What Really Works for IBS? Not All Diets Are Created Equal
If you’ve been living with bloating, cramps, or unpredictable bathroom trips, you’ve probably tried every diet under the sun. You cut out gluten. You went dairy-free. You even tried eating only rice and chicken for weeks. But nothing stuck. That’s because IBS isn’t one problem-it’s a mix of triggers, and the right diet depends on what’s actually bothering you.
The good news? Three science-backed eating plans exist to help you find your personal sweet spot: the low-FODMAP diet, the low-residue diet, and elimination diets. They’re not the same. They don’t all work for everyone. And using the wrong one can make things worse.
The Low-FODMAP Diet: The Gold Standard for IBS
Backed by over 20 clinical trials and developed by researchers at Monash University in Melbourne, the low-FODMAP diet is the most effective dietary tool for IBS today. It doesn’t just cut out "bad" foods-it targets a specific group of short-chain carbohydrates that ferment in your gut and pull water into your intestines, causing bloating, gas, and diarrhea.
FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. That’s a mouthful, but it boils down to five types: fructans (in wheat, garlic, onions), galacto-oligosaccharides (in beans and lentils), lactose (in milk and soft cheeses), excess fructose (in apples, honey, mango), and polyols (in mushrooms, stone fruits, sugar-free gum).
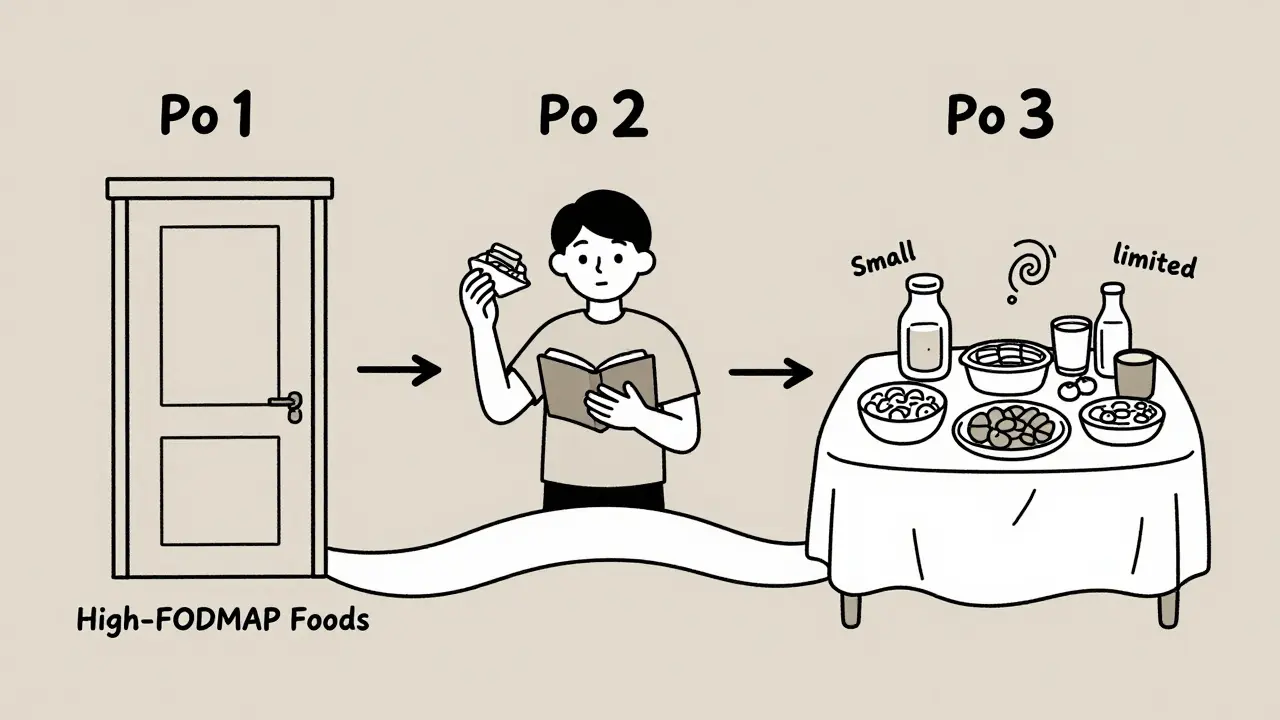
This isn’t a lifelong restriction. It’s a three-phase system:
- Elimination (2-6 weeks): You remove all high-FODMAP foods. No garlic, no onions, no wheat bread, no apples. You eat only low-FODMAP options like bananas, carrots, rice, eggs, and lactose-free dairy. Portion size matters-1 teaspoon of garlic is fine, but 2 teaspoons can trigger symptoms.
- Reintroduction (8-12 weeks): You test one FODMAP group at a time. Start with 3 grams of fructans (like 1/2 cup of cooked pasta). Wait 3 days. Track symptoms. Then move to lactose, then fructose. This is where you learn your personal triggers.
- Personalization (ongoing): Most people can bring back 50-80% of the foods they cut out. You don’t need to avoid onions forever-you just can’t have more than a pinch.
Studies show 75-80% of IBS patients see major improvement. One Reddit user, after 15 years of daily diarrhea, said: "FODMAP eliminated my symptoms in 3 weeks." The Monash FODMAP app (rated 4.8/5 with over 28,000 reviews) is essential-it gives you exact portion sizes and scans barcodes to check if a product is safe.
Low-Residue Diet: Not for Most IBS Patients
The low-residue diet was designed in the 1940s for people with Crohn’s disease or before colon surgery. It’s not made for IBS. But because it reduces stool volume, some doctors still suggest it for diarrhea-predominant IBS.
Here’s what it requires:
- Less than 10-15 grams of fiber per day (normal intake is 25-38 grams)
- No raw fruits or vegetables
- No nuts, seeds, whole grains, or legumes
- Limited dairy (only lactose-free options)
- White bread, white rice, eggs, lean meats, and canned fruits without skins
It can help reduce frequency of bowel movements in the short term. But here’s the catch: 60-70% of IBS patients don’t need this level of restriction. And it’s nutritionally risky. Folate drops by 35%. Calcium intake falls 25%. Long-term use increases osteoporosis risk.
It also does nothing for bloating or abdominal pain-the two most common IBS symptoms. In fact, Monash University data shows low-FODMAP reduces bloating in 75% of cases, while low-residue only helps 45%. If you have constipation-predominant IBS, this diet will make it worse.
General Elimination Diets: Too Broad, Too Risky
Elimination diets sound simple: cut out common triggers like dairy, gluten, caffeine, and alcohol for 2-4 weeks, then add them back one by one.
But without structure, they’re a guessing game. You might cut out gluten because you think it’s the problem-only to find out your real trigger is fructose in apples or polyols in sugar-free candy. A University of Virginia study found only 30% of people correctly identify their triggers without professional guidance.
Unlike FODMAP, there’s no standard dosing. You don’t know how much lactose or fructose you’re testing. You might eat a whole glass of milk and get sick, then assume you’re lactose intolerant-when you’re actually sensitive to the FODMAPs in milk, not the lactose itself.
These diets are useful if you don’t have access to a FODMAP-trained dietitian. But they’re not a replacement. They’re a backup plan.
Who Should Use What?
Let’s cut through the noise. Here’s a clear guide:
| IBS Type | Best Diet | Why | Avoid This |
|---|---|---|---|
| Diarrhea-predominant (IBS-D) | Low-FODMAP | Targets gas and water buildup that causes loose stools | Low-residue (too restrictive, doesn’t help bloating) |
| Constipation-predominant (IBS-C) | Low-FODMAP (modified) | Focus on low-FODMAP high-fiber foods like oats, chia seeds, kiwi | Low-residue (worsens constipation) |
| Bloating and pain dominant | Low-FODMAP | Proven to reduce bloating in 75% of cases | General elimination diets (too vague) |
| Unclear symptoms or limited access to dietitian | General elimination (short-term) | Helps rule out obvious triggers like dairy or caffeine | Low-residue (unnecessary restrictions) |
The Hidden Costs of DIY Dieting
Many people start the low-FODMAP diet on their own-using YouTube videos, Pinterest lists, or free apps. That’s where things go wrong.
Hidden FODMAPs are everywhere. Soy sauce? Contains wheat. Protein bars? Often have inulin or agave syrup. "Healthy" snacks like trail mix? Loaded with cashews (high in GOS) and dried fruit (high in fructose). A University of Virginia analysis found 60% of packaged "healthy" foods contain hidden high-FODMAP ingredients.
And the reintroduction phase? That’s where most people quit. It’s uncomfortable. You might feel bloated for a few days after testing lactose. You think you’re failing. But that’s the point-you’re learning.
Without a dietitian, 55% of people skip reintroduction entirely. That means they stay on a restrictive diet longer than needed. And that’s dangerous. Monash research shows Bifidobacterium (a good gut bacteria) drops 40% in just four weeks on low-FODMAP. That’s why you must bring foods back in.
What You Need to Succeed
Success isn’t about willpower. It’s about tools and support.
- Monash FODMAP app: $9.99/month or $49.99/year. Worth every cent. It tells you safe portions, scans barcodes, and has over 1,200 tested foods.
- Food scale: Buy one that measures to 1 gram. A tablespoon of honey might be safe. Two tablespoons? Not anymore.
- Symptom journal: Track everything: what you ate, when, and how you felt. Use a simple notebook or a free app like MySymptoms.
- Professional help: If you can afford it, see a registered dietitian trained in FODMAP. Monash has certified providers in 37 countries. If you’re in Australia, check their directory. In the U.S., ask your GI doctor for a referral.
Meal prep helps. Cook 4 days’ worth of meals on Sunday. Keep low-FODMAP snacks handy: hard-boiled eggs, rice cakes with peanut butter (check label!), lactose-free yogurt.

What to Expect-Real Talk
Day 1-7: You’ll feel overwhelmed. Grocery shopping takes hours. You’ll miss bread, garlic, and fruit.
Day 10-14: Magic happens. Bloating drops. Pain eases. You sleep better. You start to believe this might work.
Week 4-6: You’re ready for reintroduction. You test fructans. You feel bloated. You panic. But you keep going. You test lactose. No reaction. You test fructose. You get cramps. Now you know: you’re sensitive to fructose, not lactose.
By week 12: You’re eating more than you thought possible. You can have a small apple. A sprinkle of garlic. A slice of sourdough. You’re not on a diet anymore-you’ve rebuilt your life around what your body can handle.
When Not to Try This
Some people shouldn’t attempt the low-FODMAP diet.
- If you have an eating disorder: Restriction can trigger relapse. The VA Whole Health Library warns it’s contraindicated in 15% of IBS cases.
- If you’re underweight or malnourished: This diet can worsen nutrient gaps.
- If you’re not ready for structure: You need patience. You need to track. You need to test. If you want a quick fix, this isn’t it.
And if you’ve tried everything and still feel awful? Talk to your doctor. IBS isn’t always the culprit. Celiac disease, small intestinal bacterial overgrowth (SIBO), or even bile acid malabsorption can mimic IBS.
What’s Next for IBS Diets?
Science is moving fast. Monash just launched a 5-year study to predict who responds to FODMAP based on gut bacteria. AI-powered meal planners are coming. By 2026, your electronic health record might auto-suggest low-FODMAP meals based on your symptoms.
But the core won’t change: IBS isn’t cured by diet. It’s managed by knowledge. The goal isn’t to eat perfectly. It’s to eat freely-without fear.





Ryan Pagan
Man, I wish I'd found this two years ago. I was eating nothing but rice and chicken for six months thinking I was 'cleaning up' my gut. Turned out I was just starving my microbiome. The FODMAP breakdown here? Pure gold. I used the Monash app during reintroduction and found out I'm fine with garlic-just not onion. Now I eat pesto like it's my job. Life changed.
Paul Adler
This is one of the most balanced and evidence-based explanations of IBS dietary approaches I've encountered in a long time. The distinction between low-FODMAP and low-residue is particularly well-articulated, and the emphasis on professional guidance is both necessary and refreshing. Thank you for taking the time to clarify these nuances.
DHARMAN CHELLANI
fodmap is just a fancy way to say eat boring food. if u r so sensitive u prob need to chill out and eat some real food. also who uses an app to check if their bread is safe?? lmao
Kacey Yates
I tried FODMAP and it worked but then I got so depressed eating nothing but eggs and rice I started binging on gluten and dairy and ended up worse. This article says nothing about mental health. You can't just diet your way out of trauma. Also typo in paragraph 3. Its not 'monash' its 'monash'.
ryan Sifontes
fodmap is a big pharma scam to sell apps. they dont want you to heal naturally. i cured my ibs with bone broth and moon cycles. also the monash app tracks your location. they know when you eat a garlic clove.
Laura Arnal
This is SO helpful!! I’ve been stuck in the IBS loop for years and this finally made sense 😊 I started the FODMAP plan last week and already feel lighter! The part about portion sizes? Game changer. I thought I had to give up apples forever-turns out half a small one is fine! Thank you for the real talk 🙌
Eli In
As someone who’s lived in 5 countries and tried every ‘gut cleanse’ under the sun, this is the first thing that actually clicked. The FODMAP phases make sense like a puzzle-you’re not just removing food, you’re decoding your body. Also, the emoji in the app? So cute. I’ve screenshot every safe snack like it’s a treasure map 🗺️🍎🥚
Keith Oliver
You’re all missing the point. The low-residue diet is for people who actually know what they’re doing. FODMAP? That’s for people who can’t handle real food. I’ve been on low-residue for 8 years and I’m healthier than most people who think ‘kale’ is a superfood. Also, you don’t need an app-you need discipline. And if you’re using a food scale, you’re already broken.
rajaneesh s rajan
Interesting. But isn’t it funny how we treat IBS like it’s a glitch in the system? Like if we just delete the right carbs, our guts will magically become perfect machines? Maybe the problem isn’t the food-it’s the pressure to eat perfectly. I mean, who even decided that bloating is the enemy? Maybe it’s just your body whispering, ‘hey, slow down.’
paul walker
just started the elimination phase and its brutal but worth it. i cooked 4 days of meals on sunday and now i have rice cakes with pb and hard boiled eggs ready to go. no more panic eating at 2am. thank you for the tips. i got a food scale too. its tiny but life changing 💪
Andy Steenberge
One thing no one talks about enough: the emotional toll of reintroduction. You test lactose, feel bloated, and immediately think you failed. But that’s not failure-that’s data. I cried the first time I ate a slice of sourdough after six weeks. It wasn’t perfect. I felt something. But I didn’t run to the bathroom. That was the moment I stopped seeing food as an enemy. This isn’t about restriction. It’s about reclaiming joy in eating. The Monash app didn’t cure me. The patience did. And the willingness to be uncomfortable for the sake of understanding. You’re not broken. You’re just learning your body’s dialect. Keep going. You’re doing better than you think.