Many of us know the drill: itchy eyes, a runny nose, and constant sneezing when spring or fall comes around. But what if the food you eat could make these symptoms worse? The relationship between seasonal allergies and food sensitivities is a topic that’s gaining a lot of attention. This connection is more common than you might think, and understanding the basics can help you manage both more effectively.
First, let’s talk about what seasonal allergies really are. When plants release pollen, some people's immune systems go into overdrive, mistaking these harmless particles for dangerous invaders. This leads to a range of symptoms that can make everyday life quite uncomfortable.
- Understanding Seasonal Allergies
- Common Food Sensitivities
- The Immune System Connection
- Tips for Managing Symptoms
Understanding Seasonal Allergies
Seasonal allergies, often referred to as hay fever or allergic rhinitis, affect millions of people each year. These allergies are triggered by airborne substances like pollen, which are released by trees, grasses, and weeds during certain times of the year. When these particles enter the body, the immune system mistakenly identifies them as harmful invaders. This misidentification leads to the production of antibodies known as Immunoglobulin E (IgE).
When IgE antibodies react with allergens, they cause the release of histamines and other chemicals from mast cells. This process incites the well-known symptoms of seasonal allergies: sneezing, itching, nasal congestion, and watery eyes. The intensity of these symptoms can vary based on the amount of pollen in the air and an individual’s sensitivity.
It's surprising how many people don't realize the extensive impact of these allergies. According to the Asthma and Allergy Foundation of America, more than 24 million Americans experience seasonal allergic rhinitis, and around six million of those affected are children. The prevalence of these allergies is increasing, likely due to environmental changes, urbanization, and our changing lifestyles.
"Understanding what triggers these allergies is the first step in finding relief,” says Dr. Michael Blaiss, a prominent allergist and clinical professor at the University of Tennessee Health Science Center.
Another important factor to consider is that different plants pollinate at different times of the year. Tree pollen is usually the main culprit in the spring, grass pollen in the summer, and weed pollen in the fall. Knowing which allergen is active can help sufferers take appropriate preventative measures.
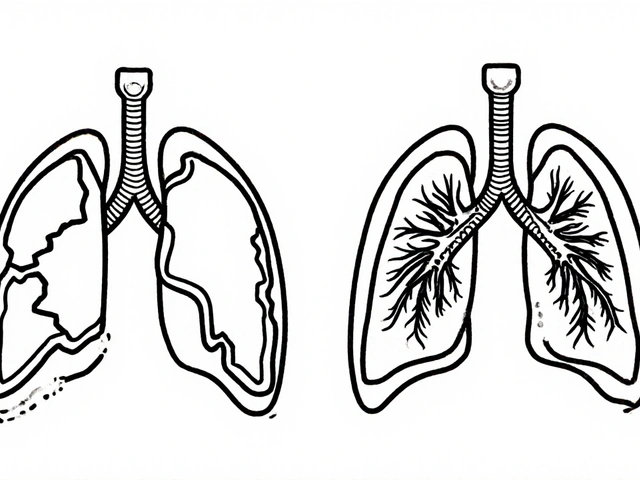
Unfortunately, seasonal allergies can often lead to complications such as sinus infections and can aggravate conditions like asthma. People with asthma, for example, may find their symptoms worsened during pollen seasons, making it crucial for them to monitor air quality and pollen counts actively.
Allergy testing can be a helpful tool in managing seasonal allergies. Tests can identify specific allergens causing problems, enabling targeted treatment approaches. Common testing methods include skin prick tests and specific IgE blood tests, which can determine sensitivities to various allergens.
Identifying and reducing exposure to allergens is a cornerstone of managing seasonal allergies. Strategies include keeping windows closed during high pollen times, using air filters, showering after spending time outdoors, and regularly washing bedding. Over-the-counter or prescription medications such as antihistamines, nasal corticosteroids, and decongestants can also help mitigate symptoms.
Although the link between seasonal allergies and food sensitivities might not be immediately obvious, emerging research suggests a significant overlap. Understanding the core aspects of seasonal allergies provides a solid foundation for exploring this fascinating and complex relationship.
Common Food Sensitivities
Many people might not realize that food sensitivities can often go hand-in-hand with seasonal allergies. If you've ever found yourself sneezing uncontrollably after a meal, it's possible that something you ate is contributing to your symptoms. Foods like peanuts, dairy, and gluten are well-known for causing problems, but there are also lesser-known culprits that might surprise you.
For those with seasonal allergies, the concept of oral allergy syndrome (OAS) is essential to understand. OAS occurs when certain fruits and vegetables cause allergic symptoms because their proteins are similar to those in pollen. For example, people allergic to birch pollen often react to apples, carrots, and celery. If you notice a tingling sensation in your mouth or throat after eating specific raw foods, OAS might be the issue.
Interestingly, cooking or peeling these foods can sometimes eliminate the problem. The heat alters the proteins enough that the immune system no longer recognizes them as a threat. Citrus fruits, tomatoes, and nuts are also common triggers for many people. If your body is already dealing with pollen, it’s more likely to react to these foods as well.
According to Dr. Clifford Bassett, a leading allergist, "Understanding the relationship between food and seasonal allergies is crucial for managing symptoms effectively. Sometimes, avoiding certain foods during peak pollen season can make a significant difference."
Another factor is histamine. Certain foods like aged cheeses, red wine, and smoked meats contain high levels of histamine, which can amplify allergy symptoms. If you’re already dealing with a high pollen count, consuming these foods could make you feel even worse. Keeping a food diary might help identify which foods trigger your symptoms. This way, you can avoid them or at least be more prepared to manage your reactions.
Maintaining good gut health is also key in managing food sensitivities. Probiotics and fermented foods like yogurt, sauerkraut, and kefir can help balance the bacteria in your gut, potentially reducing sensitivity levels. Drinking plenty of water can also help flush out histamines and other irritants.
You might be surprised to learn that some foods contain natural antihistamines. Foods like ginger, garlic, and onions can help reduce inflammation and support your immune system. Adding these to your diet can provide some relief from chronic symptoms. Turmeric and green tea have also shown promising results in managing allergic reactions.
Specific diets, such as the low FODMAP diet, have also been found beneficial. This diet helps identify and eliminate foods that cause digestive issues and allergies, providing a clearer picture of what might be contributing to your symptoms. Consulting with a nutritionist can offer personalized guidance based on your health needs.
The Immune System Connection
Our immune system is like a vigilant guard, always on the lookout for anything that might cause harm. When it comes to seasonal allergies, substances like pollen, mold, or pet dander can trigger an overzealous response. The body releases histamines and other chemicals that lead to the familiar symptoms of sneezing, itching, and congestion. But how does this relate to the food we eat?
Interestingly, the immune system’s role in food sensitivities can be quite similar. When you have a food sensitivity, certain substances in foods are mistaken as threats. This triggers an immune response that can cause various symptoms ranging from digestive issues to skin rashes. Some common food sensitivities include lactose, gluten, and certain types of nuts. The shared mechanism of an overreactive immune response is what connects seasonal allergies and food sensitivities.
There’s a fascinating concept known as Oral Allergy Syndrome (OAS). People with OAS may experience an itchy mouth or throat after eating certain fruits and vegetables. This happens because the proteins in these foods are similar to the proteins in plant pollen. For example, someone with a birch pollen allergy might react to apples or carrots.
According to Dr. Clifford Bassett, a leading allergist and founder of Allergy and Asthma Care of New York, "Birch pollen is structurally similar to proteins found in some fruits, vegetables, and nuts, which is why those with birch pollen allergies may experience OAS."
Research shows that around 50 to 70 percent of people with birch pollen allergies also have reactions to foods like apples, kiwis, and hazelnuts. It's like the immune system gets confused and can't tell the difference between the pollen it’s allergic to and the similar proteins in these foods. This means that managing seasonal allergies often involves being mindful of food sensitivities as well.
If you suspect that food is making your seasonal allergy symptoms worse, it’s a good idea to talk to a healthcare provider. They can recommend tests like skin prick tests or blood tests that can identify specific allergens. Keeping a food diary might also help you identify patterns and pinpoint the foods that trigger your symptoms. Eliminating or reducing these foods from your diet could potentially provide some relief.
Incorporating anti-inflammatory foods into your diet can also be beneficial. Foods rich in omega-3 fatty acids, like salmon and flaxseeds, can help reduce inflammation and support your immune system. Probiotic-rich foods such as yogurt and sauerkraut can promote gut health, which is crucial for a balanced immune response. Staying hydrated and maintaining a healthy diet can support your body in dealing with both seasonal allergies and food sensitivities more effectively.
Tips for Managing Symptoms
When it comes to managing the tricky relationship between seasonal allergies and food sensitivities, you have several options. Making changes in your lifestyle and diet can go a long way toward reducing discomfort and maintaining health. Here are some practical strategies to help alleviate symptoms.
First off, consider keeping a food and symptom diary. Documenting what you eat and how you feel afterward helps identify possible triggers. This approach is especially useful for uncovering hidden sensitivities, allowing you to avoid troublesome foods.
According to Dr. Anne Miranowski, an allergist and immunologist, "Keeping track of your diet and symptoms can provide valuable insights into what might be contributing to your allergy flare-ups."
Next, focus on boosting your immune system. Eating a diet rich in fruits and vegetables provides essential vitamins and minerals that can help your body respond less aggressively to allergens. Foods like citrus fruits, strawberries, broccoli, and spinach are packed with nutrients that support immune function.
Hydration is another key element. Drinking plenty of water can help thin mucus, making it easier to clear from your system. Aim for at least eight glasses of water a day, but adjust based on activity levels and climate conditions.
Consider supplementing your diet with probiotics. These beneficial bacteria can improve gut health, which plays a crucial role in your overall immune response. Foods like yogurt, kefir, and sauerkraut are excellent sources of probiotics.
Pay attention to the pollen count in your area and plan outdoor activities accordingly. High pollen counts can exacerbate seasonal allergies, so aiming for indoor activities on days when pollen levels are high is a smart move. You can usually find pollen counts on weather websites or apps.
Avoid cross-reactive foods if you know your trigger allergens. For example, if you're allergic to birch pollen, you might also react to apples, cherries, and almonds. Knowing these connections helps in selecting foods that won't worsen your symptoms.
Invest in an air purifier for your home, particularly your bedroom. These devices can help remove allergens from the air, providing a cleaner environment where you spend a lot of time. Look for purifiers with HEPA filters for the best results.
Regular cleaning is essential. Dust and vacuum your home frequently to reduce the accumulation of allergens like dust mites and pet dander. Using dust mite-proof covers on mattresses and pillows can also be a big help.
Medications and Natural Remedies
There are several medications available that can help manage both seasonal allergies and food sensitivities. Antihistamines are a common choice and can effectively reduce symptoms like sneezing and itching. For food sensitivities, enzyme supplements might help break down offending foods and reduce symptoms.
On the natural side, consider trying neti pots or nasal rinses. These tools can help flush out allergens and reduce congestion. Allergy eye drops can also provide relief if itchy, watery eyes are a problem for you.
Finally, managing stress is crucial. High stress levels can weaken your immune system, making you more susceptible to allergies and sensitivities. Practices like yoga, meditation, and deep-breathing exercises can help keep stress in check, providing benefits beyond just allergy relief.
By taking these steps, you can significantly reduce the impact of seasonal allergies and food sensitivities on your life. It’s always a good idea to consult with a healthcare provider before making significant changes to your diet or health routine. They can provide personalized advice and additional strategies tailored to your specific needs.




Sara Allen
OMG I literally couldnt breathe last spring cause i ate an apple and my throat felt like it was closing?? i thought it was just me but now i get it!! its the pollen!! i just started peeling all my fruit and it changed my life no more sneezing fits at dinner lol
Amina Kmiha
THE GOVERNMENT IS PUTTING POLLEN IN OUR FOOD TO MAKE US SICK!! I read this on a blog that got shut down by the CDC and it’s all connected to 5G and fluoride in the water!! WHY WON’T THEY TELL US THE TRUTH?? 🤡👁️🗨️💧
Ryan Tanner
Bro this is actually so helpful!! I’ve been blaming my allergies on my cat but turns out it’s the celery I snack on after mowing the lawn 🤯 Try peeling your apples and see what happens. Also, ginger tea is a game changer. You got this!! 🙌
Jessica Adelle
It is both a scientific and moral imperative to recognize that the degradation of our food supply-through industrial farming, genetic modification, and chemical preservatives-is directly responsible for the exponential rise in immune dysregulation. We must return to whole, unprocessed foods, or face the consequences of a nation of immunocompromised citizens.
Sai Ahmed
Interesting. But in India, we eat raw mangoes and spices daily during allergy season and never have problems. Maybe Western diets are too clean? Our bodies need real stress to stay strong. Also, why do you assume everyone has the same allergies? Not universal.
Albert Schueller
According to my cousin who works at Pfizer (he’s a ‘data analyst’), the FDA has known about this cross-reactivity since 2012 but suppressed the data because antihistamines make too much money. Also, the word ‘histamine’ is misspelled twice in this article. 🤔
Ted Carr
So let me get this straight. You’re telling me that eating an apple can trigger allergies… because it looks like pollen? That’s not science. That’s a Disney villain’s lab experiment. Next they’ll say my banana is secretly a birch tree in disguise.
Rebecca Parkos
THIS IS WHY I CAN’T EAT STRAWBERRIES ANYMORE!! I thought I was just being dramatic but NO. IT’S REAL. I CRIED IN THE GROCERY STORE LAST WEEK. I’M SO GLAD I’M NOT ALONE. WE NEED A SUPPORT GROUP. I’M STARTING ONE. DM ME.
Bradley Mulliner
Of course you have food sensitivities. You’re clearly emotionally unstable. Stress causes histamine release. You’re not allergic to apples-you’re allergic to not being in control. Also, probiotics are a scam. Your gut doesn’t need ‘balance.’ It needs discipline.
Rahul hossain
Back home in Kerala, we use turmeric paste on our faces during pollen season-no pills, no nasal sprays. The wisdom of our ancestors knew this long before Western science caught up. Also, your ‘low FODMAP’ diet? That’s just a fancy word for ‘I don’t like beans.’
Reginald Maarten
You say ‘OAS’ is common-but according to the 2021 Journal of Allergy and Clinical Immunology, prevalence is 0.8% among adults, not 50–70%. Also, you conflated ‘food sensitivity’ with ‘food allergy.’ They are not the same. And ‘histamine-rich foods’? Red wine contains 3–20 mg/L. That’s less than a banana. This article is misleading.
Jonathan Debo
It’s astonishing how casually the public accepts pseudoscientific generalizations. The notion that ‘cooking alters protein structure’ is not a universal rule-conformational epitopes vary by species, glycosylation patterns, and thermal denaturation thresholds. Also, you mention ‘neti pots’ as if they’re a panacea. Have you considered the biofilm risk? The CDC has issued warnings.
Robin Annison
I’ve noticed that when I stop stressing about allergies, my symptoms fade. Not because of diet or meds-but because I stopped fighting them. I used to panic every time my nose ran. Now I just sit with it. Breathe. Let it be. Weirdly, it gets better. Maybe the body just wants to be heard.
Abigail Jubb
I’ve been diagnosed with OAS, chronic fatigue, and existential dread. This article? It’s beautiful. I cried. Not because I’m dramatic-but because someone finally saw me. I eat only cooked pears now. I’ve stopped dating. I’ve started a journal. I’m not broken. I’m… evolved.
George Clark-Roden
It’s wild, isn’t it? That the same immune system that protects us from viruses also turns our favorite snacks into enemies… and that our bodies are just trying to make sense of a world full of mismatched signals. Maybe we’re not broken. Maybe we’re just… out of sync. With the earth. With our ancestors. With the rhythm of things. I think we’ve forgotten how to listen.
Sara Allen
u/3813 you’re literally the reason we can’t have nice things. apples are not government weapons. also stop using emojis. i’m not your therapist.