Switching to generic medications saves money-sometimes hundreds of dollars a month. But what if you feel different after the switch? Maybe your pain isn’t as well controlled. Or you’re more tired. Or your mood dropped out of nowhere. You’re not imagining it. And you’re not alone.
Around 90% of prescriptions in the U.S. are filled with generics. They’re cheaper, FDA-approved, and work for most people. But for some, even tiny differences in how a generic is made can change how the drug behaves in your body. That’s why keeping a medication journal isn’t just helpful-it’s essential when you’re switching to or between generic versions.
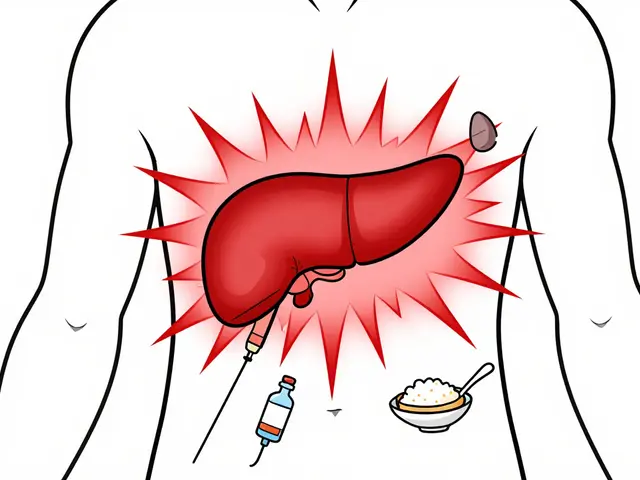
Why Generics Can Feel Different
Generics are required to be bioequivalent to brand-name drugs. That means they must deliver the same active ingredient within a certain range-80% to 125% of the original. Sounds precise, right? But that’s a 45% window. For drugs like warfarin, thyroid medicine, or seizure meds, even small shifts can mean the difference between control and crisis.
Take levothyroxine. One study found that switching manufacturers three times in six months led one patient’s TSH levels to swing from 1.2 to 8.7-far outside the normal range. That’s not a fluke. In 2013, heart transplant patients on a generic version of tacrolimus had unpredictable drug levels, leading to ER visits. Why? Because inactive ingredients (fillers, dyes, coatings) can affect how fast the drug dissolves. And not all manufacturers use the same ones.
Plus, generics from different companies can look almost identical. Same size. Same color. Same imprint. But they’re not the same pill. One might dissolve slower. Another might be more sensitive to heat or humidity. If you don’t track which version you’re on, you can’t connect symptoms to the right manufacturer.
What to Track in Your Journal
A good medication journal for generics doesn’t just say “took my pill.” It answers: Which one? When? How did I feel?
Here’s what to write down every time you fill a prescription:
- Drug name-both brand and generic (e.g., Synthroid vs. levothyroxine)
- Manufacturer-look on the bottle or pill. Names like Teva, Mylan, Dr. Reddy’s, or Aurobindo matter
- Lot number-found on the packaging. This is critical if there’s a recall or quality issue
- Physical details-color, shape, scoring, imprint code. Take a photo if you can
- Date of switch-when did you get this new version?
- Symptoms-use a 1-to-10 scale. Pain? Fatigue? Anxiety? Mood? Write it down daily
- Side effects-headaches? Nausea? Rash? Note when they started and how long they lasted
- Objective data-if you monitor blood pressure, blood sugar, INR, or TSH, record those numbers
- Adherence-did you miss a dose? Why? Ran out? Forgot? Felt worse?
Don’t guess. Be specific. “I felt weird” isn’t enough. “My headache started 2 hours after taking the new pill and lasted 6 hours” is. That’s the kind of detail that helps your doctor spot a pattern.
When Your Journal Matters Most
Not every drug needs this level of tracking. But for certain medications, it’s life-changing.
Narrow Therapeutic Index (NTI) drugs are the big ones. These are medications where the difference between a helpful dose and a dangerous one is very small. The FDA considers these high-risk:
- Warfarin (blood thinner)
- Levothyroxine (thyroid hormone)
- Phenytoin, carbamazepine, valproate (seizure meds)
- Cyclosporine, tacrolimus (transplant rejection drugs)
- Lithium (mood stabilizer)
For these, even a 5% variation in absorption can cause serious problems. One study found that 7.3% of epilepsy patients had breakthrough seizures after switching generic manufacturers. That’s more than six times higher than those who stayed on the same version.
And it’s not just about seizures or clots. People with depression, chronic pain, or autoimmune diseases report subtle but real changes in how they feel. One Reddit user wrote: “I switched from one generic antidepressant to another. My PHQ-9 score jumped from 8 to 16. I didn’t realize it until I looked back at my journal.”
Paper vs. Digital: Which Works Better?
You don’t need a fancy app. But you do need something consistent.
Paper journals still win for older adults. AARP found that 62% of people over 65 prefer writing by hand. They’re simple, private, and don’t need batteries. The CDC offers free printable templates with pre-filled columns for manufacturer, lot number, and symptom scales. A pack of 100 tear-off sheets costs under $5.
Digital tools like Medisafe and MyTherapy are popular with younger users. Medisafe has a 4.7-star rating from over 150,000 reviews. These apps send reminders, sync with pharmacies, and let you export data to share with your doctor. They’re great if you’re already using your phone for other health tracking.
But here’s the catch: 41% of people who start tracking quit within three months because it feels like a chore. The key? Make it part of your routine. Set a phone alarm for 10 minutes after you take your pill. Write it down before you brush your teeth. Tie it to an existing habit.
How Your Doctor Can Use It
Your journal isn’t just for you. It’s a tool for better care.
When you bring it to an appointment, you’re not just complaining-you’re giving evidence. A University of Michigan study found that patients who presented their medication journals had 32% fewer unnecessary drug changes and 27% higher adherence rates.
Pharmacists are especially good at reading these logs. Kaiser Permanente ran a program where pharmacists reviewed patient journals. The result? A 44% drop in generic-related medication switches. Why? Because they could see which manufacturer caused problems and suggest alternatives before symptoms got worse.
Even if your doctor doesn’t ask for it, bring it anyway. Say: “I’ve been tracking how I feel since I switched generics. I noticed this pattern-can we look at it together?”
What to Do If You Notice a Problem
If your journal shows a clear link between a new generic and worsening symptoms:
- Don’t stop the drug suddenly-especially for NTI meds
- Call your pharmacist. Ask: “Is this the same manufacturer as before?”
- Ask your doctor: “Can we try the previous version?”
- Check the FDA’s Orange Book. Look up your drug and see if it has an AB rating (interchangeable) or BX (not established)
- If you’re on an NTI drug, ask about a blood test. Serum levels can confirm if absorption changed
Some insurers will cover the brand-name drug if you can prove the generic isn’t working. Your journal is your proof.
Why Most People Don’t Journal-And How to Stick With It
Only 38% of people keep a journal beyond three months. The reasons? Too time-consuming. Too confusing. Too boring.
Here’s how to fix that:
- Start small. Track just one drug for two weeks. Not all of them.
- Use a template. The Cleveland Clinic’s NTI tracker has 6 clear columns. Download it. Print it.
- Link it to a habit. “After I take my pill, I write one line.” That’s all.
- Use voice notes. If writing feels hard, record a 15-second voice memo on your phone.
- Don’t aim for perfection. Missed a day? Just pick up tomorrow.
The goal isn’t to be a data scientist. It’s to notice the difference between “I feel okay” and “I feel worse than before.”
The Bigger Picture
Generic drugs save billions. But they’re not all created equal. The FDA inspects fewer than half of foreign manufacturing plants. And with 31% of those facilities still not inspected on time, quality control isn’t guaranteed.
That’s why patient-reported data matters. Between 2020 and 2023, 142 cases led to FDA label changes or manufacturing alerts-all because someone kept a journal.
And it’s getting easier. Apple Health now includes built-in generic tracking templates. The FDA is partnering with manufacturers to put QR codes on pill bottles that link to bioequivalence data. AI tools are being tested to predict when a change in your journal might signal trouble.
But none of that replaces your own observations. No algorithm knows how your body feels better than you do.
Final Thought
Generic drugs aren’t inferior. Most work perfectly. But when your health is on the line, you need more than a price tag. You need awareness. You need data. You need a journal.
It’s not about distrust. It’s about control. The more you know about what you’re taking and how it affects you, the more power you have to speak up-and get the right medicine.
Do I need to track every generic medication I take?
No. Focus on drugs with a narrow therapeutic index-like thyroid meds, blood thinners, or seizure drugs. For others, like antibiotics or pain relievers, tracking isn’t usually necessary unless you notice a clear change after switching.
Can I just rely on my pharmacist to tell me if a generic changed?
Pharmacists will alert you if the manufacturer changes, but they won’t know how it affects you. Your body’s response is unique. Only you can notice if you’re more tired, your pain returned, or your mood shifted. That’s why your journal matters.
What if my insurance keeps switching my generic?
That’s common. Insurance companies switch manufacturers to get lower prices. Keep your journal updated each time. If you notice a pattern-like worsening symptoms every time you get a new version-ask your doctor for a prior authorization for a specific brand or generic. Your journal gives you the evidence to support that request.
How long should I track before deciding a generic isn’t working?
For most drugs, give it 2-4 weeks. But for NTI drugs like thyroid or seizure meds, changes can happen within days. If symptoms appear right after a switch, don’t wait. Track daily and talk to your doctor within a week.
Are digital apps safe for storing my health data?
Yes, if they’re HIPAA-compliant. Apps like Medisafe and MyTherapy are. Avoid general note-taking apps like Notes or Google Keep unless you’re confident they’re secure. Always check the app’s privacy policy before entering health details.




christian jon
Let me tell you-this is the most important thing I’ve read all year. I switched my levothyroxine from Teva to Mylan, and within three days, I was a zombie. No joke. My heart was racing, I couldn’t sleep, and I thought I was having a panic attack. Then I checked the bottle-different manufacturer. I kept a journal for two weeks. The TSH spike? 1.8 to 9.4. I showed it to my endo. She cried. Literally. We switched back. Now I’m human again. If you’re on NTI meds-STOP. JUST. STOP. Assuming generics are interchangeable. Your life isn’t a spreadsheet.
Suzette Smith
I get what you’re saying, but honestly? I’ve switched generics 12 times in five years and never noticed a thing. Maybe you’re just sensitive? Or overthinking it? I mean, it’s the same active ingredient-why should the filler matter so much? I’ve got a cat with 17 allergies and even she doesn’t care if her pill is blue or green.
Autumn Frankart
They’re not just changing fillers. They’re changing the whole damn supply chain. Did you know 80% of generic pills are made in India and China? And the FDA inspects less than half? That’s not regulation-that’s a gamble. I’ve got a cousin who got a batch of generic warfarin with talc instead of magnesium stearate. He almost bled out. The FDA didn’t even issue a recall until three people died. This isn’t about ‘feeling weird.’ It’s about corporate negligence disguised as cost-cutting. And they call it ‘affordable healthcare.’ What a joke.
Skilken Awe
Okay, so you tracked your symptoms. Great. But did you control for confounders? Did you measure serum concentrations? Did you account for circadian rhythm fluctuations? Or are we just doing anecdotal medicine here? Also, ‘I felt worse’ isn’t data. It’s a feeling. Your journal is a glorified diary. The FDA doesn’t accept subjective scales. They want PK/PD curves. You’re not a scientist. You’re a guy with a notebook. And that’s dangerous.
andres az
Why are we even doing this? If the drug’s bioequivalent, why does it matter? It’s not like the pill has a soul. You’re anthropomorphizing pharmaceuticals. Also, why are we trusting patients to track this? I’ve seen people write ‘I felt 7/10 sad’ and then blame the pill. What if they just broke up? Or got fired? Or it’s January? This whole thing feels like a distraction from real healthcare problems-like access, cost, and insurance greed.
Steve DESTIVELLE
Perhaps the real question is not whether the pill changes but whether the self changes. We are not static entities. We are flux. The body is not a machine with fixed inputs and outputs. The pill may be identical, but the vessel-your being-is not. You track because you fear change. You write because you seek control. But control is an illusion. The only truth is the rhythm of the pulse, the breath, the silence between heartbeats. The journal is a cage. Let yourself be untracked.
Stephon Devereux
I love this post. Seriously. I’m a nurse practitioner, and I’ve been telling patients this for years. One of my patients on lithium switched generics and went into toxicity-her level was 1.8 when it should’ve been 0.6. She didn’t know the bottle changed. I asked her to start journaling. Two weeks later, she caught the pattern. We switched back. She’s been stable for 18 months. This isn’t hype. It’s science. And you? You can do this too. Start with one drug. One week. One line a day. You’ve got this. I believe in you.
Carla McKinney
Interesting. But let’s be honest: this is a tactic to make patients feel like they need to be their own pharmacists. Who benefits? The pharmaceutical companies who profit from brand-name drugs. The FDA? They’re underfunded. The system? Broken. This journal? It’s a Band-Aid on a hemorrhage. And you’re being manipulated into believing that tracking will fix systemic failure. It won’t. It’ll just make you tired. And guilty. And exhausted. And still on the same damn drug.
Ojus Save
man i tried journaling but i forgot to write for 3 days and then i felt bad so i stopped. now i just take my pills and hope for the best. also i think the blue one makes me sleepy and the white one makes me hungry idk maybe its placebo
Jack Havard
Here’s the real issue: insurance companies are forced to switch generics because they’re paid per prescription, not per outcome. So they don’t care if you crash. They care about the discount. Your journal doesn’t fix that. It just gives them more data to exploit. They’ll use your symptom log to deny coverage for the brand-name version. ‘Oh, you didn’t track consistently.’ ‘You didn’t provide enough data.’ ‘Your mood scale isn’t validated.’ This isn’t empowerment. It’s surveillance dressed up as self-care.
Gloria Ricky
Thank you for this. I started tracking my seizure meds after my last hospital stay. I didn’t think I could do it-but I did. Just one line a day. ‘Took Aurobindo. Headache. Slept 4 hrs.’ That’s it. And guess what? I caught the pattern before my next seizure. My neurologist was blown away. You don’t need to be perfect. You just need to show up. Even a little. You’re doing better than you think.
Stephon Devereux
Just saw @GloriaRicky’s comment. That’s exactly right. I had a patient last month who said she only wrote ‘felt okay’ every day. I told her: ‘That’s fine. Keep going.’ One day she wrote: ‘Headache after new pill.’ That was the breakthrough. You don’t need to be a data scientist. You just need to be consistent. And brave. And kind to yourself.