Opioid Restart: What It Means and How It Connects to Pain Management and Recovery
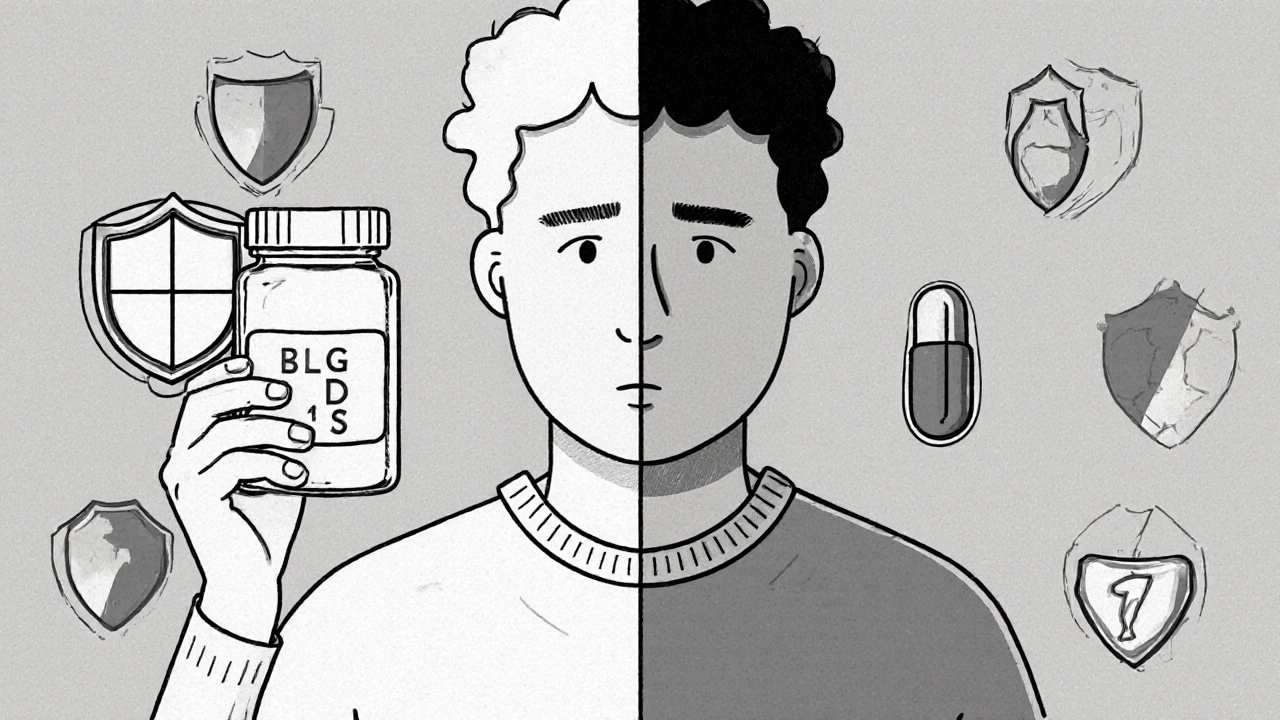
When someone talks about an opioid restart, the process of resuming opioid medication after a period of stopping, often under medical supervision. Also known as reinitiating opioid therapy, it’s not just about going back to pills—it’s a clinical decision shaped by pain control, addiction recovery, and safety. This isn’t something people do on their own. It happens in controlled settings, usually when chronic pain returns after a break, or when someone transitions from opioid use disorder treatment back to maintenance therapy.
One of the biggest concerns with an opioid restart, the process of resuming opioid medication after a period of stopping, often under medical supervision. Also known as reinitiating opioid therapy, it’s not just about going back to pills—it’s a clinical decision shaped by pain control, addiction recovery, and safety. is tolerance. Your body forgets how to handle opioids after even a few weeks off. Restarting at your old dose can be deadly. That’s why doctors often start low and go slow—sometimes using methadone, a long-acting opioid used in medication-assisted treatment for opioid use disorder. Also known as methadone maintenance, it helps stabilize brain chemistry and reduce cravings without the highs. or buprenorphine, a partial opioid agonist used to treat opioid addiction by reducing withdrawal and cravings with lower overdose risk. Also known as Suboxone, it’s one of the safest tools for long-term recovery.. These aren’t just substitutes—they’re tools that help your brain readjust without triggering relapse or respiratory depression. And they’re often paired with counseling, because recovery isn’t just about chemistry—it’s about behavior, environment, and support.
Many people think opioid restart means failure. But in reality, it’s often part of a longer journey. Someone might stop opioids after surgery, then need them again for chronic back pain. Or someone in recovery might relapse and re-enter treatment. What matters isn’t the restart—it’s how it’s done. Monitoring, dose titration, and avoiding combinations with other sedatives like gabapentin or alcohol are non-negotiable. The posts below cover exactly these real-world scenarios: how methadone and buprenorphine compare, why respiratory depression spikes when opioids mix with other drugs, and how patients and doctors navigate these decisions together. You’ll find practical advice on managing side effects, avoiding errors, and understanding what works—not just what’s advertised.