Clarithromycin Drug Interaction Checker
Dangerous Combination Alert
Clarithromycin can cause life-threatening interactions with certain medications. This tool helps identify high-risk combinations.
Based on FDA warnings and medical guidelines, do NOT take clarithromycin with these medications:
- Colchicine (gout medication)
- Simvastatin or Lovastatin (common statins)
- Heart medications like amiodarone, verapamil, or sotalol
Check Your Medications
Clarithromycin is a powerful antibiotic used to treat infections like pneumonia, bronchitis, and skin infections. But here’s the problem: it doesn’t just kill bacteria-it can also dangerously interfere with dozens of other medications you might be taking. In fact, mixing clarithromycin with certain drugs can lead to life-threatening complications, including kidney failure, muscle breakdown, irregular heart rhythms, and even death. These aren’t rare theoretical risks. They’ve killed people. And they’re still happening today.
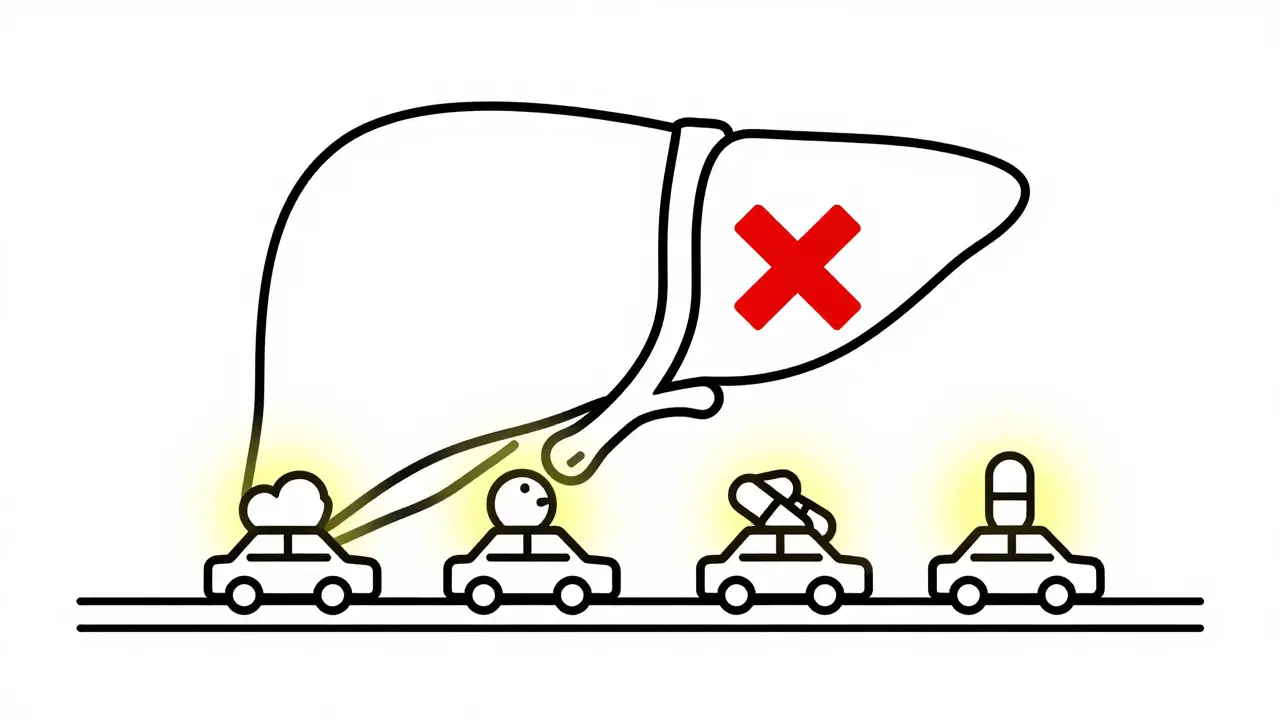
Why Clarithromycin Is So Dangerous with Other Drugs
Clarithromycin doesn’t just work on bacteria-it also shuts down a key enzyme in your liver called CYP3A4. This enzyme is responsible for breaking down about half of all prescription drugs. When clarithromycin blocks it, those drugs build up in your bloodstream like traffic jammed on a highway. Some of them can reach toxic levels in just a few days.
Compared to other antibiotics in its class, clarithromycin is one of the worst offenders. Azithromycin, another macrolide, barely touches CYP3A4. That’s why doctors now prefer azithromycin for most infections-especially in older adults or people on multiple medications. Clarithromycin’s inhibition of CYP3A4 is so strong that one study showed it increased the concentration of colchicine by nearly three times. That’s enough to turn a routine gout pill into a poison.
The Deadliest Combination: Clarithromycin and Colchicine
If you take colchicine for gout or familial Mediterranean fever, you need to hear this: never take clarithromycin with it.
Colchicine is already a narrow-therapeutic-index drug-meaning the difference between a helpful dose and a deadly one is tiny. When clarithromycin blocks its breakdown, colchicine levels skyrocket. The result? Severe diarrhea, vomiting, muscle weakness, nerve damage, and multi-organ failure. According to the FDA, there are 58 documented cases of serious or fatal reactions between these two drugs as of 2020. Twenty-two of those cases ended in death.
One real case involved a 76-year-old woman with chronic gout. She took her usual colchicine dose while on clarithromycin for a chest infection. Eleven days later, she was dead. Her family didn’t know the two drugs could kill together. Her doctor didn’t check her meds.
The FDA added a boxed warning to clarithromycin’s label in March 2023-its strongest possible alert-specifically naming colchicine as a lethal combination. The American College of Physicians now advises doctors to avoid clarithromycin entirely in patients taking colchicine. There is no safe dose. No timing trick. No workaround. Just avoid it.
Statins: When a Cholesterol Drug Turns Deadly
Clarithromycin also turns common cholesterol-lowering drugs into ticking time bombs. Simvastatin and lovastatin are the worst offenders. Both are metabolized by CYP3A4. When clarithromycin blocks their breakdown, muscle tissue starts breaking down-a condition called rhabdomyolysis.
Rhabdomyolysis can lead to kidney failure, dialysis, and death. One documented case involved a 68-year-old man on simvastatin 40mg daily. He started clarithromycin for a sinus infection. Within 72 hours, he was in the ICU with severe muscle pain, dark urine, and failing kidneys. He needed dialysis to survive.
Atorvastatin is less risky but still dangerous. The Mayo Clinic lists simvastatin and lovastatin as absolute no-gos with clarithromycin. If you’re on one of these statins, your doctor should switch you to pravastatin, rosuvastatin, or fluvastatin-drugs that don’t rely on CYP3A4 for metabolism.
Heart Medications: Risk of Sudden Death
Clarithromycin doesn’t just raise drug levels-it can also mess with your heart’s electrical rhythm. It prolongs the QT interval, a measure of how long your heart takes to recharge between beats. When combined with other QT-prolonging drugs, this can trigger a deadly arrhythmia called torsades de pointes.
Drugs like verapamil, diltiazem, amiodarone, and sotalol are all risky when paired with clarithromycin. Even common blood pressure meds like amlodipine can become dangerous in combination. The American Heart Association warns that clarithromycin increases the risk of torsades de pointes by 2.7 times compared to safer antibiotics.
Patients with existing heart conditions, low potassium, or kidney disease are at highest risk. Yet, many prescriptions still slip through. A 2022 Medscape case report described a pharmacist catching a dangerous combo: clarithromycin given to a 72-year-old with atrial fibrillation who was also taking rivaroxaban and colchicine. The pharmacist intervened just in time.
Other Dangerous Interactions You Can’t Ignore
- Digoxin: Clarithromycin can raise digoxin levels by up to 50%, leading to nausea, confusion, and fatal heart rhythms.
- Warfarin: Increased bleeding risk due to slowed metabolism. INR levels can spike unpredictably.
- Theophylline: Used for asthma and COPD. Toxicity causes seizures and cardiac arrest.
- Ergotamine: Used for migraines. Combined with clarithromycin, it can cause limb ischemia and gangrene.
- Immunosuppressants like cyclosporine and tacrolimus: Levels can double or triple, leading to kidney damage or organ rejection.
The Mayo Clinic’s interaction checker currently flags 142 drugs as contraindicated with clarithromycin. That’s not a typo. One hundred forty-two. And that’s just the ones we know about.
Who’s Most at Risk?
Older adults. People on multiple medications. Those with kidney problems. These aren’t edge cases-they’re the majority of clarithromycin users.
Studies show that 42% of patients over 65 taking clarithromycin are also on at least one contraindicated drug. The American Geriatrics Society’s Beers Criteria (2023) explicitly says: avoid clarithromycin in anyone 65+ who’s taking CYP3A4 substrates with a narrow therapeutic window. That includes colchicine, statins, digoxin, and many others.
And here’s the kicker: many of these interactions happen because no one checks. Prescribers focus on the infection. Pharmacists are overwhelmed. Patients don’t know to speak up.
What Should You Do?
If you’re prescribed clarithromycin, ask these questions right away:
- What other medications am I taking that could interact with this?
- Is there a safer alternative like azithromycin?
- Am I on any statins, colchicine, heart meds, or kidney-affecting drugs?
- Can you check my full medication list before I start this?
If you’re on any of the high-risk drugs listed above, don’t take clarithromycin. Period. Azithromycin works just as well for most common infections-and it doesn’t carry this risk.
Even if you’ve taken clarithromycin before without problems, that doesn’t mean it’s safe now. Your body changes. Your meds change. Your kidneys slow down with age. What was fine last year could kill you this year.
The Bigger Picture: Why This Keeps Happening
Clarithromycin prescriptions have dropped 28% since 2015. Azithromycin now makes up 63% of macrolide prescriptions in the U.S. Why? Because doctors are learning the hard way.
Pharmaceutical companies are even working on a new version of clarithromycin with less CYP3A4 inhibition-but it won’t be available until at least 2026. Until then, the risk remains.
Clarithromycin isn’t evil. It saves lives in specific cases-like treating Mycobacterium avium complex in people with advanced HIV. But for routine infections? The cost is too high. The data is clear. The warnings are loud. And the deaths are real.
If you’re a patient, speak up. If you’re a caregiver, double-check. If you’re a provider, screen every time. Because one missed interaction can end a life.
Can I take clarithromycin if I’m on a statin?
No, not if you’re taking simvastatin or lovastatin. These two statins can build up to toxic levels when combined with clarithromycin, causing muscle breakdown and kidney failure. Atorvastatin carries some risk too. Safer alternatives include pravastatin, rosuvastatin, or fluvastatin. Always check with your pharmacist or doctor before starting clarithromycin if you’re on any cholesterol medication.
Is azithromycin safer than clarithromycin?
Yes, significantly. Azithromycin has minimal effect on the CYP3A4 enzyme, so it rarely causes dangerous drug interactions. For most common infections like sinusitis, bronchitis, or strep throat, azithromycin works just as well as clarithromycin-and without the risk of fatal side effects. Many doctors now prescribe azithromycin as the default macrolide, especially for older patients or those on multiple medications.
How long does clarithromycin stay in my system?
Clarithromycin has a half-life of 3 to 7 hours, meaning it clears from your bloodstream in about a day. But its effect on the CYP3A4 enzyme lasts much longer-up to several days after your last dose. That’s why even if you stop clarithromycin, you still need to wait before restarting certain medications like colchicine or statins. Always ask your doctor for specific timing guidance.
What should I do if I accidentally took clarithromycin with colchicine?
Stop both medications immediately and seek medical help right away. Symptoms of colchicine toxicity include severe diarrhea, vomiting, muscle pain, weakness, and dark urine. These can appear within days. Even if you feel fine, go to the ER. Blood tests can detect rising toxin levels before symptoms become severe. This is a medical emergency.
Are there any foods or supplements I should avoid with clarithromycin?
Unlike some antibiotics, clarithromycin doesn’t interact with food, though the extended-release form must be taken with meals for proper absorption. However, avoid grapefruit juice-it can also inhibit CYP3A4 and increase drug levels. There’s no evidence that herbal supplements like St. John’s wort or garlic affect clarithromycin, but always disclose all supplements to your doctor before starting any new antibiotic.





Neil Ellis
Man, this post is a godsend. I’ve seen so many older folks get prescribed clarithromycin like it’s candy-no checks, no questions. My grandma nearly died last year because her cardiologist didn’t know she was on colchicine. She ended up in the ER with muscle cramps so bad she couldn’t stand. Azithromycin would’ve been fine. Why do we still let this happen?
Doctors aren’t evil-they’re just overwhelmed. But this isn’t a gray area. It’s a red flag with a siren on it.
Malik Ronquillo
Clarithromycin is just a death sentence wrapped in a prescription label. I don’t care if you’re 25 or 85-if you’re on any statin, colchicine, or heart med, just say no. Azithromycin exists for a reason. Stop being lazy and switch.
Also-grapefruit juice? Yeah, that’s just the cherry on top of your suicide sundae.
Brenda King
Thank you for writing this. I’m a nurse and I see this every week. A 70-year-old man on simvastatin gets clarithromycin for a sinus infection. Two days later he’s in the hospital with rhabdo. His family didn’t even know he was on a statin. We need better systems. Not just warnings-mandatory EHR alerts. It’s not enough to hope someone reads the label.
Also-azithromycin is the new standard. Period. End of story.
❤️
Daphne Mallari - Tolentino
While the clinical data presented is undeniably compelling, one must consider the broader pharmacoeconomic context in which such prescribing patterns persist. The inertia of entrenched clinical protocols, coupled with the absence of real-time decision support infrastructure in primary care settings, renders even the most explicit FDA warnings insufficient to alter behavior at scale. Moreover, the implicit assumption that azithromycin is universally preferable neglects the nuanced microbiological indications where clarithromycin’s superior tissue penetration remains clinically indispensable-such as in Mycobacterium avium complex prophylaxis in immunocompromised hosts. The conflation of risk with absolute contraindication risks creating a new category of therapeutic nihilism.
That said, the documented mortality statistics are horrifying and demand systemic reform-not merely patient education.
Tatiana Bandurina
Let’s be real-this isn’t about drug interactions. It’s about lazy prescribing. Doctors don’t check med lists because it takes 30 seconds and they’re running behind. Pharmacists don’t catch it because they’re processing 200 scripts an hour. Patients don’t speak up because they think the doctor knows best.
So we get bodies. Not because the science is unclear. Because the system is broken.
And now you’re all acting like you’re surprised.
Lana Kabulova
Wait-I’ve been on clarithromycin twice before, once with atorvastatin, and I’m fine. Why are you all acting like this is some universal death sentence? My uncle took it with colchicine and lived. You’re overhyping this. Not everything is a medical emergency.
Also, why is azithromycin always the answer? What if it doesn’t work? You’re ignoring the fact that some infections actually need clarithromycin. This post feels like fearmongering dressed up as education.
Margaret Khaemba
Hey, I’m a med student and I just read this. This is insane. I had no idea how dangerous this was. I’m going to start asking every patient I see: ‘Are you on colchicine? Statins? Any heart meds?’
Also-can someone explain why grapefruit juice is bad? I thought it was just for blood pressure pills?
Thanks for this. I’m gonna share it with my whole cohort.
Keith Helm
Stop. The FDA issued a boxed warning. The American College of Physicians recommends avoidance. The Beers Criteria lists it as inappropriate for elderly patients on CYP3A4 substrates. The evidence is conclusive. Your anecdote does not override systematic data. Do not take clarithromycin with contraindicated medications. Period.
Oren Prettyman
Interesting how this post frames clarithromycin as some uniquely dangerous drug when in reality, nearly every antibiotic has interaction risks. Ciprofloxacin with theophylline. Trimethoprim with warfarin. Vancomycin with nephrotoxins. Why is this one getting the spotlight? Because it’s convenient. Because it fits the narrative that older drugs are evil and newer ones are saviors. Azithromycin isn’t perfect-it’s linked to QT prolongation too, just less often. But we don’t hear about that. We get clickbait headlines about ‘deadly combos’ while ignoring the real issue: fragmented care, lack of pharmacist involvement, and poor EHR integration.
Also, the author mentions 142 interactions. That’s not a feature-it’s a bug of the interaction checker software, which flags anything remotely plausible, even if the risk is theoretical or negligible. This isn’t medicine. It’s alarmist marketing dressed in white coats.