When someone with idiopathic pulmonary fibrosis (IPF) suddenly gets worse-breathing harder, coughing more, oxygen levels dropping-it’s not just a bad day. It’s an acute exacerbation. These events can happen without warning, often lead to hospitalization, and carry a high risk of death. For years, doctors had almost nothing to offer beyond supportive care. Then came pirfenidone. Not a cure. Not a miracle. But a real, measurable tool that’s changing outcomes for people facing this brutal disease.
What Exactly Is an Acute Exacerbation of IPF?
Idiopathic pulmonary fibrosis is a progressive lung disease where scar tissue slowly builds up in the lungs, making it harder to breathe. It’s not caused by smoking, infection, or toxins-it just happens. Acute exacerbations are sudden, severe worsening episodes. No clear trigger. No infection. No heart failure. Just a rapid decline in lung function, often within days.
Studies show that about 5% to 15% of people with IPF have at least one acute exacerbation over five years. And when it happens, half of those patients die within three months. The median survival after an exacerbation is just 3 to 4 months. That’s why even small improvements in preventing or managing these events matter so much.
How Pirfenidone Works in IPF
Pirfenidone is an antifibrotic and anti-inflammatory drug. It doesn’t reverse existing scarring, but it slows down the process that causes more of it. It works by blocking key signaling molecules-like TGF-beta and TNF-alpha-that tell the body to make excess collagen and scar tissue in the lungs.
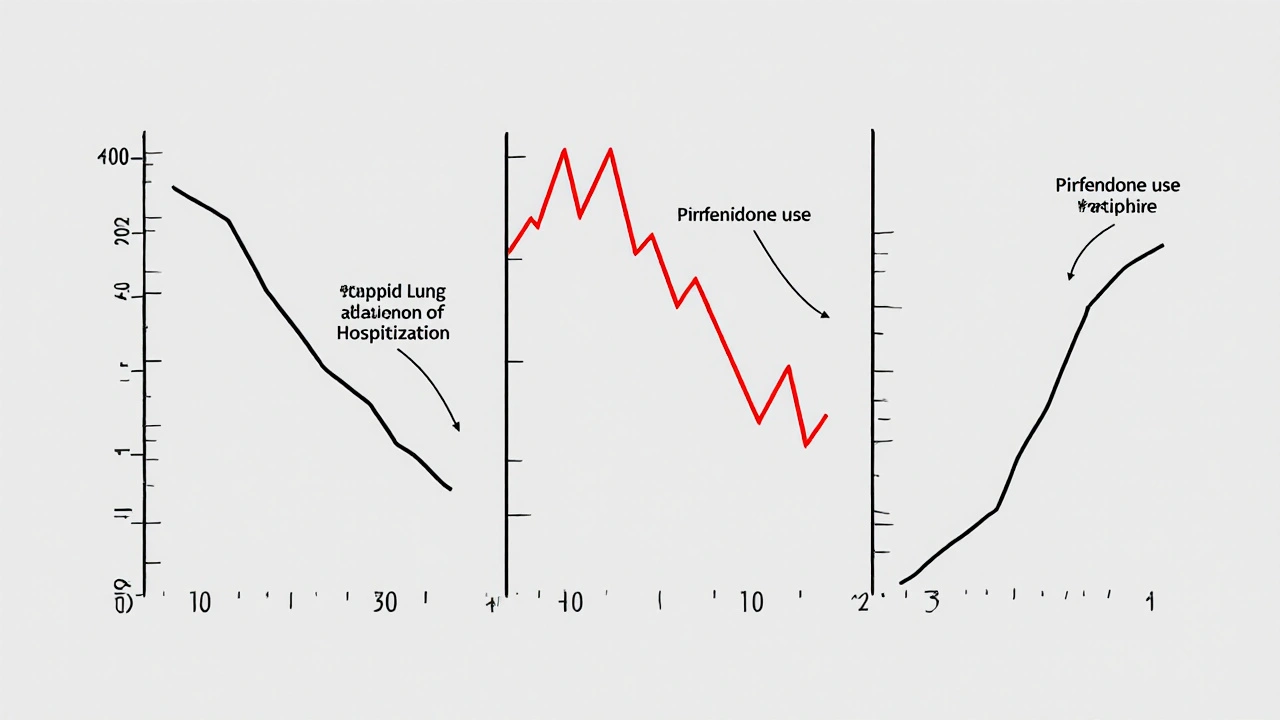
In clinical trials, people taking pirfenidone had a 30% to 40% lower rate of lung function decline over a year compared to those on placebo. That’s not just a statistic-it means more days breathing without oxygen, more time walking the dog, more nights sleeping through the night.
Pirfenidone and Acute Exacerbations: What the Evidence Shows
For years, experts assumed pirfenidone only helped with long-term decline. Then came the pooled analysis of three major Phase 3 trials-CAPACITY and ASCEND-published in the European Respiratory Journal in 2019. The results were striking: patients taking pirfenidone had a 46% lower risk of experiencing an acute exacerbation over 72 weeks compared to those on placebo.
Another study from Japan, tracking over 800 patients for three years, found that those on pirfenidone had fewer hospitalizations due to exacerbations. Their time to next event was longer. Their survival after an exacerbation was better. The effect wasn’t huge for everyone-but for those who responded, it was life-changing.
Why does this happen? Researchers think pirfenidone stabilizes the lung environment. By reducing inflammation and fibrosis activity, it makes the lungs less likely to tip into a runaway collapse during stress-whether from a cold, a clot, or just unknown triggers.

Who Benefits Most From Pirfenidone?
Not everyone with IPF responds the same way. Pirfenidone works best in people with mild to moderate disease-those with forced vital capacity (FVC) between 50% and 90% of predicted. It’s less effective if the lungs are already severely scarred.
It’s also more effective when started early. Waiting until after the first exacerbation means you’ve already lost ground. Guidelines from the American Thoracic Society and European Respiratory Society now recommend starting pirfenidone as soon as IPF is diagnosed, even if symptoms feel mild.
Patients with higher baseline levels of certain biomarkers-like KL-6 and SP-D-also seem to respond better. These are blood markers linked to lung injury and fibrosis activity. Doctors don’t test them routinely yet, but they’re becoming more common in specialized clinics.
Side Effects and Real-World Challenges
Pirfenidone isn’t easy to take. About 30% of people stop because of side effects. The most common: nausea, loss of appetite, dizziness, and skin rashes. Sun sensitivity is a big one-you can get burned easily, even on cloudy days. That’s why patients are told to wear hats, long sleeves, and high-SPF sunscreen every single day.
Most side effects get better after the first few months. Doctors usually start with a low dose and ramp up slowly over three weeks. Many patients need to take it with food to reduce stomach upset. Some switch to generic versions to cut costs-pirfenidone is expensive, often over $10,000 a year in the U.S., though prices vary by country.
In Australia, it’s covered by the PBS (Pharmaceutical Benefits Scheme) for eligible patients with confirmed IPF. That makes it affordable for most, but access still depends on specialist referral and lung function testing.
How It Compares to Other Treatments
The only other approved antifibrotic drug for IPF is nintedanib. Both drugs slow decline and reduce exacerbation risk. Direct comparisons are limited, but a 2022 meta-analysis found they’re about equally effective. The main difference? Side effect profiles.
Nintedanib causes more diarrhea. Pirfenidone causes more skin reactions and nausea. Some patients tolerate one better than the other. A few doctors even switch patients from one to the other if side effects are unbearable.
There’s no evidence that combining them helps more than using one alone-and the side effects stack up. So most guidelines stick to monotherapy.
Other treatments-like corticosteroids, immunosuppressants, or antibiotics-are sometimes tried during an acute exacerbation. But studies show they don’t improve survival. In fact, steroids may increase the risk of infection without helping lung recovery.
What Patients Should Know Before Starting
If you’ve been diagnosed with IPF, ask your doctor about pirfenidone. Don’t wait. Start early. Stick with it. Even if you feel fine now, the damage is still happening.
Be ready for side effects. Talk to your pharmacist about timing doses with meals. Use sunscreen religiously. Keep a symptom diary-note your oxygen levels, breathing effort, and any rashes. That info helps your doctor adjust your dose or catch problems early.
And if you do have an acute exacerbation? Don’t panic. Get to a hospital fast. Pirfenidone doesn’t stop all exacerbations-but if you’ve been taking it, your chances of surviving one are better than if you hadn’t.
Looking Ahead: What’s Next for Pirfenidone?
Researchers are now studying pirfenidone in combination with other drugs-like anticoagulants or anti-inflammatory agents-to see if they can boost its effect. Early trials are promising, but nothing’s approved yet.
There’s also growing interest in using pirfenidone for other fibrotic lung diseases-like those linked to connective tissue disorders or chronic hypersensitivity pneumonitis. Early data suggests it might help there too.
But for now, its clearest role remains in IPF. Not as a cure. Not as a magic bullet. But as the best tool we have to slow the fall-and give people more time with the people they love.
Can pirfenidone reverse lung scarring in IPF?
No, pirfenidone cannot reverse existing scar tissue in the lungs. It works by slowing down the production of new scar tissue. This helps preserve lung function over time, but it doesn’t undo damage that’s already there. That’s why starting treatment early is so important.
How long does it take for pirfenidone to start working?
Pirfenidone doesn’t give immediate results. Most patients don’t feel better right away. The benefits show up over months-not days. Lung function tests, like FVC and DLCO, are the best way to track progress. Doctors usually wait 6 to 12 months to see if the drug is slowing decline.
Is pirfenidone safe to take with other medications?
Pirfenidone is metabolized by the liver, so it can interact with drugs that affect liver enzymes-like certain antibiotics, antifungals, or seizure medications. Always tell your doctor about every pill, supplement, or herb you’re taking. They may need to adjust doses or monitor liver enzymes more closely.
Can I stop taking pirfenidone if I feel better?
No. IPF is a progressive disease, and pirfenidone works by slowing that progression. Stopping the drug-even if you feel fine-lets the scarring process resume. Clinical trials show that patients who stop taking pirfenidone decline faster than those who continue. It’s a long-term treatment, not a short-term fix.
What should I do if I miss a dose of pirfenidone?
If you miss a dose, skip it and take your next dose at the regular time. Don’t double up to make up for it. Taking too much at once can increase side effects like nausea or dizziness. Consistency matters more than perfect timing-try to take it with meals at the same times each day.



Sierra Thompson
Pirfenidone doesn't fix the broken system. It just makes the decline slower. We're treating symptoms of a system that lets people wait years for diagnosis while their lungs turn to stone. The real tragedy isn't the disease-it's the healthcare inertia that lets it get this far before we even try to help.
They call it a miracle drug. I call it a Band-Aid on a hemorrhage.
Khaled El-Sawaf
While the clinical data presented is statistically significant, one must consider the economic and ethical implications of prescribing pirfenidone in a healthcare system where access is dictated by insurance status. The 46% reduction in exacerbation risk is meaningless if 30% of patients discontinue due to cost or side effects. This is not medicine-it's privilege masquerading as treatment.
Let us not mistake palliation for progress.
Nawal Albakri
they say pirfenidone helps but what if the real cause is 5g radiation from cell towers and chemtrails? i read a guy on reddit who got ipf after living near a 5g tower for 2 years. the drug just masks it. they dont want you to know the truth. why do you think its so expensive? because they dont want you to get it from india or china. the pharma giants are scared. they know this is a coverup. my cousin died from ipf and they told her it was 'idiopathic'-but she never smoked, never worked in a factory. she just used her phone too much.
ask your doctor about the real cause. theyll lie to you.
theyre watching.
Megan Oftedal
Hi! I just wanted to say I found this super helpful-my dad has IPF and we’re thinking about starting him on pirfenidone. I had no idea about the sun sensitivity thing, that’s wild. We’ve been using SPF 70 and hats nonstop since he started. He still gets rashes though, poor guy. Any tips on managing nausea? We’ve tried ginger tea and it kinda helps, but not always.
Also, is generic really as good? We’re in Texas and the copay is insane.
Musa Aminu
Y’all in the West act like this is some new miracle. In Nigeria, we don’t even have access to basic oxygen tanks, let alone $10k pills. You talk about survival rates like it’s a video game stat. Meanwhile, African patients are dying in silence because they can’t even get a CT scan. This isn’t science-it’s a luxury for the rich. Pirfenidone? More like pirfenidone-for-the-rich-while-the-poor-die.
Stop celebrating medicine that only helps those who can afford to be sick.
robert maisha
The data shows pirfenidone reduces exacerbation risk by nearly half yet we still treat it as if it were a last resort. Why do we wait until the lungs are half gone before we act? Why is early intervention not standard practice across all clinics? The science is clear. The delay is moral. We have tools. We choose not to use them until it is too late. This is not negligence. It is complicity.
And yet we call ourselves healers
Alexander Ståhlberg
Let’s be real here. Pirfenidone isn’t a cure. It’s a pause button. And we’re all pretending that pausing the inevitable is somehow heroic. The truth? We’re just buying time so people can die slower, surrounded by more machines, more bills, more fear. The drug doesn’t give you more life-it gives you more time to grieve the life you’re losing.
And don’t get me started on the side effects. You take this pill and suddenly you’re afraid of sunlight, afraid of food, afraid of your own body. It’s not treatment. It’s a slow, expensive, sunburned surrender.
But hey-at least you’re not dead yet. Right?
Robert Andersen
My dad’s been on it for 18 months. He doesn’t feel different. But his FVC held steady when his buddy’s dropped 15% in six months. So yeah, it’s not magic. But if it keeps you breathing just a little longer so you can hear your grandkid laugh? Worth every nausea-ridden morning.
Just take the damn pill. And wear the hat.