Tolerance Loss: What It Is, Why It Happens, and How It Affects Your Medications
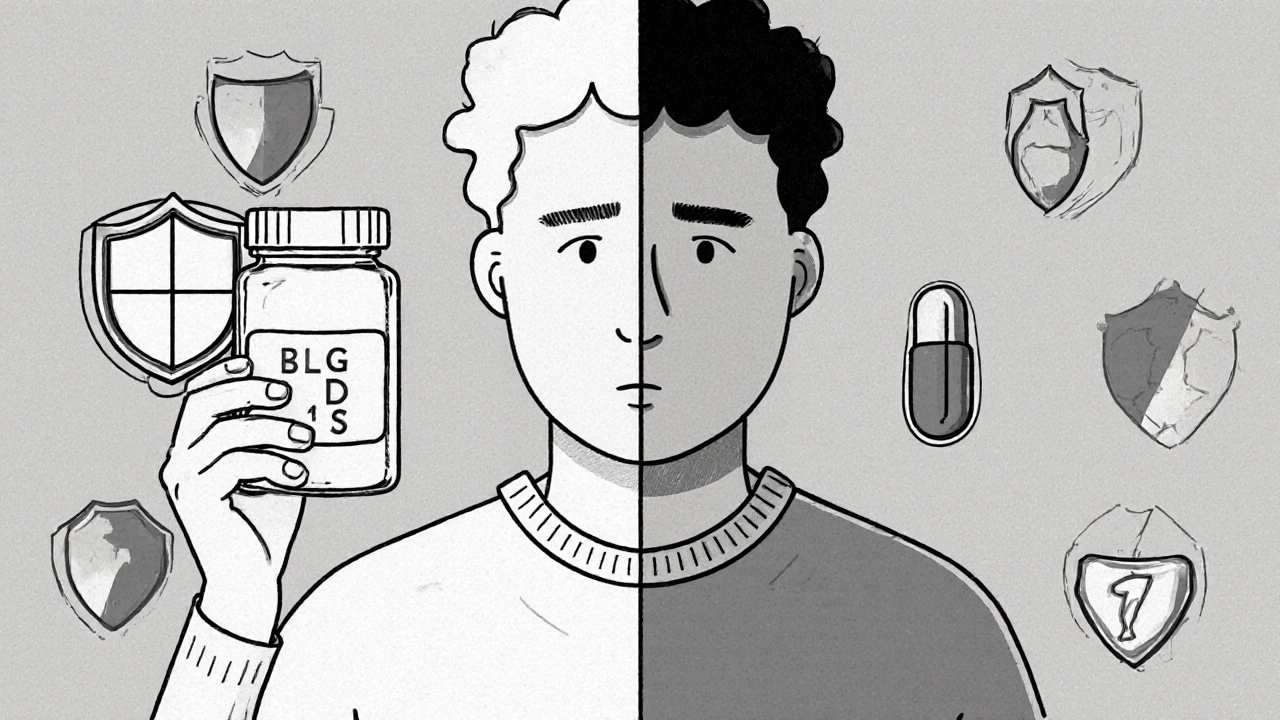
When your body stops responding to a drug the way it used to, you might be experiencing tolerance loss, a change in how your system reacts to a medication after prolonged use. Also known as pharmacological tolerance, it’s not just about needing higher doses—it’s about your body adapting in ways that can make treatment less effective or even risky. This isn’t just a problem with painkillers or opioids. It shows up with antidepressants, blood pressure meds, sleep aids, and even antibiotics. The moment your body gets used to a drug, it starts adjusting its own chemistry to counteract it. That’s why a dose that once worked perfectly might suddenly feel weak—or stop working altogether.
Tolerance loss doesn’t always mean you’re taking too much. Sometimes, it happens after you’ve been on a steady dose for months, or even years. Your liver enzymes might start breaking down the drug faster. Your brain receptors might become less sensitive. Or your kidneys might clear it out too quickly. Drug tolerance, the body’s reduced response to a medication over time is often confused with addiction, but they’re not the same. You can have tolerance without craving the drug. And you can have addiction without tolerance. What matters is the effect: if your medication isn’t doing what it should, your health is at risk.
One of the biggest dangers? When tolerance loss leads to sudden withdrawal. If you’ve been on a medication long enough for your body to adapt, stopping it cold can trigger shaking, anxiety, nausea, or worse. That’s why doctors don’t just tell you to quit—they guide you through tapering. Withdrawal symptoms, the physical and mental reactions that occur when a drug is reduced or stopped after regular use are real, and they vary wildly depending on the drug. Antidepressants? Brain zaps. Blood pressure meds? Spike in heart rate. Sleep aids? Insomnia worse than before.
And here’s the thing: tolerance loss isn’t always obvious. You might not notice your pain isn’t as controlled, or your blood pressure is creeping up, until it’s too late. That’s why tracking your symptoms matters. Keep a simple log: what you take, when, and how you feel. Small changes add up. If you’re on a long-term medication, ask your doctor: Is this still working the way it should? Don’t assume it is. Many people don’t realize their meds have lost their punch until they’re in crisis.
What you’ll find in the posts below are real-world stories and science-backed facts about how tolerance loss shows up in everyday treatments. From HIV drugs that lose power because of enzyme changes, to beta-blockers that stop lowering heart rate, to antidepressants that suddenly feel useless—these aren’t edge cases. They’re common. And they’re fixable—if you know what to look for. This isn’t about stopping your meds. It’s about making sure they still work for you.