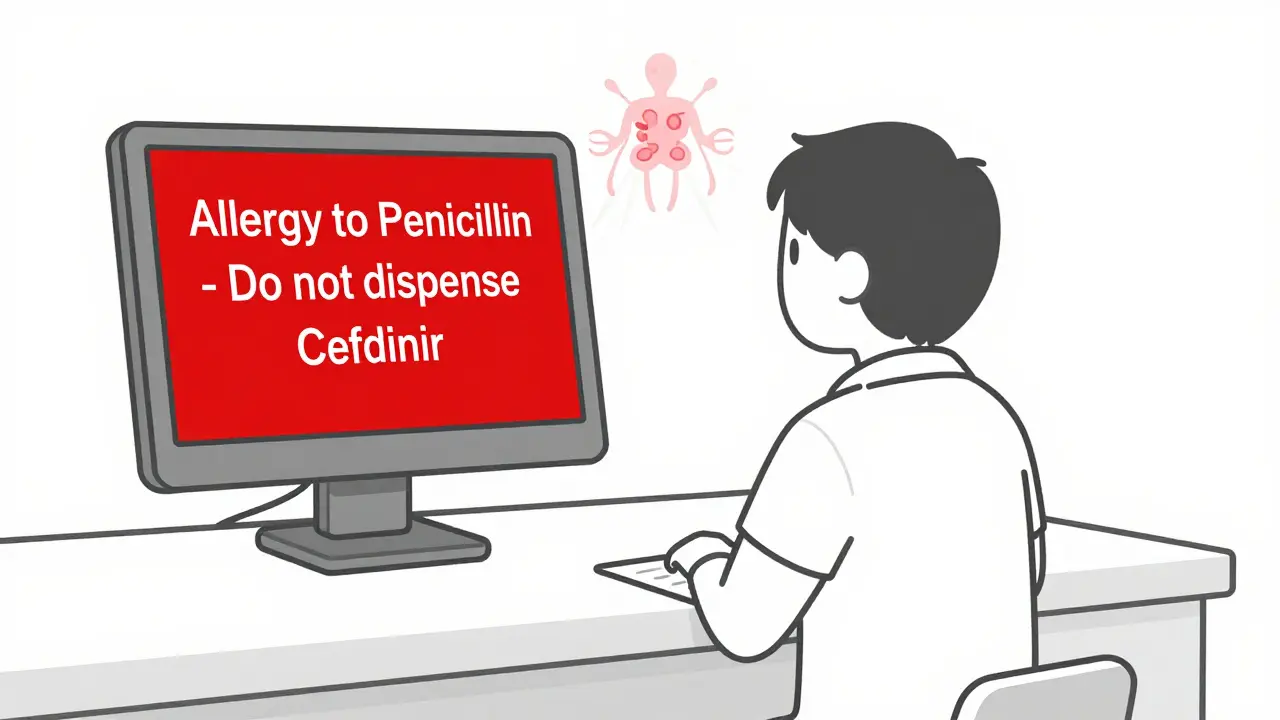
When you pick up your prescription, you might see a red or yellow pop-up on the pharmacist’s screen. It says: "Allergy to Penicillin - Do not dispense Cefdinir." You wonder: Is this real? Did you actually have a reaction? Or is this just a computer glitch from a system that screams wolf too often?
Pharmacy allergy alerts are everywhere now. Nearly every pharmacy in Australia, the U.S., and Europe uses them. They’re built into the electronic systems that handle your prescriptions - Epic, Cerner, Meditech. These alerts are supposed to save lives. But too often, they just annoy you and your pharmacist.
What You’re Seeing Isn’t Always a Real Allergy
Most of these alerts aren’t about true allergies. They’re about class-based assumptions. If your chart says "penicillin allergy," the system flags every drug in the penicillin family - and sometimes even drugs that have nothing to do with it, like cephalosporins or even NSAIDs. That’s because older systems treat all "allergies" the same, no matter how mild.
Here’s the truth: only 5-10% of people who say they’re allergic to penicillin actually are. A 2019 Cochrane review found that less than 2% of people with a penicillin label have true IgE-mediated reactions - the kind that cause anaphylaxis. The rest? They had a rash as a kid, threw up after taking amoxicillin, or got a stomach ache. None of those are allergies. But the system doesn’t know that. It just sees the word "allergy" and triggers a red alert.
Understanding the Two Types of Alerts
There are two kinds of alerts you’ll see:
- Definite allergy alert: The drug you’re getting is the same as or very similar to something you’ve documented as an allergy. Example: You’re allergic to amoxicillin, and the system blocks another penicillin.
- Possible allergy alert: The drug isn’t the same, but it’s in the same class. Example: You’re flagged for cefdinir because you have a "penicillin allergy." This is a cross-reactivity alert.
Here’s the kicker: 90% of all allergy alerts are possible allergy alerts. And most of them are wrong.
A 2020 study in the Journal of Allergy and Clinical Immunology: In Practice found that clinicians misinterpreted the difference between these two types 42% of the time. That means almost half the time, someone skips a safe drug because they thought the alert meant "danger" - when it really meant "maybe."
What the Colors and Symbols Really Mean
Each EHR system uses colors and symbols differently. Epic uses:
- Yellow = Mild reaction (rash, itching)
- Orange = Moderate (hives, swelling)
- Red = Severe (difficulty breathing, anaphylaxis)
- Black = Life-threatening (requires mandatory override confirmation)
Cerner uses a simpler three-tier system. But here’s the problem: even when the color is red, the alert might still be wrong. A 2022 study found that 75-82% of red alerts for anaphylaxis were overridden - not because doctors were careless, but because the patient had taken the same drug three times before without issue.
Don’t trust the color alone. Look at the reaction description next to it. Was it "hives after penicillin"? That’s worth paying attention to. Was it "nausea after amoxicillin"? That’s not an allergy. That’s a side effect.
Why These Alerts Are So Wrong - And Why That’s Dangerous
These systems were built on old assumptions. For decades, doctors were taught that if you’re allergic to penicillin, you’re allergic to all cephalosporins. That’s not true. Modern data shows cross-reactivity between penicillins and third- or fourth-generation cephalosporins is less than 2%. Yet most systems still treat them like the same thing.
And it’s getting worse. A 2021 NIH study found that 47% of EHR systems don’t even ask for details about the reaction. They just let you pick "allergy" from a dropdown. So if you say "I got a rash," the system doesn’t know if it was from penicillin, stress, or a new soap. It just flags everything.
This creates alert fatigue. Clinicians see 12-15 alerts per 100 prescriptions. Most are useless. So they start clicking "OK" without reading. That’s dangerous. Because when a real, life-threatening alert pops up - like a patient with a documented anaphylaxis to morphine - the system might be ignored simply because it’s lost credibility.
What You Can Do: Be Your Own Advocate
You don’t have to accept these alerts as gospel. Here’s what to do:
- Check your own allergy list. Go to your My Health Record or ask your GP for a copy. Does it say "penicillin allergy"? Or does it say "stomach upset after amoxicillin at age 7"? If it’s vague, ask to update it.
- Ask: Was this a true allergic reaction? True allergies involve your immune system. Signs: hives, swelling of lips/tongue, wheezing, drop in blood pressure. If it was nausea, diarrhea, or headache - it’s not an allergy.
- Ask about alternatives. If you’re being denied a drug because of an alert, ask: "Is there a test to confirm this?" Many hospitals now offer penicillin skin testing. It’s quick, safe, and 95% accurate.
- Update your records. If you’ve taken a drug since the alert was added - and you didn’t react - tell your doctor. That’s the only way to fix the system.
A 2022 study at Johns Hopkins showed that when patients were asked to describe their reactions in detail - not just "allergy" - accurate documentation jumped from 39% to 76% in six months. That’s huge. And it’s something you can help with.

The Future: Smarter Alerts Are Coming
Change is happening. Epic’s 2023.2 update introduced "Allergy Relevance Scoring" - a machine learning tool that learns from how often doctors override certain alerts. If 90% of people override a penicillin-cephalosporin alert, the system starts downgrading it from red to yellow.
Oracle Health (formerly Cerner) now integrates with allergist records. If you’ve had a drug challenge test and were cleared, the system automatically removes the alert.
And by 2026, 70% of major EHR systems will use risk-stratified alerting. That means:
- True anaphylaxis? Loud, mandatory alert.
- Stomach ache from ibuprofen? Quiet pop-up - maybe not even a block.
This isn’t just tech. It’s a cultural shift. We’re moving from blanket warnings to smart, personalized alerts.
Bottom Line: Don’t Ignore the Alert - But Don’t Believe It Blindly
Pharmacy allergy alerts are a tool. Not a rule. They’re better than nothing. But they’re far from perfect. They were built on outdated science and poor documentation. And they’ve created a system where safe drugs are denied, and dangerous ones are overlooked because we’ve stopped listening.
If you’ve been told you’re allergic to a drug, ask: How do I know? If you’ve never been tested, you might not be allergic at all. And if you’ve taken the drug since the alert was added - and you’re fine - that’s proof.
Speak up. Update your records. Ask for testing. You’re not just a patient in a system. You’re the person who knows your body best. And that’s the most important data point of all.




brooke wright
I got flagged for a penicillin allergy in 2018 after a rash from amoxicillin at 12. Turned out it was just heat rash from running a fever. Took cefdinir last year for a sinus infection-no problem. Why do systems still treat every rash like a death sentence? I had to fight my PCP for 3 months just to get it removed.
evelyn wellding
YAS THIS!! 🙌 I used to panic every time I got a red alert, but now I just say ‘nah, I’ve taken this 4 times’ and laugh while the pharmacist sighs. My doc finally updated my chart after I showed them my old prescriptions. We’re not all allergic to everything, people 😘
Chelsea Harton
allergy my ass. its just a computer thing. they dont even know what a rash is. lol
Corey Chrisinger
It’s wild how we’ve outsourced medical judgment to algorithms that don’t know the difference between nausea and anaphylaxis. We treat software like it’s infallible, but the data feeding it? Garbage in, garbage out. The real issue isn’t the alert-it’s the culture of compliance over critical thinking. 🤔
Bianca Leonhardt
People who say they’re ‘allergic’ to penicillin because they got a stomach ache at age 6 are the reason this system is broken. Stop being dramatic. Your ‘allergy’ is a bad memory and bad documentation. If you don’t know the difference between side effects and immune responses, don’t blame the pharmacy.
Travis Craw
My grandma had a red alert for penicillin for 40 years. Turned out she just threw up once in 1972 because the pill was expired. Took her 3 visits to get it fixed. I’m glad someone finally wrote this. Maybe now my mom will stop arguing with the pharmacist every time she gets a script.
Christina Bilotti
Oh sweetie, you wrote an entire essay on why people can’t read. The system isn’t broken-it’s just surrounded by humans who think ‘I felt weird once’ qualifies as a medical diagnosis. Maybe if people stopped treating their childhood tummy ache like a trauma, we wouldn’t need machine learning to fix the mess they made.
Cheryl Griffith
I used to be the person who just clicked ‘OK’ on every alert. Then my sister had a real anaphylactic reaction to a drug they thought was ‘safe’ because the system downgraded her alert. I cried for days. Now I ask every pharmacist: ‘Is this a true allergy or a class alert?’ It’s not just about me-it’s about making sure the system still works when it really matters.
Nick Cole
My cousin got penicillin skin tested last year. Took 20 minutes. No reaction. Her chart got updated. Now she can take amoxicillin again. Why isn’t this standard? Why do we still treat this like a secret handshake with the doctor? It’s simple. Ask. Get tested. Update. Done.
vivek kumar
In India, we rarely have these alerts. Doctors rely on patient history, not software. But when I came to the US, I was shocked how often safe drugs are denied because of vague labels. The real solution isn’t better AI-it’s better education. Patients need to understand what an allergy is, not just what the system says.
Bobbi-Marie Nova
LOL I once told my pharmacist I had a ‘penicillin allergy’ because my mom said so. Turned out I’d taken it three times since then with zero issues. She looked at me like I’d just admitted to stealing her coffee. Now I just say ‘I’m not allergic, but I’m weirdly bad at remembering what I ate in 2003.’ 😅