, SCS might be worth exploring. Talk to a pain specialist who does trials. Ask about their success rates. Ask about their revision rates. Ask if they screen for depression. Don’t rush. This isn’t a decision you make in a week. It’s a decision you live with for years.
The data shows it works-for those who are truly selected. The question isn’t whether SCS is effective. The question is: are you the right candidate?
Is spinal cord stimulation painful?
The implant procedure is done under sedation, so you won’t feel pain during surgery. Afterward, there’s mild soreness at the incision sites, similar to any minor surgery. The stimulation itself usually feels like a gentle tingling or buzzing. Newer high-frequency and burst modes don’t cause tingling at all, so many patients report feeling nothing but pain relief.
Does insurance cover spinal cord stimulation?
Yes, Medicare covers SCS for approved conditions like failed back surgery syndrome, CRPS, and chronic leg or back pain. Most private insurers follow Medicare’s guidelines. However, coverage often requires proof that you’ve tried conservative treatments first and passed a trial stimulation. Out-of-pocket costs can still be $5,000 to $10,000 depending on your plan.
How long does the device last?
The implanted pulse generator (battery) lasts 5 to 9 years for non-rechargeable models. Rechargeable systems like Boston Scientific’s WaveWriter Alpha™ Prime last longer-up to 24 months between charges-but need weekly recharging. When the battery dies, you need a minor surgery to replace it, usually as an outpatient procedure.
Can I have an MRI with a spinal cord stimulator?
It depends on the device. Newer models like Boston Scientific’s Precision Montage™ MRI and Medtronic’s Intellis™ are designed to be MRI-safe under specific conditions (usually 1.5T or 3.0T scanners, with settings turned off). Older devices are not MRI-compatible. Always check your device’s manual and inform your radiologist before any scan.
What happens if the device stops working?
If your stimulation stops or changes, it could mean the leads have moved, the battery is low, or there’s a connection issue. Don’t panic. Keep using it as usual and contact your pain specialist. Most issues can be fixed with a quick programming adjustment. If the leads have migrated significantly, a revision surgery may be needed. About 15% of patients experience lead movement within six months.
Can SCS help with neuropathic pain in the feet?
SCS is most effective for pain in the lower back, buttocks, and legs. For isolated foot pain, peripheral nerve stimulation (targeting specific nerves in the foot) often works better. SCS can still help if the foot pain is part of a broader nerve condition like CRPS or diabetic neuropathy, but results are less predictable than for axial pain.



Paul Ong
Been through this myself and it changed everything
Richard Thomas
It's fascinating how technology can rewire our perception of suffering without altering the underlying pathology. The brain doesn't need the pain to stop-it just needs to stop believing it's in danger. That's the real magic here. Not the electrodes, not the waveform patterns, but the quiet renegotiation between nerve and mind. We treat pain like a broken pipe, but it's more like a misinterpreted alarm. And yet, we still demand cures when what we need is recalibration. The trial isn't just a filter-it's a mirror. It shows you whether you're ready to stop fighting your body and start listening to it.
Ann Romine
I'm from the Philippines and we don't have access to this kind of tech. My cousin has CRPS and they're using acupuncture and herbal baths. I wonder how much of this is accessible outside the US? Is it just a luxury for the insured?
Todd Nickel
The data on lead migration and revision rates is underdiscussed. 15% within six months isn't trivial-it's systemic. Why aren't we investing more in fixation technology? The fact that a device can shift position due to normal movement and then require another surgery suggests we're still in the early stages of biomechanical integration. Also, the battery replacement cycle is absurd. We're talking about a medical implant that needs surgery every 5–9 years, and yet we're not developing long-term power solutions like bio-batteries or kinetic charging. This isn't innovation-it's iterative patchwork.
Andy Heinlein
my buddy got the wavewriter last year and now he hikes every weekend. no more opioids. no more crying in the shower. just quiet mornings and coffee. it's not perfect but it's worth the risk. seriously, if you're stuck in pain hell, try the trial. you got nothing to lose but the suffering
Austin Mac-Anabraba
Let’s be real-this is just another corporate cash grab disguised as medical progress. The device costs $40k, the surgeon makes $15k, the rep gets a bonus, and you’re left with a battery that dies every 24 months. Meanwhile, the real cause of chronic pain-poor diet, sedentary lifestyles, environmental toxins-is ignored because it doesn’t come with a patent. They sell you a gadget to mute the symptom while the system keeps poisoning you. Wake up.
Phoebe McKenzie
Of course it works for some people-those who actually care about their health. But most of these patients are lazy, overweight, and addicted to painkillers. They want a magic button instead of doing physical therapy or losing weight. This isn’t medicine-it’s enabling. And now insurance pays for it? What happened to personal responsibility? People like this are drowning the system in unnecessary procedures.
gerard najera
It’s not about pain reduction. It’s about reclaiming autonomy.
Stephen Gikuma
Who funds these studies? Big Pharma? The device makers? You think they want you to heal? They want you dependent. Recharge weekly. Replace every 5 years. Get revisions. Pay premiums. This isn’t treatment-it’s a subscription model wrapped in electrodes. And they’re pushing it because opioids are getting regulated. They need a new addiction. Don’t fall for it.