Every year, millions of Medicare beneficiaries get a free, in-depth review of all their medications - but many miss out because they don’t know how to get ready. If you’re taking multiple pills, supplements, or over-the-counter drugs, this review isn’t just a formality. It’s a chance to catch dangerous interactions, lower your costs, and make sure every medication you take is still helping you.
What Exactly Is a Medicare Annual Medication Review?
This is officially called a Comprehensive Medication Review (CMR). It’s required by Medicare for all Part D plan sponsors to offer at least once a year to eligible beneficiaries. It’s not just a quick chat at the pharmacy counter. It’s a 30- to 60-minute one-on-one session with a pharmacist who looks at every single thing you take - prescription drugs, vitamins, herbal supplements, pain relievers, even eye drops or creams.
The goal? To find problems you might not even know about. Maybe you’re taking two drugs that clash. Maybe you’re paying too much for something cheaper. Maybe you’ve stopped taking a pill because it made you dizzy, but no one asked you why. The pharmacist will check for duplicates, side effects, adherence issues, and whether any meds are no longer needed.
By law, you get a written summary after the review: a Consultation Letter, a Medication Action Plan, and a Personal Medication List. These aren’t just paperwork - they’re tools you can share with your doctor, family, or next pharmacist.
Who Qualifies for the Review?
You don’t automatically get one just because you’re on Medicare. To qualify in 2026, you must meet these three criteria:
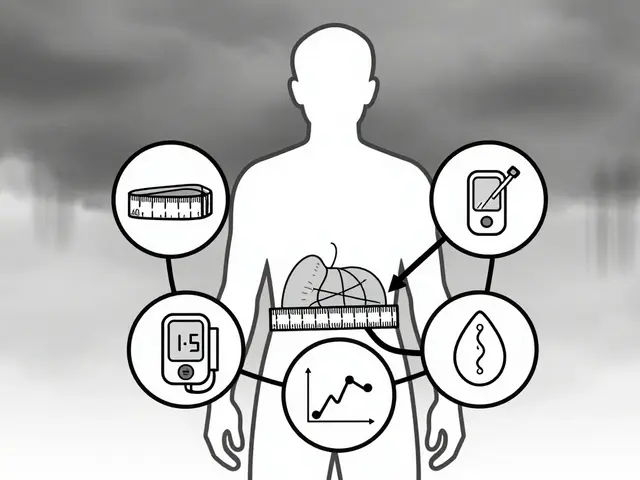
- You have at least three chronic conditions like diabetes, heart disease, COPD, high blood pressure, or kidney disease.
- You take eight or more Part D-covered prescription medications (including maintenance drugs like statins or insulin).
- You’ve spent at least $1,623 out-of-pocket on covered Part D drugs in the last year.
That sounds strict, but Medicare updated the rules in 2025 to make it easier to qualify. In 2024, the cost threshold was higher. Now, more seniors are eligible - especially those managing multiple conditions on expensive meds.
Even if you don’t meet all the criteria, call your Part D plan. Some plans offer reviews to others who might benefit. Don’t assume you’re not eligible - ask.
Why This Review Matters More Than You Think
Studies show seniors on multiple medications are three times more likely to have a dangerous drug interaction. Many of these aren’t caught during a 10-minute doctor visit. Pharmacists, however, are trained to spot them.
In 2023, a review of 1,245 CMR participants found that 63% of seniors had at least one medication issue identified - like a duplicate drug, an unnecessary prescription, or a side effect they never reported. One woman in Ohio was taking two different blood thinners. Her doctor didn’t know. The pharmacist caught it during her CMR and stopped one - avoiding a possible hospital stay.
Cost savings are real too. In 2022, Medicare beneficiaries saved an average of $380 per year after switching to lower-cost alternatives identified during their review. That’s not just a few bucks - it’s groceries, gas, or a new pair of shoes.
And it’s not just about pills. Herbal supplements like St. John’s Wort can interfere with antidepressants. Garlic pills can thin your blood. Fish oil? It’s fine for most - but if you’re on warfarin, it can be risky. Pharmacists know this stuff. You might not.
How to Prepare: The 5-Step Checklist
Preparation is the biggest factor in whether your CMR helps you. A 2024 survey by the Medicare Rights Center found that 78% of seniors who brought full medication lists rated their review as “very helpful.” Only 42% of those who came without them did.
Here’s how to get ready - and it won’t take hours.
- Gather every medication you take. Collect all prescription bottles, OTC boxes, vitamin containers, and supplement jars. Don’t skip the aspirin, antacids, sleep aids, or topical creams. Bring them in their original packaging. This takes 20-30 minutes.
- Make a written list. Write down the name, dose, frequency, and reason for each one. Example: “Lisinopril 10 mg, once daily, for high blood pressure.” Include when you started each one if you know. If you don’t, write “don’t know.” Better than nothing.
- Write down your concerns. What’s bothering you? Dizziness after taking your blood pressure pill? Trouble swallowing big pills? Forgetting to take your diabetes meds on weekends? Cost issues? Write them all down. Even if you think it’s silly. The pharmacist has heard it all.
- Bring recent health changes. Did you go to the ER last month? Have new lab results? Start or stop a new activity? Any falls, confusion, or changes in appetite? These matter. They might explain why a medication isn’t working or is causing side effects.
- Bring someone with you. If you can, bring a family member or friend. Memory fades. You’ll forget to ask something important. A second set of ears helps. If you can’t bring someone, record the conversation on your phone (ask permission first).
Pro tip: Take photos of each pill bottle with your phone. That way, if you lose the physical bottles, you still have the info. Many seniors do this now - it’s quick, easy, and saves time.

What Happens During the Review?
The pharmacist will start by asking you to confirm your list. They’ll compare it to what’s in their system (from pharmacy claims or your doctor’s records). Don’t be surprised if they say, “I see you’re taking this, but you haven’t picked it up in 6 months.” That’s normal. They’re looking for gaps.
Then they’ll ask questions:
- Do you take your meds at the same time every day?
- Do you ever skip doses because they’re too expensive or make you feel bad?
- Do you use a pill organizer? Does it work?
- Are you taking anything not on this list?
They’ll check for:
- Duplicate medications (two drugs doing the same thing)
- Drug interactions (like mixing blood thinners with NSAIDs)
- Unnecessary prescriptions (meds you no longer need)
- Cost-saving options (generic alternatives, mail-order discounts)
- Adherence barriers (too many pills, confusing schedules)
They might suggest:
- Stopping a drug that’s no longer needed
- Switching to a cheaper brand
- Changing the time you take a pill to avoid drowsiness
- Using a pill box or reminder app
You’ll get a printed Medication Action Plan with next steps - like who to contact about a change, or when to follow up. Keep it. Show it to your doctor.
Common Mistakes People Make
Even when people mean to prepare, they mess up. Here’s what not to do:
- Bringing only your prescriptions. OTC meds and supplements are just as important. One man skipped his fish oil because he thought it wasn’t “real medicine.” It was interacting with his blood thinner.
- Trying to remember everything. Memory fails. Don’t rely on it. Bring the bottles.
- Not asking questions. If you don’t understand why you’re taking a pill, say so. No judgment.
- Thinking the doctor already knows. Doctors see dozens of patients a day. They don’t know every pill you take unless you tell them - and even then, they might not catch it.
- Waiting for the plan to call you. You have to initiate the review. Call your Part D plan. Don’t wait.
What If You Can’t Get a CMR?
If you don’t qualify, you still have options.
Ask your pharmacist for a Targeted Medication Review (TMR). These are shorter, but still useful. They’re offered quarterly and focus on specific issues - like a new prescription or a side effect you reported.
You can also schedule a free medication check at your local pharmacy. Many independent pharmacies offer this for free, even if you’re not on Medicare. Bring your list. Ask: “Can you check for interactions or if anything here is outdated?”
And if you’re still struggling - reach out to the Medicare Rights Center or your State Health Insurance Assistance Program (SHIP). They offer free one-on-one counseling. No cost. No pressure.
What Comes After the Review?
Don’t just file the paperwork and forget it.
Keep your Personal Medication List. Update it every time you get a new prescription or stop one. Share it with any new doctor or specialist. If you go to the ER, show it to the nurse.
Follow up on any action steps. If the pharmacist suggested switching to a generic, call your pharmacy. If they told you to talk to your doctor about stopping a med, schedule that appointment. Don’t wait.
And mark your calendar. Your next CMR is due in 365 days. Set a reminder now. Don’t wait for them to call.
Real Stories, Real Results
One 74-year-old man in Florida was taking six pills a day. He felt tired all the time. He didn’t think it was related. During his CMR, the pharmacist found he was on two different statins - one prescribed by his cardiologist, another by his primary care doctor. He was taking both. The pharmacist stopped the duplicate. Within two weeks, his energy came back.
A woman in Texas was paying $180 a month for her diabetes pill. The pharmacist found a generic version for $12. She switched. Saved $2,000 a year.
Another senior in Ohio was taking melatonin for sleep - but also a sedative prescribed by her doctor. The pharmacist warned her: combining them could cause dangerous drowsiness. She stopped the melatonin. Her doctor adjusted the sedative. She hasn’t fallen since.
These aren’t rare. They happen every day. But only if you show up prepared.
Final Tip: Don’t Wait Until It’s Too Late
Medication problems don’t always show up as emergencies. Sometimes, they creep in slowly - fatigue, confusion, dizziness, stomach upset. You might think it’s just aging. It might be your meds.
This review isn’t about being told what to do. It’s about getting the right information so you can make smarter choices. You’re not just a patient. You’re the manager of your own health. And this is your tool.
Take 45 minutes now. Gather your bottles. Write down your questions. Call your plan. Don’t wait. Your next CMR could be the one that changes how you feel - every single day.



Jan Hess
Just did my CMR last week and holy crap it saved me $400 on my blood pressure med alone. I brought my whole medicine cabinet and the pharmacist caught me taking two different versions of the same statin. I didn’t even know I was double-dipping. Now I feel like a genius for showing up.
Diane Hendriks
It is imperative to note that the federal government mandates these reviews not out of benevolence, but as a cost-containment mechanism to reduce hospitalizations stemming from polypharmacy. The Medicare Part D program is not a charity; it is a fiscal safeguard. Those who neglect to prepare are not merely careless-they are complicit in systemic inefficiency.
Tom Doan
Interesting. So the government now expects us to become amateur pharmacists just to avoid being penalized for not knowing what’s in our own medicine cabinet? And yet, the same system won’t fix the absurd pricing of insulin. The irony is thick enough to spread on toast.
Sohan Jindal
They want you to bring all your pills so they can track you. Next they’ll put a chip in your pill bottle. This is how they control the elderly. You think this is about helping? No. It’s about data. They know what you take. They know when you skip. They know when you’re weak. Watch your back.
Frank Geurts
Allow me to extend my profound appreciation for this meticulously articulated exposition on the Comprehensive Medication Review protocol. The structural clarity, coupled with the empirical substantiation of cost-savings and safety outcomes, constitutes a paradigmatic exemplar of public health communication. I have forwarded this to my local Senior Center for inclusion in our monthly wellness bulletin. Well done.
Annie Choi
CMR is a game-changer for polypharmacy management-especially when you’re juggling anticoagulants, beta-blockers, and OTC NSAIDs. The pharmacist’s action plan is the only thing that actually gets synced with your EHR. Don’t skip it. Period.
Arjun Seth
You think this is hard? Back in my village in Punjab, we took one pill a day and knew why. Now you need a PhD just to take aspirin. This is what happens when you let the West over-medicate everyone. You don’t need a review-you need less pills and more yoga.
Ayush Pareek
Hey, if you’re reading this and thinking ‘I’ll do it next year’-stop. Just call your plan today. Grab those bottles. Write down your dizziness or the stomach pain or the confusion. Don’t wait for someone to fix it for you. You’re the boss of your body. This review? It’s your superpower. You got this.