Combination Therapy Risk Calculator
Check Your Risk
Based on your lab values and medication regimen. Results help you discuss risks with your doctor.
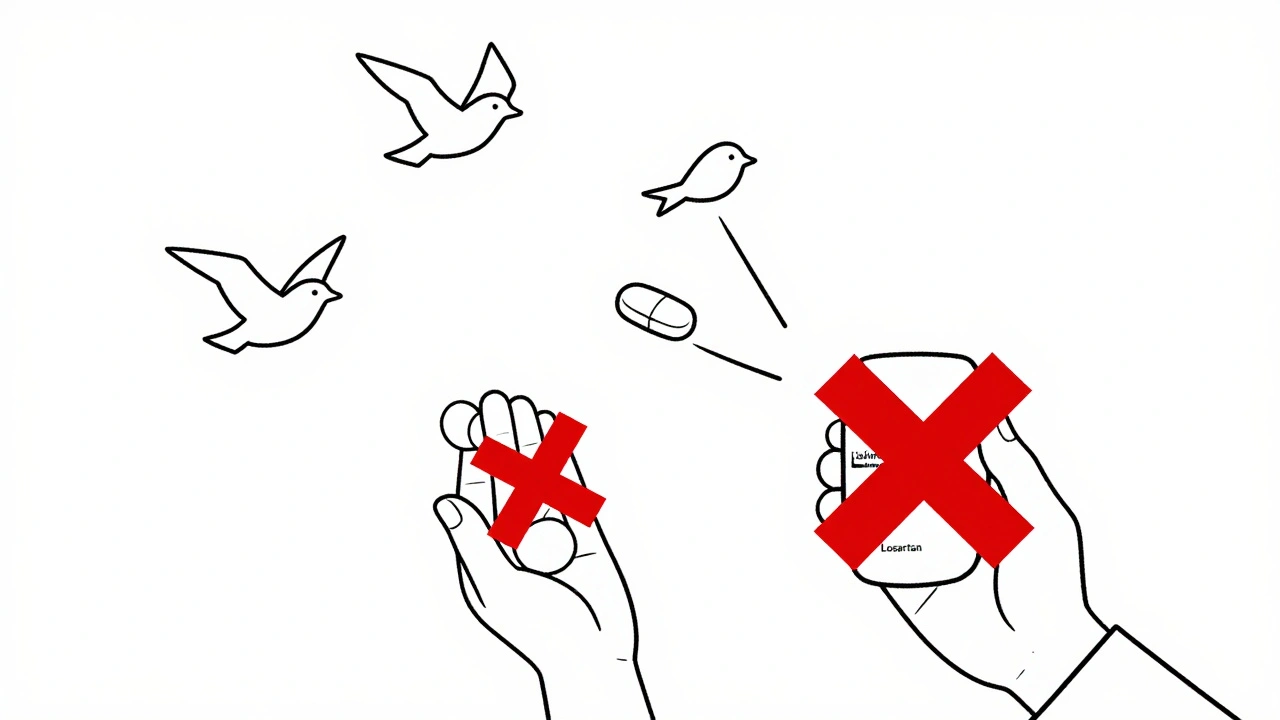
When your doctor prescribes an ACE inhibitor or an ARB for high blood pressure, heart failure, or kidney protection, you’re getting one of the most studied and effective classes of heart meds available. But here’s the thing: ACE inhibitors and ARBs aren’t interchangeable, and mixing them can be dangerous-even if it seems like doubling down should help more.
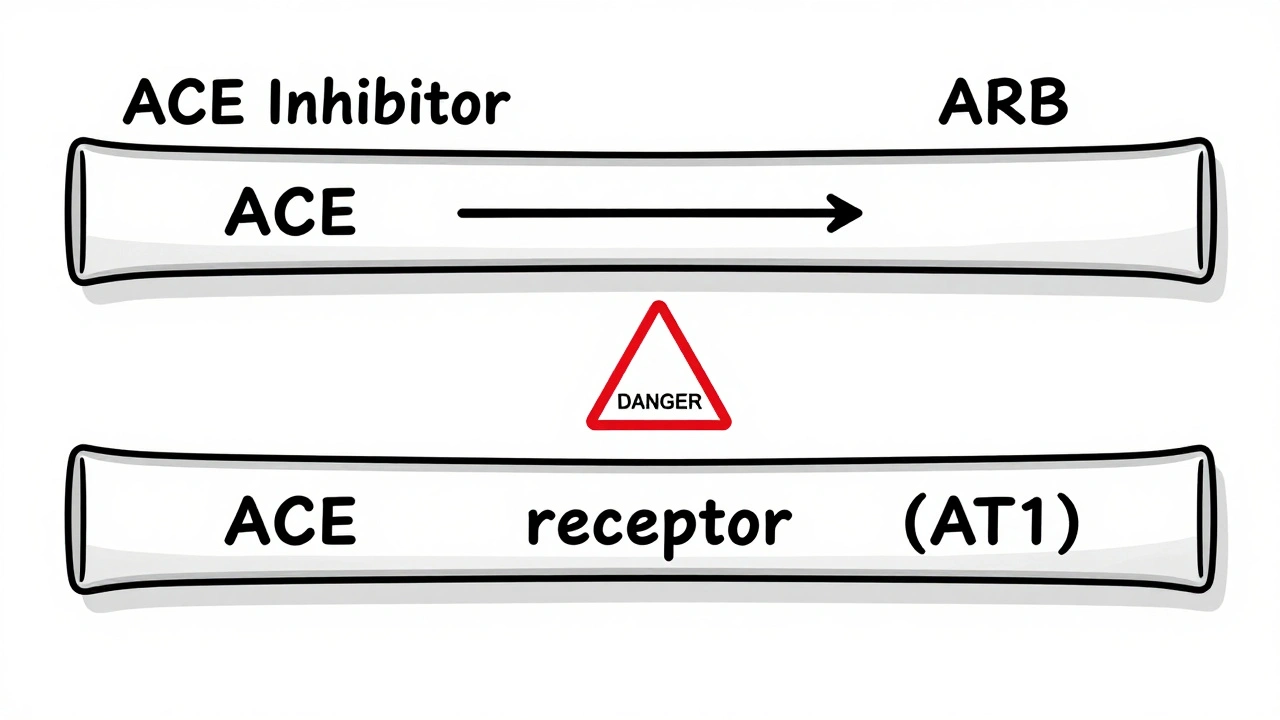
How ACE Inhibitors and ARBs Work (And Why It Matters)
Both ACE inhibitors and ARBs target the same system in your body-the renin-angiotensin system (RAS)-but they hit different spots. ACE inhibitors like lisinopril and enalapril block the enzyme that turns angiotensin I into angiotensin II, the molecule that tightens blood vessels and raises blood pressure. ARBs like losartan and valsartan don’t stop angiotensin II from being made; they just block its receptors so it can’t do its job.
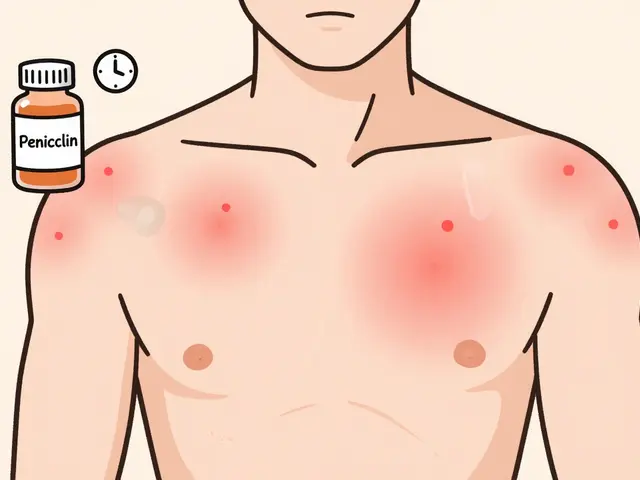
This small difference has big consequences. ACE inhibitors cause bradykinin to build up, which is why about 1 in 10 people on these drugs get a dry, annoying cough. ARBs don’t do that. That’s why if you can’t tolerate an ACE inhibitor, your doctor will switch you to an ARB-not add it.
And here’s something most people don’t realize: even if your ACE inhibitor seems to stop working after a few months, it’s not because your body got used to it. It’s because your body found another way to make angiotensin II. About two-thirds of long-term users experience this ‘escape effect,’ where angiotensin II levels bounce back up by 25-30%. That’s why some patients need higher doses or different meds-not more RAS blockers.
The Real Risk: Combining ACE Inhibitors and ARBs
It’s tempting. If one drug lowers blood pressure, two must be better, right? Wrong. Multiple large studies-like the ONTARGET trial and the VA NEPHRON-D trial-showed that combining an ACE inhibitor with an ARB doesn’t save lives, doesn’t prevent heart attacks, and doesn’t slow kidney disease any better than one drug alone.
But it does make you sicker.
Here’s what happens when you mix them:
- Hyperkalemia (high potassium): Your potassium level jumps by an average of 0.8 mmol/L. Normal is 3.5-5.0. Above 5.5, you risk dangerous heart rhythms. In studies, the risk of dangerous hyperkalemia doubled-from 5% to 10%.
- Acute kidney injury: Your kidneys can’t handle the double hit. Risk goes up by 80%. In diabetic patients, this can mean sudden dialysis.
- Low blood pressure and fainting: You’re more likely to feel dizzy, fall, or end up in the ER.
The FDA and major guidelines from the American Heart Association, the American College of Cardiology, and the European Society of Cardiology all say: Don’t combine them. Not for hypertension. Not for kidney disease. Not unless you’re in a research study-and even then, only under strict supervision.
When Might a Doctor Still Consider It?
There’s one tiny gray area: non-diabetic kidney disease with heavy proteinuria (over 1 gram per day) that doesn’t respond to maximum ACE inhibitor doses. A handful of nephrologists, like Dr. Srinivasan Beddhu, have reported cases where adding an ARB cut protein loss by 40-60%. But these are rare. And they come with a catch.
If you’re one of those rare cases, you’ll need weekly blood tests for potassium and kidney function. You’ll need to avoid salt substitutes, potassium-rich foods like bananas and spinach, and NSAIDs like ibuprofen. And you’ll need to stop the combo immediately if your creatinine rises more than 30% or your potassium hits 5.5.
Even then, most doctors won’t do it. A 2023 survey of 317 primary care doctors found only 11% still used the combo-and only in patients they monitored monthly. The rest stopped after the VA NEPHRON-D trial showed 27% more serious side effects with no benefit.
What to Do Instead
If your blood pressure isn’t controlled on an ACE inhibitor or ARB, here’s what actually works:
- Add a diuretic: Hydrochlorothiazide or chlorthalidone helps flush out extra fluid and sodium. This is the most common next step.
- Add a calcium channel blocker: Amlodipine is often paired with RAS blockers and works well together.
- Switch to an ARNI: Sacubitril/valsartan (Entresto) is now first-line for heart failure with reduced ejection fraction. It combines an ARB with a neprilysin inhibitor and has better outcomes than ACE inhibitors alone.
- Add a mineralocorticoid receptor antagonist: Spironolactone or eplerenone can reduce proteinuria by 30-40% without the hyperkalemia risk of ARB+ACE combos.
One big mistake I see? Doctors switch from an ACE inhibitor to an ARB and start the new drug the next day. That’s risky. The drugs linger in your system. The American College of Cardiology recommends a 4-week washout period before switching. Only 42% of prescribers follow this, according to a 2022 JAMA study. If you’re switching, ask your doctor about this.
Side Effects: ACE Inhibitors vs. ARBs
Both can raise potassium and hurt kidney function, especially if you’re older, have diabetes, or already have kidney disease. But their side effect profiles are very different.
| Side Effect | ACE Inhibitors | ARBs |
|---|---|---|
| Dry cough | 10-15% | 3-5% |
| Angioedema (swelling) | 0.1-0.7% | 0.1-0.2% |
| Hyperkalemia | 5-8% | 4-7% |
| Acute kidney injury | 5-8% | 4-7% |
| Discontinuation due to side effects | Higher | Lower (1.8% fewer) |
That 1.8% difference in discontinuation might not sound like much, but over 4 years, it means 1 in every 55 patients avoids a side effect serious enough to quit the drug. That’s meaningful.
Monitoring: What You Need to Watch
Whether you’re on an ACE inhibitor or ARB, you need regular blood tests. Here’s the standard schedule:
- Check potassium and creatinine 1-2 weeks after starting or changing dose.
- If stable, repeat every 3 months.
- If you have diabetes or kidney disease, check every 2 months.
- If you’re sick, dehydrated, or start a new med (like NSAIDs), check immediately.
And don’t ignore symptoms: unusual fatigue, muscle weakness, irregular heartbeat, or swelling in your legs could mean your potassium is too high. Call your doctor right away.
Market Trends and New Developments
In 2023, ACE inhibitors were still the most prescribed RAS blockers in the U.S.-over 32 million prescriptions, led by lisinopril. ARBs came in second at 23.6 million, with losartan as the top choice. But the trend is shifting. More patients are being switched to ARBs because of the cough issue.
There’s also been progress in safety. Between 2018 and 2020, several ARBs were recalled due to cancer-causing impurities. That’s mostly fixed now. New manufacturing standards have restored confidence.
And the future? The FINE-REWIND trial is testing ultra-low-dose combinations in diabetic kidney disease, with results expected in 2026. But don’t hold your breath-analysts predict less than 1% of prescriptions will ever involve this combo. The real winners are newer drugs like ARNIs and SGLT2 inhibitors, which are now preferred for heart and kidney protection.
Bottom Line
ACE inhibitors and ARBs are powerful tools. But they’re not meant to be used together. The added blood pressure drop isn’t worth the risk of kidney failure or life-threatening high potassium. If your current med isn’t working, talk to your doctor about adding a diuretic, switching to an ARNI, or using a mineralocorticoid blocker-not another RAS drug.
And if you’re on both? Ask your doctor why. Most of the time, it’s an accident from years ago. It’s not too late to stop.



nina nakamura
ACEi and ARB combos are a lazy hack. If your BP isn't controlled, it's not because you need more RAS blockade-it's because you're not doing the basics. Salt intake, weight, sleep, stress. Fix those first. No one wants to hear it but most hypertensives are just bad at lifestyle. The meds are bandaids on a leaking pipe.
And yes, I've seen 70-year-olds on both get dialyzed after a weekend of ibuprofen and bananas. Don't be that person.
Hamza Laassili
WHAT THE ACTUAL F***. I WAS ON LISINOPRIL AND MY DOCTOR JUST SWITCHED ME TO LOSARTAN AND NOW I'M NOT COUGHING LIKE A TUBERCULOSIS PATIENT??!! THANK GOD. BUT WAIT-SO WE CAN'T JUST TAKE BOTH?? I THOUGHT DOCTORS KNEW WHAT THEY WERE DOING??!!
MY GRANDPA WAS ON BOTH FOR 5 YEARS AND HE'S FINE?? WHAT'S THE DEAL?? I'M CONFUSED AND NOW I'M SCARED TO TAKE ANYTHING.
AND WHY THE HELL DO WE NEED TO WAIT 4 WEEKS TO SWITCH?? THAT'S INSANE. I'M JUST GONNA STICK WITH WHAT WORKS.
PS: I'M NOT A DOCTOR BUT I READ THE INTERNET AND THIS POST MADE ME REGRET EVERYTHING.
Rawlson King
The VA NEPHRON-D trial remains the definitive evidence against dual RAS blockade. The lack of mortality benefit coupled with a 27% increase in serious adverse events renders the combination clinically indefensible outside of highly selected, closely monitored research cohorts. The persistence of this practice in primary care reflects systemic failures in continuing medical education and pharmaceutical marketing influence. Nephrologists who still prescribe this combo without stringent monitoring are practicing outdated, high-risk medicine.
And yes, the 1.8% reduction in discontinuation with ARBs over ACE inhibitors is statistically significant and clinically meaningful over a population level. This is not trivial.
Constantine Vigderman
YESSSSS this is so important!! I had a friend who was on both and ended up in the ER with potassium at 6.2 😱
But here’s the good news-switching to spironolactone + amlodipine changed his life!! No more dizziness, no more scary blood tests, and his proteinuria dropped like a rock!!
Also-try cutting out salt substitutes! They’re basically potassium bombs. I didn’t know that until my kidney doc told me.
And if you’re switching from ACE to ARB? DO THE 4-WEEK WASHOUT. Seriously. Your kidneys will thank you. 💪❤️
YOU GOT THIS. YOU’RE NOT ALONE. LET’S MAKE HEALTH SMARTER TOGETHER!!
Cole Newman
Wait so if I'm on lisinopril and I get a cough, I just switch to losartan? No big deal? No blood tests? No waiting? My doc just switched me last week and I'm fine.
Why is everyone making this so complicated? I don't need a 15-page essay to know if my BP is down and I'm not coughing, I'm good.
And why are you people obsessed with potassium? I eat bananas every day and I'm 32. I'm not dying.
Also, why do doctors even prescribe these if they're so dangerous? Just give me a beta blocker and be done with it.
Casey Mellish
As an Aussie who’s seen the RAS blockade debate play out in both public and private healthcare systems, I can confirm: the evidence is crystal clear. Dual therapy is not just ineffective-it’s actively harmful. The Australian Heart Foundation updated its guidelines in 2022 to explicitly prohibit combination use outside of clinical trials.
What’s interesting is how the US still lags behind in adoption of ARNIs and SGLT2 inhibitors despite superior outcomes. We’ve had them on PBS since 2020. If you’re still reaching for a second RAS blocker, you’re not being proactive-you’re being reactive.
And yes, the 4-week washout? Non-negotiable. I’ve seen patients on both end up in ICU because their GP thought ‘it’s just a switch.’ It’s not.
Tyrone Marshall
There’s a quiet tragedy here: people aren’t being taught how to think about their meds, they’re just being given them.
Doctors prescribe ACE inhibitors because they’re cheap, familiar, and covered. Patients take them because they trust the system. But no one talks about the slow erosion of kidney function, the silent rise in potassium, the way our bodies adapt and rebel.
It’s not about blaming doctors or patients. It’s about creating systems that honor complexity. A pill isn’t a solution-it’s a tool. And tools need context.
If your blood pressure is high, ask: What’s my diet? My stress? My sleep? My movement? The RAS system is just one lever. Don’t pull all of them at once.
And if you’re on both? You’re not broken. You’re just part of a system that didn’t catch up. You deserve better. You deserve to be heard. You deserve to be safe.
It’s never too late to ask the right question.