When your pancreas inflames, it doesn’t just hurt-it disrupts everything. Digestion slows, blood sugar swings, and even eating can feel dangerous. Two forms of this condition-acute and chronic-look similar at first, but they’re fundamentally different in how they strike, how they heal, and how you must eat to survive.
Acute Pancreatitis: A Sudden Attack
Acute pancreatitis hits fast. One day you’re fine; the next, you’re doubled over with sharp pain in your upper belly that shoots straight through to your back. Nausea, vomiting, fever-these aren’t just flu symptoms. They’re your body screaming that digestive enzymes, meant to break down food in the small intestine, are now eating your own pancreas.
This isn’t rare. In the U.S. alone, over 275,000 people end up in the hospital each year because of it. Most cases-about 80%-get better within a week with nothing more than fluids, rest, and pain control. But the other 20%? That’s where things get serious. If the inflammation triggers organ failure-like your kidneys or lungs shutting down-it can turn deadly. Mortality jumps from under 1% in mild cases to nearly 30% when organs fail for more than 48 hours.
The triggers? Gallstones and alcohol make up about 70% of cases. But there are others: high triglycerides, certain medications, autoimmune reactions, and in 1 in 5 cases, no clear cause at all. Diagnosis is straightforward: two out of three-severe abdominal pain, blood tests showing lipase levels tripled or higher, and imaging like a CT scan showing swollen pancreas tissue.
Chronic Pancreatitis: The Slow Burn
Chronic pancreatitis isn’t a flare-up. It’s a slow, steady destruction. Think of it like rust eating through metal. Over months or years, repeated inflammation turns healthy pancreatic tissue into scar tissue. The pancreas can’t produce enzymes anymore. It can’t regulate insulin. And the pain? It changes. Early on, it’s sharp after meals. Later, it fades-not because it’s better, but because the pancreas is too damaged to feel much at all.
It affects about 5 to 12 people per 100,000 globally. Eighty percent of cases link back to long-term alcohol use. Genetic mutations in genes like PRSS1 or SPINK1 explain most of the rest. Smoking? It doesn’t just add risk-it speeds up the damage. Quitting can cut disease progression by half over five years.
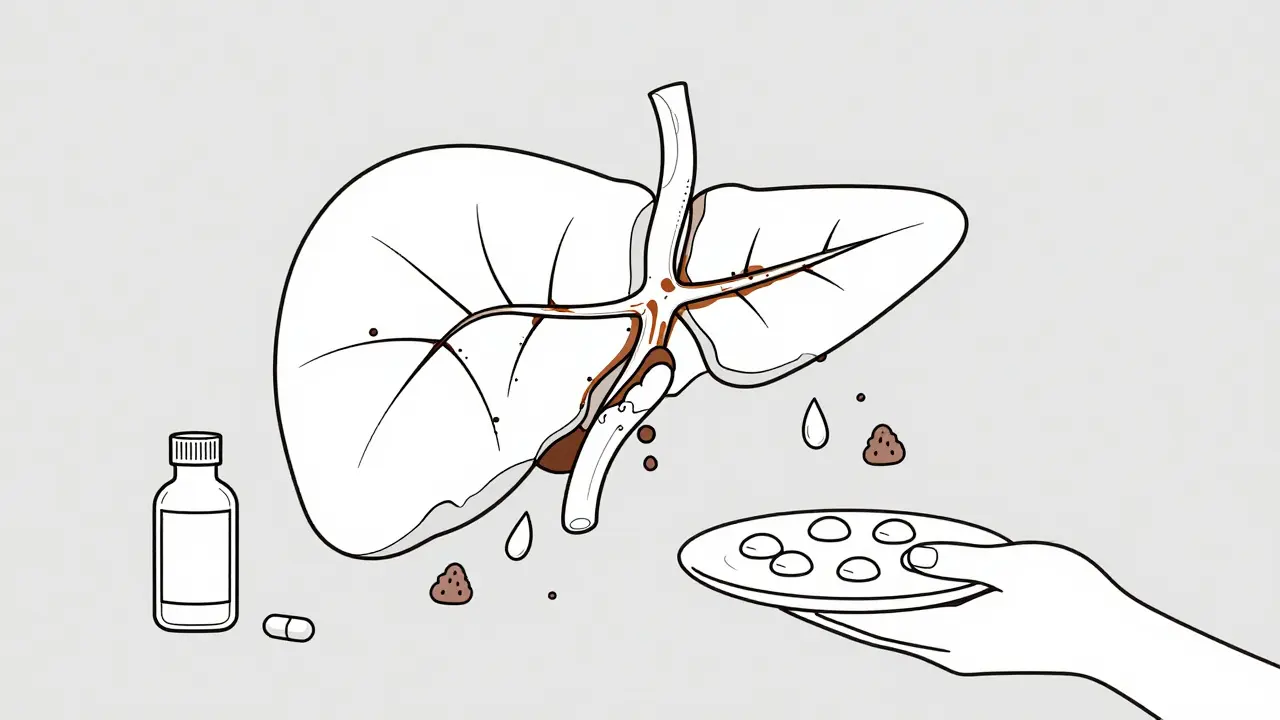
By the time most patients are diagnosed, their pancreas is already half-dead. Sixty to ninety percent develop exocrine insufficiency-meaning they can’t digest fat properly. That leads to steatorrhea: greasy, foul-smelling stools that float. And over time, half will develop diabetes. After 20 years, 90% will have lost most of their digestive function.
Key Differences Between Acute and Chronic
Here’s the breakdown:
- Onset: Acute comes suddenly. Chronic creeps in over years.
- Pain: Acute = constant, severe, radiating to back. Chronic = post-meal, dull, sometimes disappears as damage worsens.
- Lab tests: Acute = lipase skyrockets. Chronic = lipase may be normal, but fat in stool is high.
- Imaging: Acute = swollen pancreas. Chronic = calcifications, ducts widened or blocked.
- Recovery: Acute = often full recovery. Chronic = irreversible damage, lifelong management.
One critical fact: people with chronic pancreatitis have a 15 to 20 times higher risk of pancreatic cancer. That’s why annual MRI or MRCP scans are now recommended for long-term patients-even if they feel okay.
Nutrition in Acute Pancreatitis Recovery
When you’re in the middle of an acute attack, you’re not eating. Not for days. Your gut shuts down. Doctors give you IV fluids to keep your organs working. But here’s the game-changer: once the pain starts to ease, you need to start feeding your gut again-within 24 to 48 hours.
Studies show that starting enteral nutrition (through a tube into the small intestine) instead of waiting for oral intake reduces infection risk by 30%. That’s huge. And it’s not about starving the pancreas-it’s about feeding the gut. The pancreas doesn’t need to work hard to digest food if you’re giving nutrients directly past it.
When you can eat again, start small. Clear liquids. Then bland, low-fat foods: toast, rice, applesauce. Aim for 30 to 35 calories per kilogram of body weight daily. Protein? At least 1 gram per kilogram. That’s about 70 grams for a 150-pound person. Too little protein? You won’t heal. Too much fat? You’ll trigger another flare.
Nutrition in Chronic Pancreatitis: The Lifeline
If you have chronic pancreatitis, food isn’t just fuel-it’s medicine. And medicine needs a prescription.
First: pancreatic enzyme replacement therapy (PERT). You need to take these with every meal and snack. Dosing isn’t one-size-fits-all. For a main meal, 40,000 to 90,000 lipase units. For a snack? 25,000. If you’re still having greasy stools, your dose is too low. A 72-hour stool fat test can confirm it.
Second: fat restriction-but not elimination. During flares, cut fat to 20-30 grams a day. Long-term? 40-50 grams is fine, as long as you’re taking enzymes. But here’s the trick: avoid long-chain fats (like butter, oil, fatty meats). Instead, use medium-chain triglycerides (MCTs). These don’t need pancreatic enzymes to absorb. They’re in MCT oil, coconut oil, and some medical formulas. Patients who switch report fewer bowel movements and better weight gain.
Third: eat often. Six to eight small meals a day. Why? Large meals overwhelm your already weak system. Small, frequent bites keep your body steady and prevent blood sugar spikes-especially if you’ve developed diabetes.
Fourth: vitamins. You’re likely deficient. Eighty-five percent of chronic pancreatitis patients have low vitamin D. Forty percent lack B12. A quarter are low in vitamin A. These aren’t optional supplements. They’re essential. A daily multivitamin with fat-soluble vitamins (A, D, E, K) is non-negotiable. Many doctors now prescribe high-dose versions.
What Doesn’t Work
There are myths out there. One: “No fat means no pain.” False. Too little fat leads to malnutrition. Your body needs fat for hormones, brain function, and cell repair. Another: “Enzymes will fix everything.” Not if you’re taking them wrong. They must be taken right before or during meals. If you swallow them with water and wait 20 minutes, they’ll pass through your stomach and never reach the small intestine where they’re needed.
And opioids? They’re often prescribed for chronic pain. But 30% of patients end up dependent. Pain management should involve physical therapy, nerve blocks, and psychological support-not just pills.

Real Stories, Real Struggles
Sarah, 52, spent seven years misdiagnosed. She thought it was IBS. When she finally saw a pancreatic specialist, she was down 40 pounds. Her doctor switched her to MCT oil and raised her enzyme dose. Within three months, her bowel movements dropped from five times a day to one or two. She gained back 15 pounds.
Mark, 61, took 40,000 LU of enzymes with every meal and still lost 35 pounds. His body couldn’t absorb enough. He ended up on a feeding tube for three weeks. Now, he uses a specialized liquid nutrition formula. He’s stable-but he’ll need it for life.
They’re not outliers. These are the people who made it through. The ones who didn’t give up on food.
What’s New in Treatment
Science is catching up. A new biomarker called pancreatic stone protein (PSP) can predict how severe an acute attack will be within 24 hours-helping doctors decide who needs aggressive care. In chronic cases, stem cell therapy is being tested. Early results show a 30% improvement in enzyme production after a year.
Probiotics? A 2023 study found that Lactobacillus rhamnosus GG and Bifidobacterium lactis reduced pain by 40% over six months. Not a cure-but a helpful tool.
And for those with pancreatogenic diabetes, Dexcom G7, the first continuous glucose monitor approved specifically for this type, launched in early 2024. It tracks wild swings in blood sugar that regular monitors miss.
Final Thoughts
Acute pancreatitis is a wake-up call. Chronic pancreatitis is a lifestyle overhaul. Both demand respect for the pancreas-not as an organ you ignore until it hurts, but as the quiet engine of digestion and metabolism.
Recovery isn’t just about surviving the next attack. It’s about eating well, taking your enzymes, quitting smoking, avoiding alcohol, and staying on top of your labs. It’s about realizing that food isn’t the enemy-it’s the tool that keeps you alive.
If you’ve been diagnosed, find a specialist. Most primary care doctors aren’t trained for this. Look for a pancreas center. Ask about nutritionists who specialize in pancreatic disease. Don’t settle for vague advice. You deserve precision.
Because the pancreas doesn’t heal itself. But with the right care, it can still let you live.
Can acute pancreatitis turn into chronic pancreatitis?
Yes, but it’s not common. Repeated episodes of acute pancreatitis-especially if caused by alcohol, smoking, or gallstones-can lead to permanent damage over time. If you’ve had more than two acute attacks, especially with ongoing risk factors, you’re at higher risk for chronic pancreatitis. Early intervention and lifestyle changes can prevent this progression.
Do I need to take pancreatic enzymes forever if I have chronic pancreatitis?
Almost always. Once your pancreas loses its ability to produce digestive enzymes, it won’t regain it. Enzyme replacement therapy (PERT) is lifelong. Stopping them-even if you feel fine-leads to malnutrition, weight loss, and vitamin deficiencies. Dosing may change over time, so regular stool fat tests help your doctor adjust your prescription.
Can I drink alcohol again after recovering from acute pancreatitis?
No. Even if your attack was caused by gallstones, alcohol can still damage your pancreas. If alcohol triggered your attack, you must stop completely. Continuing to drink-even one drink a week-dramatically increases your risk of developing chronic pancreatitis, diabetes, and pancreatic cancer. Abstinence is the only safe choice.
Why do I still have pain even though I’m taking enzymes?
Enzymes help with digestion, not pain. Chronic pancreatitis pain comes from nerve damage, inflammation, and scarring. Enzymes won’t fix that. You may need pain specialists, nerve blocks, physical therapy, or medications like gabapentin. Some patients benefit from low-dose antidepressants, which can calm overactive pain nerves. Don’t assume your enzymes aren’t working-your pain might need a different treatment path.
Is there a special diet for pancreatitis?
Yes, but it’s not a fad diet. Focus on small, frequent meals with moderate fat (40-50g/day), high protein, and complex carbs. Use MCT oil instead of butter or olive oil. Avoid fried foods, creamy sauces, and processed snacks. Supplement with vitamins A, D, E, K, and B12. Work with a dietitian who knows pancreatic disease-generic low-fat diets often miss key needs like enzyme timing and nutrient density.
Can I eat dairy with chronic pancreatitis?
Yes-but choose wisely. Whole milk, cheese, and ice cream are too high in long-chain fats and can trigger steatorrhea. Opt for low-fat or non-fat dairy, or use lactose-free alternatives fortified with MCT oil. Some people tolerate yogurt with live cultures better because the bacteria help break down lactose. Always pair dairy with your enzyme dose.
How do I know if my enzyme dose is right?
Three signs: your stools are no longer greasy or floating, you’re not losing weight, and you’re not bloated or gassy after meals. But the gold standard is a 72-hour fecal fat test. If your stool contains more than 7% fat, your dose is too low. Talk to your doctor about scheduling this test-it’s the only way to know for sure.
Should I get screened for pancreatic cancer if I have chronic pancreatitis?
Yes-if you’ve had chronic pancreatitis for more than five years, especially if you smoke, drink, or have a family history of pancreatic cancer. Annual MRI or MRCP scans are recommended. Early detection is critical: pancreatic cancer is often found too late. Surveillance doesn’t prevent cancer, but it can catch it early enough to treat.
Can stress make pancreatitis worse?
Stress doesn’t cause pancreatitis, but it can worsen pain and slow healing. High stress raises inflammation markers and may trigger flare-ups in chronic cases. Mindfulness, therapy, and even light exercise like walking can reduce pain perception and improve quality of life. Managing stress isn’t optional-it’s part of treatment.
What should I do if I miss a dose of enzymes?
If you miss a dose before a meal, take it as soon as you remember-even if you’re halfway through eating. If you forget until later, don’t double up at the next meal. Just take your regular dose then. Missing one dose won’t cause harm, but consistently skipping them leads to malnutrition. Set phone reminders or keep a small pill case with your enzymes in your bag or wallet.




Glenda Marínez Granados
So let me get this straight… we’re telling people to stop drinking, quit smoking, eat MCT oil like it’s cereal, and take enzymes like they’re candy… but the pancreas still gets to be a drama queen? 😏
At this point, I’m just waiting for the FDA to approve a pancreas Netflix subscription. ‘Binge-watch your way to better digestion.’
MAHENDRA MEGHWAL
It is with profound respect for the medical science presented herein that I acknowledge the gravity of pancreatic pathology. The precision of diagnostic criteria and the evidence-based nutritional interventions reflect a commendable advancement in clinical practice. One must, however, exercise utmost diligence in adherence to enzyme replacement therapy, as deviation may precipitate irreversible metabolic consequences. Thank you for this illuminating exposition.
Sangeeta Isaac
so like… pancreas = broken blender that still thinks it’s a chef? 🤡
you gotta feed it tiny bites, use special oil (mct?? sounds like a new crypto), and take pills with every snack or it throws a tantrum and makes your poop look like oil paint.
also why does everyone have to be on a 72-hour poop test?? like… i didn’t sign up for this when i ordered the tacos.
but honestly? this is the most useful medical article i’ve ever read. i’m telling my mom. she thinks i’m just ‘sensitive to fat’… she’s gonna cry.
Alex Carletti Gouvea
Look, I don’t care if your pancreas is ‘quiet’ or ‘drama.’ If you’re eating that much fat, you’re doing it wrong. This isn’t a yoga retreat-it’s a medical emergency. We don’t need MCT oil and probiotics-we need discipline. American healthcare is coddling people into chronic illness. Stop treating organs like pets. Time to toughen up.
Philip Williams
This is an exceptionally comprehensive overview of pancreatitis management. I appreciate the clarity between acute and chronic forms, and the emphasis on early enteral nutrition is critical. The data on enzyme dosing and MCT oil utilization is particularly compelling. I would encourage clinicians to integrate these protocols into standard practice. Well-researched and well-presented.
Ben McKibbin
Let’s be real: the pancreas doesn’t care if you’re ‘busy’ or ‘forgot.’ It’s not a suggestion-it’s a biological contract. Take your enzymes. Eat small. Use MCT oil. Quit the booze. No exceptions.
I’ve seen too many people treat this like a diet trend-‘I’ll just cut back on fat’-until they’re down 50 pounds and on a feeding tube. This isn’t about willpower. It’s about survival. And if you’re still drinking? You’re not just hurting yourself-you’re disrespecting everyone who fought to get here.
Melanie Pearson
How many of these patients are obese? How many are on Medicaid? How many ignored their doctor for five years while eating nachos and energy drinks? This article reads like a pity party for poor lifestyle choices.
And now we’re prescribing MCT oil like it’s a miracle? Let me guess-next they’ll recommend yoga and affirmations for liver failure. The system is broken. Stop rewarding negligence with medical band-aids.
Rod Wheatley
Okay, real talk: I had acute pancreatitis in 2020. I thought I’d be fine after a week. I wasn’t. I didn’t know about enzymes. I didn’t know about MCT oil. I lost 40 pounds. I cried in the grocery store because I couldn’t eat cheese.
Then I found a pancreatic dietitian. She told me: ‘Your pancreas isn’t broken-it’s just tired.’ She taught me to eat every 3 hours. She told me to take enzymes WITH the first bite-not after. She gave me a pill case with a timer.
Now? I’m back to hiking. I still take enzymes. I still avoid butter. But I eat. I live. And I’m not sorry. If you’re reading this and you’re struggling? You’re not alone. Reach out. Ask for help. You deserve to eat without fear.
Uju Megafu
THIS IS WHY AMERICA IS DYING.
People think they can drink, eat fried chicken, and then just ‘take a pill’ and fix it? NO.
My cousin had this. He drank every weekend. Said ‘it was just one beer.’ Then he got cancer. Died at 43.
NO MORE EXCUSES.
STOP THE WHINING.
THE PANCREAS ISN’T A TOY.
IF YOU’RE STILL DRINKING, YOU’RE A DEAD MAN WALKING.
AND YES, I’M TALKING TO YOU, GUY WHO JUST LIKED THIS POST WHILE DRINKING A BEER.
Jarrod Flesch
Just wanted to say thanks for this. I’ve been living with chronic for 8 years. Took me 5 to find a doc who actually knew what PERT meant.
MCT oil changed my life. No more floating toilet disasters. I use it in coffee now. Tastes weird at first, but you get used to it. And yeah, I take enzymes with every bite-even peanut butter on toast.
Also, stress? Big one. I started walking 20 mins a day. Not for fitness. For my brain. It helps more than you’d think.
You’re not alone. Keep going. 💪🌿
Kelly McRainey Moore
My grandma had this. She was 72, never drank, never smoked. Just… got it. No idea why.
She took her enzymes like clockwork. Ate six tiny meals. Ate MCT oil like it was butter. And she lived to 91.
She used to say: ‘My pancreas is my quietest friend. I treat it right, it lets me keep eating pie.’
I’m gonna start doing the same. Thanks for the reminder.
lokesh prasanth
Enzymes dont fix pain. Only painkillers do. So why are we ignoring the real issue? The nerve damage. The scarring. The truth? Most of this is just placebo with a prescription.