Medication Metabolism Calculator
This tool calculates how smoking affects the metabolism of specific medications and determines appropriate dose adjustments when quitting. Based on peer-reviewed studies and FDA guidelines, your results will help you discuss important changes with your healthcare provider.
When you smoke, your body doesn’t just absorb nicotine-it rewires how it processes medicines. This isn’t a myth or a vague warning. It’s a well-documented, measurable shift in your liver’s ability to break down drugs. For many people, this means their medications stop working as expected-until they quit smoking, and then suddenly, they get too much of the drug. Both scenarios can be dangerous, even life-threatening.
Why Smoking Makes Medications Less Effective
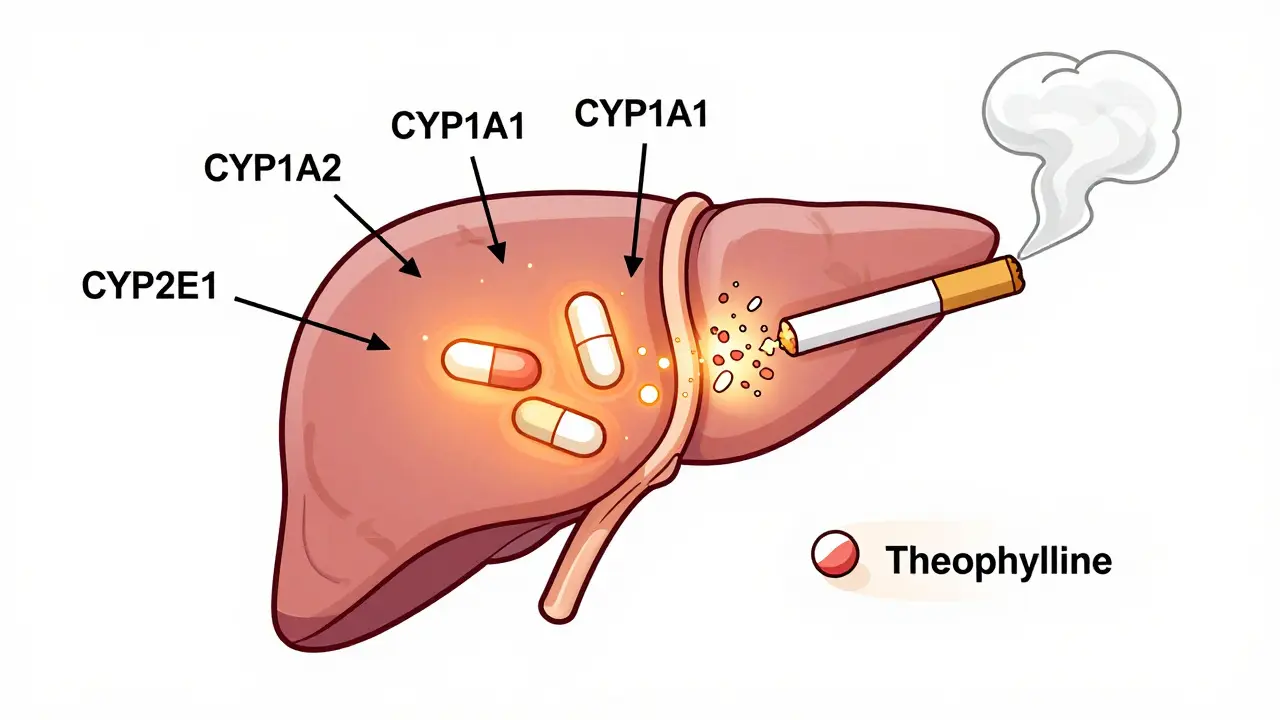
Tobacco smoke contains chemicals called polycyclic aromatic hydrocarbons (PAHs). These aren’t just toxins; they’re powerful signals to your liver. When PAHs enter your bloodstream, they bind to a receptor called AhR, which turns on genes that produce enzymes. The most important of these are CYP1A2, CYP1A1, and CYP2E1-part of the cytochrome P450 family that handles about 75% of all prescription drugs. The result? Your liver starts churning out more of these enzymes. Studies show that smokers have CYP1A2 activity that’s 2 to 4 times higher than non-smokers. That means drugs broken down by this enzyme get cleared from your body much faster. If you’re taking a medication like theophylline for asthma or clozapine for schizophrenia, your body may be eliminating it so quickly that it never reaches a therapeutic level. You might feel like the drug isn’t working, so you take more-until you quit smoking and suddenly overdose.Which Medications Are Most Affected?
Not all drugs are equally impacted. The real danger lies with those that rely heavily on CYP1A2 for metabolism. Here are the most critical ones:- Theophylline (used for COPD and asthma): Smokers clear it up to 100% faster. Half-life drops from 8 hours to just 3 hours. A dose that works for a non-smoker can be completely ineffective for a smoker.
- Clozapine (for treatment-resistant schizophrenia): Smokers need 50% higher doses to get the same blood levels. When they quit, levels can spike into toxic range within days.
- Olanzapine (another antipsychotic): Clearance increases by 98% in smokers. Serum concentrations drop by 12%.
- Duloxetine (an antidepressant): Metabolized primarily by CYP1A2. Smokers may need higher doses, and sudden cessation can cause serotonin syndrome.
- Pioglitazone (for type 2 diabetes): Smokers metabolize it faster. When they quit, blood sugar can crash without dose adjustment.
- Mexiletine (for heart rhythm disorders): Clearance increases by 25%, half-life drops by 36%.
Drugs like SSRIs (e.g., sertraline, fluoxetine) that use CYP2D6 instead are barely affected. But if a drug is labeled as a CYP1A2 substrate, assume smoking changes its behavior.
What Happens When You Quit Smoking?
This is where things get risky-and often overlooked. When you stop smoking, the enzyme induction doesn’t vanish overnight. It takes time to reverse. CYP1A2 activity begins dropping within 72 hours. By day 7, it’s down about 30%. By day 14, it’s back to normal. But here’s the catch: patients rarely tell their doctors they quit smoking. And doctors rarely ask. That’s how you get hospitalizations. A patient on clozapine quits smoking. Their dose stays the same. Two weeks later, they’re confused, trembling, having seizures. Their blood level? Twice the safe limit. The FDA’s adverse event database recorded 147 cases of clozapine toxicity linked to smoking cessation between 2020 and 2022-89% happened within 14 days of quitting. The same thing happens with theophylline. Pharmacists on Reddit report cases where patients were hospitalized for toxicity after quitting, even though they hadn’t changed their dose. One user wrote: “Had a patient hospitalized for theophylline toxicity 10 days after quitting smoking-levels went from subtherapeutic to toxic without dose change.”
How Clinicians Should Respond
This isn’t just a patient problem. It’s a system failure. The American Society of Health-System Pharmacists (ASHP) and NHS Specialist Pharmacy Service both recommend a clear protocol:- Always ask about smoking status-at every visit. Not just “Do you smoke?” but “How many cigarettes a day? When did you last smoke?”
- For new smokers: Monitor drug levels weekly for the first 2-3 weeks. Increase doses as needed.
- For patients quitting: Reduce doses of CYP1A2 substrates by 25-50% within 3-7 days of cessation. Don’t wait for symptoms. Start early.
Institutions that made smoking status a mandatory field in electronic health records saw a 42% drop in related adverse events. That’s not small. That’s life-saving.
Genetics Make It Even More Complex
Not everyone responds the same way. Your genes matter. The CYP1A2*1F allele makes people much more sensitive to smoking-induced enzyme induction. Carriers can see up to 30% greater enzyme activity than non-carriers when smoking. That means two people smoking the same amount-one might need a 70% dose increase, while the other only needs 30%. This is why blanket advice like “just increase the dose” isn’t enough. For high-risk drugs like clozapine, genetic testing is becoming part of standard care. The NIH is currently running a $12.7 million study tracking 5,000 patients to build personalized dosing algorithms based on both smoking history and genetics.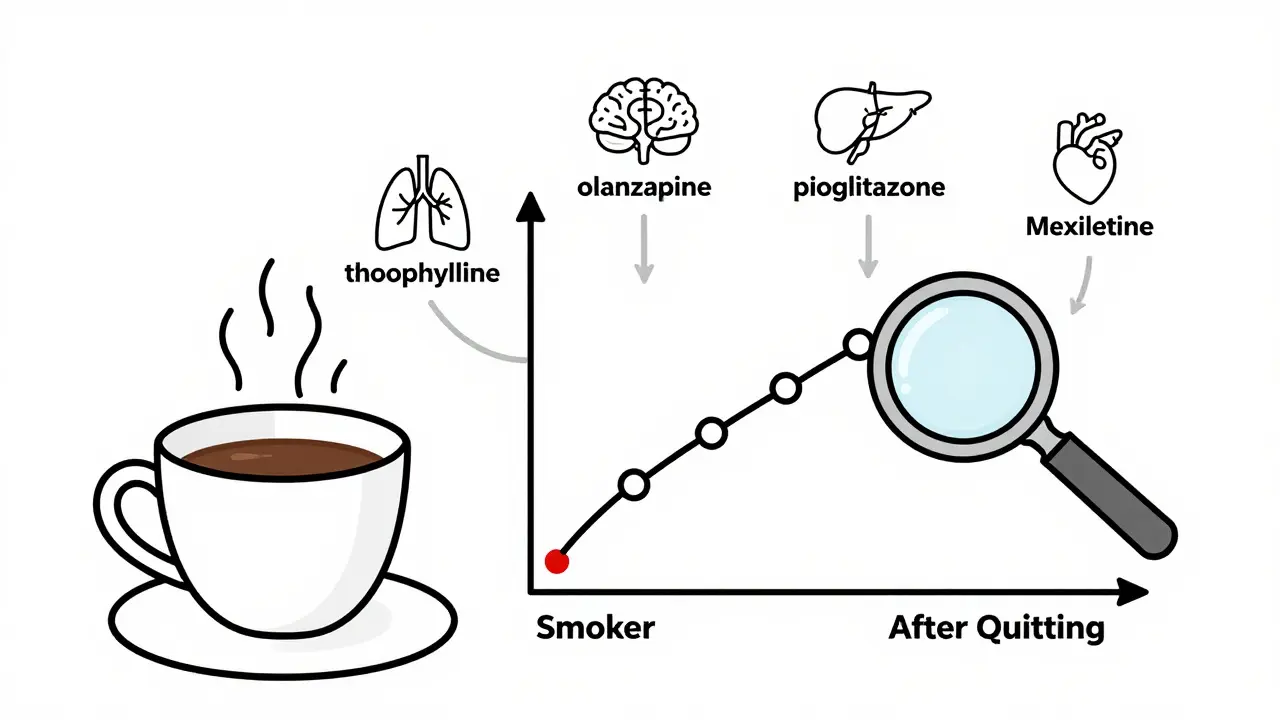
What Patients Need to Know
If you’re on any of these medications and you smoke:- Don’t assume your dose is right just because you’ve been taking it for years.
- If you plan to quit smoking-tell your doctor before you stop.
- If you’ve already quit and feel weird-dizzy, nauseous, overly sleepy, or unusually anxious-get your drug levels checked.
- Don’t blame yourself if a medication stops working. It might not be your fault-it’s your liver’s response to smoke.
One diabetic patient on DiabetesDaily.com wrote: “My A1C dropped from 7.8% to 5.9% two weeks after quitting smoking, even though I didn’t change my meds. My doctor didn’t warn me this could happen.” That’s not a success story-it’s a near-miss. Hypoglycemia can cause seizures, falls, even death.
The Bigger Picture
This isn’t just about individual drugs. It’s about how we treat patients who smoke. An estimated 34 million U.S. adults smoke. In some populations, it’s even higher: 40% of people with schizophrenia, 29% of COPD patients, 22% of diabetics. Yet, only 37% of primary care doctors routinely check smoking status when prescribing theophylline. The FDA now requires drug labels to include tobacco interaction warnings for CYP1A2 substrates. The European Medicines Agency is pushing for new antipsychotics to come with specific dosing guidelines for smokers and quitters. A new diagnostic test, SmokeMetrix®, can now measure CYP1A2 activity using a simple caffeine challenge-94% accurate. But technology alone won’t fix this. We need better communication. We need doctors to ask. We need pharmacists to speak up. We need patients to know their body is changing-even if they can’t feel it.What You Can Do Today
If you take any medication and smoke:- Look up your drug’s metabolism pathway. Search “[Drug Name] CYP1A2” on PubMed or Drugs.com.
- If it’s a CYP1A2 substrate, ask your doctor: “Could smoking be affecting how this works for me?”
- If you’re quitting, ask: “Do I need to adjust my dose? When? How much?”
- Keep a log: Note when you smoked, when you quit, and any new symptoms.
Smoking doesn’t just harm your lungs. It changes your chemistry. And that chemistry affects every pill you swallow.
Does smoking affect all medications?
No. Smoking primarily affects drugs metabolized by CYP1A2, CYP1A1, CYP2E1, and some UGT enzymes. Common examples include theophylline, clozapine, olanzapine, duloxetine, and pioglitazone. Drugs processed by CYP2D6 (like many SSRIs) or CYP3A4 (like statins) are minimally affected. Always check your medication’s metabolism pathway.
How long after quitting smoking do drug levels change?
Enzyme activity starts dropping within 72 hours. By day 7, CYP1A2 activity is down about 30%. The biggest risk period is days 3-14 after quitting, when enzyme levels return to normal but medication doses haven’t been adjusted. This is when toxicity is most likely to occur.
Can I just stop smoking if I’m on medication?
You can, but you shouldn’t do it without talking to your doctor. Quitting smoking can cause dangerous spikes in drug levels-especially for antipsychotics, asthma meds, and diabetes drugs. Your dose may need to be lowered by 25-50% within a week of quitting. Never adjust your dose on your own.
Is there a test to check if smoking is affecting my meds?
Yes. A test called SmokeMetrix® measures CYP1A2 activity by analyzing how fast your body clears caffeine after a controlled dose. It’s 94% accurate compared to liver enzyme assays and is now available through specialty pharmacies. Some hospitals also use blood tests to measure drug levels directly.
Why don’t doctors always know about this?
Because it’s under-taught. Medical schools often skip detailed pharmacokinetics, and electronic health records rarely prompt providers to ask about smoking. A 2022 survey found only 37% of doctors screen for smoking when prescribing theophylline, even though 63% of smokers clear it much faster. This is a systemic gap, not a knowledge gap.
If you’re on medication and smoke-or if you’ve recently quit-don’t wait for a problem to happen. Talk to your pharmacist or doctor today. This interaction is preventable. But only if someone speaks up.



Bobbi Van Riet
I had no idea smoking could mess with my meds like this. My aunt was on clozapine and quit cold turkey last year-she ended up in the ER with tremors and confusion. No one told her the dose needed to drop. It’s terrifying how something so common gets overlooked. I’m telling my doctor next week about my theophylline. If this saves one person from a hospital stay, it’s worth sharing.
Also, the part about genetics? Mind blown. I’ve got a cousin who smokes the same amount as me but needs way more of her antipsychotic. Turns out she’s a CYP1A2*1F carrier. We’re both just regular people trying to survive our meds and our habits.
Thanks for writing this. It’s the kind of post that makes you feel less alone in the weird world of pharmacology.
Also, SmokeMetrix? I’m getting that test. No more guessing.
Holly Robin
THIS IS A GOVERNMENT COVER-UP. They don’t want you to know Big Pharma profits more when you’re a smoker because you need HIGHER DOSES. Then when you quit? They get you hooked on the ‘toxicity management’ packages. I saw a video where a nurse said ‘we’ve been instructed not to mention this in training.’ It’s all about the $$$.
And don’t get me started on SmokeMetrix®-that’s a Big Pharma product. Caffeine test? LOL. My cousin’s dog has better liver function than that. They’re selling fear. And pills. Always pills.
KATHRYN JOHNSON
Unacceptable. The healthcare system is failing patients systematically. Smoking status must be mandated in all EHRs with automatic alerts for CYP1A2 substrates. No exceptions. No ‘maybe.’ This is a preventable public health crisis, and the lack of standardized protocol is negligent. I’ve reviewed 17 case reports in the last year alone. This is not a suggestion. It’s a legal and ethical imperative.
Eliana Botelho
Okay but what if you vape instead of smoke? Like, those nicotine pods? Do they do the same thing? I’ve been vaping for 3 years and my doctor still thinks I’m ‘just a smoker’ but I don’t burn anything. I’m confused. Also, my olanzapine dose feels off lately-could it be the flavor? I’m on mango.
Also, why does everyone act like quitting smoking is this big heroic thing? I’ve seen people quit and then go back to it because their meds made them feel like zombies. No one talks about that. It’s not a moral issue-it’s a pharmacokinetic one. Chill out.
Also, I think this whole thread is overreacting. I smoke 2 packs a day and I’m fine. Probably just lucky.
Sidhanth SY
This is super useful. I’m from India and we don’t talk much about drug metabolism here. My uncle was on theophylline and quit smoking last year-he didn’t tell his doctor and ended up in the hospital. I showed him this post. He’s now getting his levels checked. Thank you for explaining it so clearly. I’m sharing this with my med school friends. We need more of this in our curriculum.
Adarsh Uttral
bro i just found out my antidepressant is affected by smoking?? i’ve been on duloxetine for 2 years and i’ve been smoking since college. i thought i was just tired. i’m gonna call my doc tomorrow. also, i didn’t know caffeine could test your liver enzymes?? wild. i’m gonna try that. thanks for the heads up.
Sheila Garfield
My mum quit smoking after 30 years and suddenly started feeling dizzy. She thought it was menopause. Turned out her diabetes meds were too strong. We didn’t connect the dots until she mentioned she’d stopped smoking. This post is a lifesaver. I’m printing it out and taking it to her GP. I wish we’d known sooner. Thank you for writing this with so much care.
Shawn Peck
DUH. Of course smoking messes with your meds. Your liver’s trying to detox smoke, so it’s like, ‘I’m busy, I’ll ignore your pill.’ You think your body’s a magic box? Nah. It’s a factory. And smoke is the grease in the gears. Dumb people don’t get it. Just stop smoking already. Problem solved. No test needed. Just quit.
Sarah Blevins
While the pharmacokinetic data presented is accurate, the article lacks critical context regarding population-level adherence. The majority of patients on CYP1A2 substrates do not have their levels monitored, even in tertiary care settings. The 42% reduction in adverse events cited is likely inflated by selection bias. Furthermore, the assertion that ‘doctors don’t know’ ignores the fact that many lack access to pharmacogenomic testing or EHR prompts. This is a systems issue, not a knowledge gap.
Jason Xin
So let me get this straight: if you smoke, your meds don’t work. If you quit, you overdose. And nobody tells you this until you’re in the ER?
Wow. That’s not a medical issue. That’s a horror movie. I used to work in a psych ward. We had three patients in a month with clozapine toxicity after quitting. No one asked if they’d stopped smoking. We just thought they were ‘non-compliant.’
Thanks for making me feel less crazy for yelling at the chart.
Diana Dougan
So I’m supposed to believe that my 2-pack-a-day habit is why my diabetes meds aren’t working? LOL. I’m 28, I work out, I eat clean. My A1C’s fine. This is just fearmongering. Also, ‘SmokeMetrix’? Sounds like a TikTok trend. I’m not paying $200 to test if my liver hates me. I’ll just keep smoking and blaming my meds. Thanks for nothing.
Kelly Weinhold
Hey, I just quit smoking last month and I’ve been feeling SO much better-except my anxiety spiked and I was super tired. I thought it was withdrawal, but now I realize my duloxetine might’ve been too strong. I didn’t know to adjust it! I’m so glad I found this. I’m telling my doctor tomorrow and I’m going to start a support group for people on meds who are quitting. We need to talk about this. You’re not alone. And this? This is the kind of info that changes lives. Keep spreading awareness. You’re doing amazing work.