Drug Rash Severity Checker
This tool helps you assess whether your skin reaction might be an emergency. Remember: This is not a diagnosis tool but a guide based on the article content.
Symptoms Assessment
Select all symptoms you're experiencing
Have you ever broken out in a rash after starting a new pill, antibiotic, or painkiller? You’re not alone. About 2-5% of people who take medications develop some kind of skin reaction - and most don’t realize it’s linked to what they’re taking. These aren’t just annoying spots. Some rashes are mild and go away on their own. Others can be life-threatening. Knowing the difference could save your life.
What Does a Drug Rash Look Like?
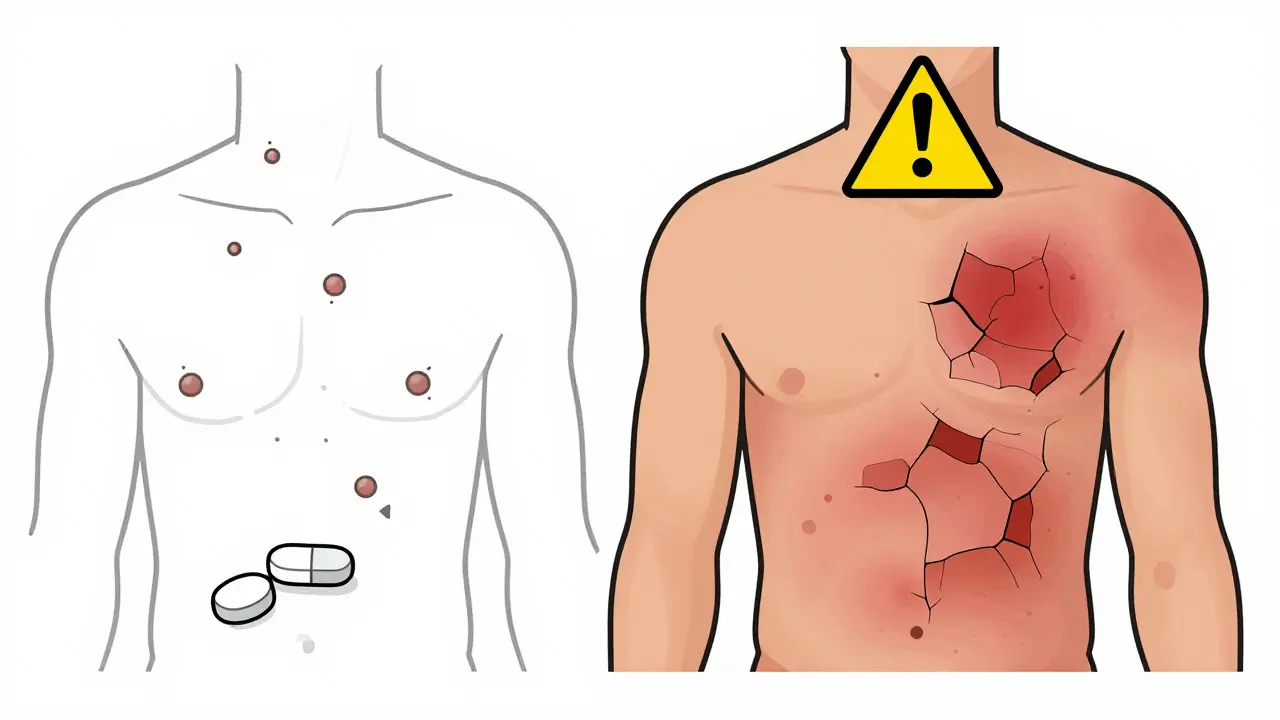
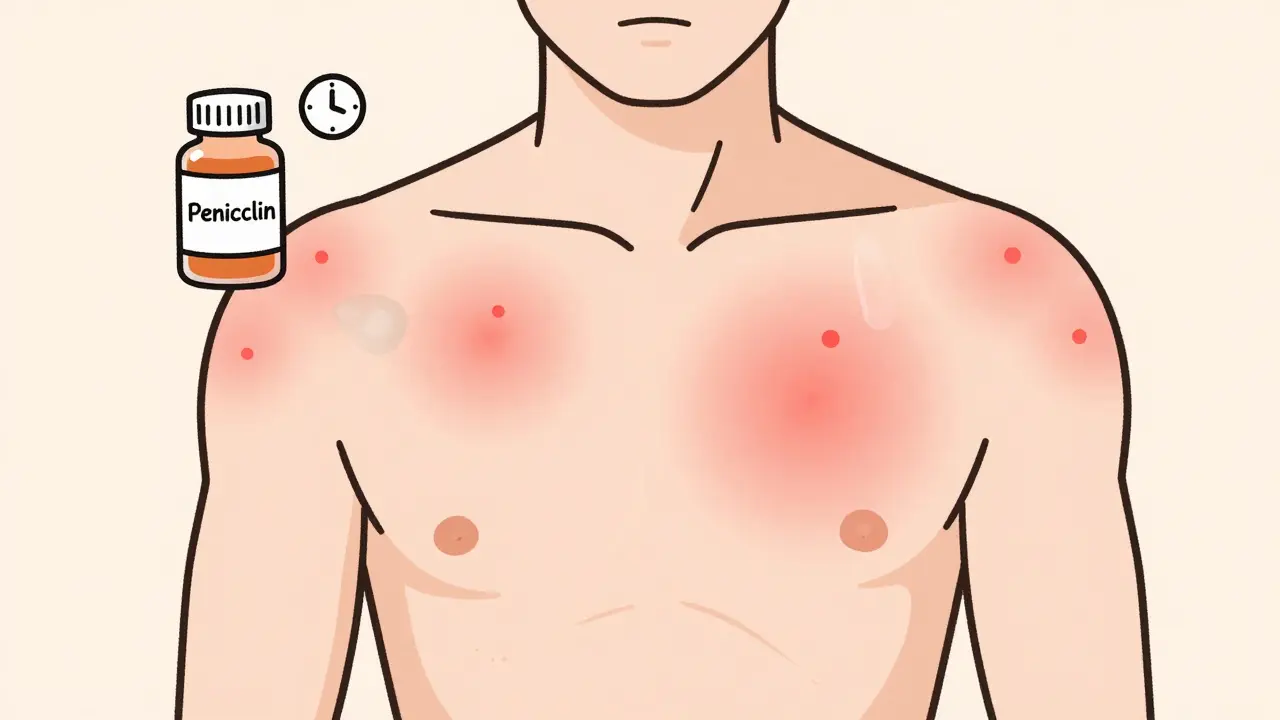
Not all skin reactions are the same. The most common type, called a morbilliform or maculopapular rash, looks like small red bumps or flat spots that spread symmetrically. It usually shows up on the chest, back, or upper arms, sometimes with a low fever. This happens in about 90-95% of all drug rashes and is often caused by antibiotics like penicillin or sulfa drugs. It typically appears 4 to 14 days after starting the medication - but sometimes not until you’ve stopped it. Then there’s urticaria, or hives. These are raised, itchy welts that come and go within hours. If you get hives after taking ibuprofen or naproxen, it’s likely a non-allergic reaction. They usually fade within 24 to 48 hours after stopping the drug. More serious patterns include:- Nummular dermatitis: Coin-shaped, dry, scaly patches that look like eczema. These can be mistaken for atopic dermatitis - up to 40% of cases are misdiagnosed.
- DRESS syndrome: A delayed reaction that starts 2 to 6 weeks after taking certain drugs. It causes a widespread rash, fever, swollen lymph nodes, and organ inflammation. It’s linked to antiseizure meds like carbamazepine, allopurinol, and some antibiotics.
- Stevens-Johnson Syndrome (SJS) or Toxic Epidermal Necrolysis (TEN): These are medical emergencies. The skin blisters, peels, and looks like a severe burn. Mucous membranes in the mouth, eyes, or genitals may also break down. SJS has a 5-15% death rate; TEN is even deadlier at 25-35%.
Why Do Medications Cause Skin Reactions?
There are two main ways drugs trigger rashes: allergic and non-allergic. Allergic reactions happen when your immune system mistakes the drug for a threat. It releases histamine and other chemicals, causing itching, swelling, or hives. Penicillin is the most common offender here - responsible for 80% of severe allergic drug reactions. Other frequent culprits include sulfa drugs, anticonvulsants, and chemotherapy agents. Non-allergic reactions are trickier. Your body doesn’t treat the drug like an invader, but it still reacts. Aspirin, radiocontrast dye (used in CT scans), and opiates can cause symptoms that look like allergies - but without the immune system involvement. These reactions are often dose-related and can occur even on the first use. One surprising fact: you might not even know you were exposed to a drug before. Trace amounts in food or contaminated water can sensitize your immune system without you realizing it. That’s why a rash can appear suddenly - even if you’ve taken the same medicine before without issues.Who’s at Higher Risk?
Some people are much more likely to develop drug rashes:- People on five or more medications: Your risk jumps to 35% over your lifetime. This is why older adults and those with chronic conditions are most affected.
- People with viral infections: If you’re fighting Epstein-Barr virus (mononucleosis) or HIV and take antibiotics like amoxicillin, your chance of a severe rash increases by 5 to 10 times.
- Those with weakened immune systems: Cancer patients or those on immunosuppressants have a 3 to 5 times higher risk.
- People with certain genes: HLA-B*1502 gene carriers in Southeast Asia have a 1,000-fold higher risk of SJS from carbamazepine. HLA-B*5801 in Han Chinese populations increases allopurinol-related SCAR risk by 580-fold.
What Should You Do If You Get a Rash?
Don’t panic - but don’t ignore it either. If you notice a rash after starting a new drug:- Don’t stop the medication on your own. Especially if it’s for seizures, high blood pressure, or heart disease. Stopping suddenly can be dangerous.
- Call your doctor. Take a photo of the rash. Note when it started, what you’ve been taking, and whether you have other symptoms like fever, swelling, or trouble breathing.
- Watch for red flags. Go to the ER immediately if you have:
- Blisters or peeling skin
- Swelling of the face, lips, or tongue
- Difficulty breathing or swallowing
- Sores in your mouth, eyes, or genitals
- Lukewarm baths with fragrance-free cleansers
- Applying fragrance-free moisturizer within 3 minutes of bathing
- Over-the-counter 1% hydrocortisone cream twice daily
- Antihistamines like cetirizine or loratadine for itching
Can You Be Tested for Drug Allergies?
Yes - and it’s more accurate than ever. Penicillin skin testing now identifies 95% of true allergies. Many people who think they’re allergic to penicillin aren’t - about 15% of reported allergies turn out to be false. If you’ve been told you’re allergic, ask your doctor about testing. It could open up better treatment options. For other drugs, testing is less reliable. Blood tests for drug allergies aren’t widely available or validated. The best way to confirm a reaction is still careful history, timing, and sometimes a supervised rechallenge under medical supervision.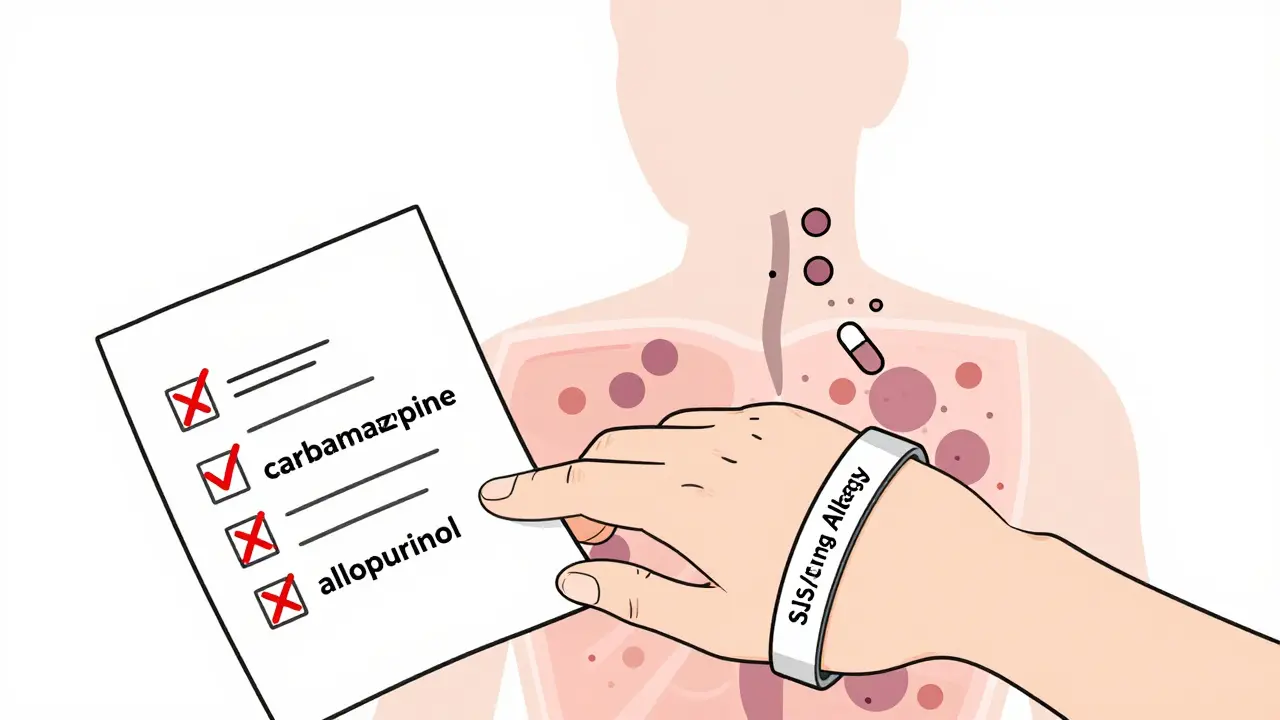
How to Prevent Future Reactions
- Keep a list of all medications you’ve reacted to - including the name, type of rash, and when it happened.
- Wear a medical alert bracelet if you’ve had SJS, DRESS, or a severe anaphylactic reaction.
- Ask your pharmacist if any new prescriptions could interact with drugs you’ve had reactions to.
- Be cautious with photosensitivity. Drugs like doxycycline, ciprofloxacin, and hydrochlorothiazide make your skin sensitive to sunlight. Use sunscreen and cover up - even on cloudy days.
- Limit unnecessary drugs. The more pills you take, the higher your risk. Talk to your doctor about whether every medication is still needed.
The Bottom Line
Most drug rashes aren’t emergencies. About 90% clear up within 1 to 2 weeks after stopping the medication. But that doesn’t mean you should wait. Early recognition is key. The most dangerous reactions - SJS, TEN, DRESS, and AGEP - are rare. They make up less than 2% of all drug rashes, but cause 90% of deaths. If you’re on long-term meds like antiseizure drugs or allopurinol, know the warning signs. Your skin is a mirror. A rash isn’t just a skin problem - it’s your body’s way of saying something’s wrong. Listen to it. Talk to your doctor. And don’t assume you know what’s causing it. Sometimes, the answer isn’t obvious - and that’s why expert help matters.Can a drug rash appear days after stopping the medication?
Yes. Some rashes, especially morbilliform or DRESS-type reactions, can appear 1 to 2 days after stopping the drug. This happens because the immune system continues reacting even after the drug is cleared from your system. It’s not unusual for a rash to peak after discontinuation, so don’t assume the drug is harmless just because you stopped taking it.
Is a drug rash always an allergy?
No. Only about 15% of drug rashes are true IgE-mediated allergies. The vast majority - around 85% - are T-cell mediated delayed reactions, meaning your immune system responds slowly without producing classic allergy antibodies. Non-allergic reactions, like those from aspirin or opiates, mimic allergies but don’t involve the immune system at all. The treatment and risk profile differ significantly.
Can I take a drug again if I had a mild rash before?
Generally, no. Even if your rash was mild, re-exposure carries a high risk of a much worse reaction. Your immune system remembers the drug. Doctors strongly advise avoiding any medication that previously caused a rash - unless testing confirms it was not an allergic reaction. For life-saving drugs like antiseizure meds, specialists may perform a controlled rechallenge in a hospital setting.
Are over-the-counter creams safe for drug rashes?
For mild, non-blistering rashes, 1% hydrocortisone cream and moisturizers are usually safe and helpful. But avoid anything with fragrances, lidocaine, or antihistamines in the cream - these can irritate the skin further or even trigger new reactions. If the rash is spreading, blistering, or painful, stop all topical treatments and see a doctor immediately.
Do drug rashes leave scars?
Mild rashes like morbilliform or nummular dermatitis typically don’t scar. But severe reactions like SJS, TEN, or prolonged DRESS can leave permanent changes - including dark spots, thinning skin, or scarring. In extreme cases, patients lose skin integrity and need long-term wound care. Early intervention is the best way to prevent lasting damage.
Can I prevent a drug rash before it starts?
You can reduce your risk. Avoid unnecessary medications. Keep a detailed list of all drugs you’ve taken and any reactions. Ask about genetic testing if you’re of Southeast Asian or Han Chinese descent and prescribed carbamazepine or allopurinol. Stay hydrated, avoid sun exposure if on photosensitizing drugs, and report even minor skin changes to your doctor early. Prevention is always better than treatment.





Virginia Kimball
Okay, I just read this and I’m honestly amazed how much I didn’t know. I thought rashes were just ‘allergies’-turns out it’s way more complex. That bit about DRESS syndrome showing up weeks after stopping meds? Mind blown. I’ve had a weird rash after amoxicillin once and just brushed it off. Maybe I should’ve listened harder to my skin. Thanks for laying this out so clearly-it’s like a survival guide for anyone on meds.
Kapil Verma
This is why India has better healthcare than the West-you people overmedicate and then blame the pill. In my village, we use neem paste and turmeric. No hospital needed. Your system is broken. You take 12 pills a day and then cry when your skin breaks out. Stop poisoning yourselves with chemicals. Natural remedies work better. Always have. Always will.
Michael Page
The notion that the skin is a mirror is poetic but misleading. The skin is not a messenger-it is a casualty. The real signal lies in the immune system’s misinterpretation of molecular structure, not in some metaphysical reflection. To anthropomorphize the dermis as if it has agency is to confuse biology with metaphor. The rash is not speaking-it is signaling. There is a difference.
Sarah Barrett
Very well-structured and informative. I appreciate the breakdown of allergic vs. non-allergic mechanisms-it’s something most patients never get explained in detail. I’ve seen several cases in my practice where patients were misdiagnosed with eczema when it was actually nummular dermatitis from a new antihypertensive. The 40% misdiagnosis stat is alarming. More clinicians need to be aware of this.
Mike Hammer
bro i had a rash after ibuprofen once and thought it was just heat rash. turned out it was hives. took me 3 weeks to figure it out because i kept using it thinking ‘it’s fine, it’s just dry skin.’ now i carry an epipen just in case. also, why is no one talking about how weird it is that we can get allergic to a drug we took 5 years ago? like… how does that even work? my immune system’s got a long memory, i guess.
Daniel Dover
Agreed. The key is early recognition. If it’s not spreading or blistering, monitor. If it is, go now. Simple.
Chiruvella Pardha Krishna
One must consider the ontological weight of pharmaceutical intervention. The body, in its natural state, does not produce rashes. Rashes are the consequence of artificial molecular intrusion. We have become dependent on chemical constructs to regulate what nature once balanced. The skin, in its wisdom, rebels-not out of malice, but out of fidelity to homeostasis. To treat the rash without questioning the drug is to silence the messenger and glorify the weapon.
Charlotte Dacre
So let me get this straight-my body is screaming at me through a rash, but I’m not allowed to stop the pill? Thanks, medicine. I’ll just keep taking my blood pressure med while my arms look like a Jackson Pollock painting. Brilliant strategy. I’m sure the FDA had a long brainstorming session over coffee and donuts for this one.
Erica Banatao Darilag
thank you for this. i had a rash after amoxicillin last year and i was so scared. i didnt know if it was serious. i went to the er and they just gave me benadryl. this article helped me understand so much more. i didnt realize you could be allergic even if you took it before. i’m gonna start keeping a list now. also… typo: i think you meant ‘clobetasol’ not ‘clobetasol’? lol. sorry.