Cyclosporine Dose Assessment Tool
Cyclosporine Monitoring Calculator
This tool helps assess whether your cyclosporine levels and kidney function are in the safe range. Based on your data, it calculates your risk of nephrotoxicity and suggests appropriate actions.
Your Risk Assessment
When you take cyclosporine after a kidney, heart, or liver transplant, it’s not just about preventing rejection. It’s about staying alive without wrecking your kidneys. Cyclosporine is powerful-it keeps your immune system from attacking your new organ. But it’s also one of the most dangerous drugs you can take if not watched closely. About cyclosporine nephrotoxicity affects 25% to 75% of transplant patients, and in many cases, it’s the reason a transplanted kidney fails years later. This isn’t rare. It’s predictable. And it’s preventable-if you know how to monitor it right.
Why Cyclosporine Is So Risky
Cyclosporine works by blocking calcineurin, a protein that tells your immune cells to attack. That’s great for stopping rejection. But calcineurin is also involved in keeping your kidneys healthy. When you block it too much, your kidney’s tiny blood vessels tighten up. Blood flow drops. Pressure builds. Over time, this causes scarring, thickened artery walls, and damaged tubules. The damage starts quietly-no pain, no swelling. By the time creatinine rises, you’ve already lost kidney function. The problem isn’t just the drug. It’s the window. Cyclosporine’s therapeutic range is razor-thin. Too low, and your body rejects the transplant. Too high, and your kidneys start shutting down. For kidney transplant patients, the target range shifts over time: 200-400 ng/mL in the first week, then slowly dropping to 75-160 ng/mL after a year. But here’s the catch: two people can take the same dose and have completely different blood levels. One might be safe. The other could be heading for kidney failure.How Blood Levels Are Measured-And Why It Matters
Not all lab tests for cyclosporine are created equal. In 2025, most U.S. transplant centers use liquid chromatography-tandem mass spectrometry (LC-MS/MS). It’s the gold standard because it measures only the active drug, not its metabolites. Older methods-like immunoassays-can give false highs. Why? Because they can’t tell the difference between cyclosporine and its breakdown products. That’s dangerous. A falsely high reading might lead a doctor to lower your dose, putting you at risk for rejection. A falsely low reading might make them increase your dose, pushing you into kidney damage. LC-MS/MS is accurate to within 99.2%. It can detect levels as low as 5 ng/mL. That’s critical because small changes matter. A rise from 140 to 160 ng/mL might mean nothing in an immunoassay-but in LC-MS/MS, it’s a red flag. Labs that still use immunoassays have 10-15% more dosing errors. And those errors? They lead to graft failure.When to Test: Trough vs. C2 Monitoring
Traditionally, doctors checked cyclosporine levels right before your next dose-the trough or C0 level. But that’s like checking your gas tank only when you’re already out of fuel. Research since 2018 shows that measuring cyclosporine two hours after you take your pill-the C2 level-gives a much better picture of how much drug your body is actually absorbing. C2 levels correlate with the total drug exposure over 12 hours (AUC) with 87% accuracy. Trough levels? Only 63%. That’s why centers using C2 monitoring saw a 22.4% drop in nephrotoxicity between 2015 and 2023. The American Journal of Transplantation now recommends C2 for all patients in the first six months. After that, if levels are stable, you might switch back to troughs. But timing matters. If you take your pill at 8 a.m., you can’t test at 10 a.m. and then go to lunch. You have to wait exactly two hours. Miss that window, and the number is useless. And you can’t just grab any blood tube. You need EDTA tubes. Serum separator tubes can give falsely high results by 15-20% because cyclosporine sticks to the gel. That’s enough to trigger a dangerous dose change.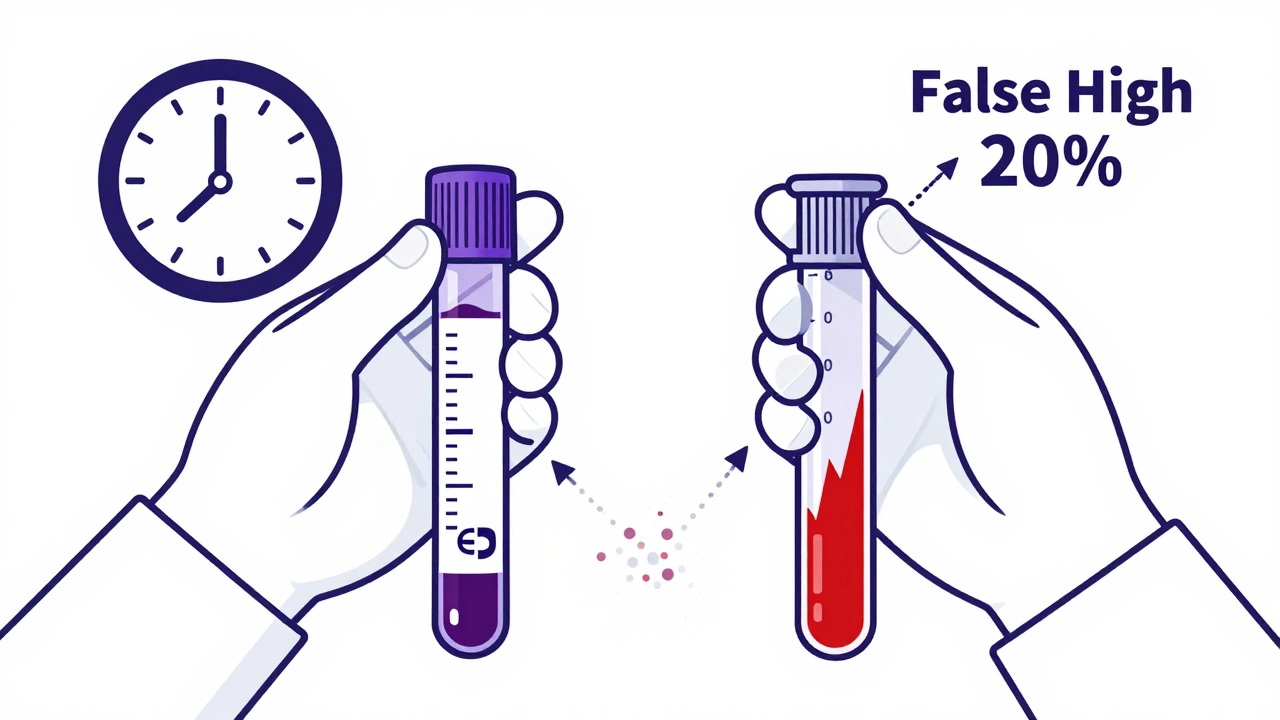
What Else to Watch: Kidney Function Beyond Blood Levels
You can’t rely on cyclosporine levels alone. You need to track your kidneys directly. Here’s what matters:- Serum creatinine: Keep it under 1.5 mg/dL. A rise of 0.3 mg/dL in a week is a warning sign.
- BUN-to-creatinine ratio: Should be under 20:1. Higher ratios suggest reduced kidney blood flow.
- Blood pressure: Must be below 130/80 mmHg. Cyclosporine raises blood pressure in 50% of patients.
- Magnesium: Low levels (below 1.7 mg/dL) are common and linked to kidney damage. Many patients need supplements.
- Uric acid: Often elevated. Not always harmful, but high levels can worsen kidney stress.
Drugs That Change Cyclosporine Levels-And What to Do
Cyclosporine is broken down by liver enzymes called CYP3A4. Many common drugs interfere with this. Here’s what can wreck your levels:- Ketoconazole, fluconazole, diltiazem: Can raise cyclosporine by 30-50%. If you’re on one of these, your dose needs to drop by 30-50%.
- Rifampin, phenytoin, St. John’s wort: Can slash cyclosporine levels by 40-60%. You might need a 50% increase.
- Macrolide antibiotics (like clarithromycin): Increase levels. Avoid if possible.
- Calcium channel blockers: Can raise levels. Monitor closely.
How Often Should You Get Tested?
The schedule isn’t one-size-fits-all. But here’s what most centers follow:- Weeks 1-4: Twice a week. Your body is adjusting. Levels swing wildly.
- Weeks 5-24: Once a week. Still high risk for rejection and toxicity.
- Months 7-12: Every two weeks.
- After one year: Monthly, if stable. But if your creatinine climbs or you start a new drug, go back to weekly.

Can the Damage Be Reversed?
Yes-if you catch it early. Studies show that if you lower your cyclosporine dose within three months of seeing kidney damage, about 60-70% of patients recover some function. The scarring stops. Blood flow improves. Creatinine drops. But if you wait six months? Recovery drops to under 30%. And after a year? The damage is often permanent. That’s why monitoring isn’t optional. It’s survival. You can’t feel this damage coming. You have to test for it.What’s Next? The Future of Monitoring
The future is faster and smarter. Point-of-care devices that measure cyclosporine in whole blood in under 15 minutes are in Phase 3 trials and expected to get FDA approval in late 2025. Imagine getting your level back in the clinic while you wait-no lab, no wait, no guesswork. AI tools are also being tested. One system analyzes 17 variables-your weight, liver enzymes, diet, other meds, even your genetic profile-to predict the perfect dose. Early results show 89.7% accuracy. That could mean fewer blood draws and fewer mistakes. But here’s the truth: none of that matters if you skip your tests. The most advanced tech in the world won’t help if you don’t show up. Cyclosporine isn’t a drug you take and forget. It’s a daily balancing act. And the scale is your kidneys.How do I know if cyclosporine is hurting my kidneys?
You won’t feel it. The only way to know is through regular blood tests: check your creatinine, BUN, magnesium, and blood pressure. A rising creatinine-even by 0.3 mg/dL-is a red flag. If your cyclosporine level is high at the same time, the risk is clear. Don’t wait for swelling or fatigue. By then, it’s too late.
Is a C2 level test better than a trough level?
Yes, especially in the first six months after transplant. C2 levels (taken two hours after your dose) show how much drug your body absorbs over time. Trough levels (taken right before your next dose) only show the lowest point. Studies prove C2 monitoring cuts kidney damage by over 20%. Most transplant centers now recommend it.
Can I take other medications with cyclosporine?
Some are safe. Many are not. Antibiotics like clarithromycin, antifungals like ketoconazole, and even St. John’s wort can dangerously raise or lower your cyclosporine levels. Always check with your transplant team before taking anything new-even vitamins or herbal supplements. A simple change can trigger rejection or kidney failure.
What blood tube should I use for cyclosporine testing?
You must use EDTA tubes (purple top). Serum separator tubes (red or gold top) can give falsely high results by 15-20% because cyclosporine sticks to the gel. If your lab uses the wrong tube, your dose could be adjusted incorrectly. Always confirm your lab uses EDTA.
Can I stop taking cyclosporine if my kidney function improves?
Never stop or reduce cyclosporine without your transplant doctor’s direction. Even if your kidneys look better, stopping the drug can cause your body to reject your transplant within days. If your kidneys are damaged, your doctor may lower your dose-but they’ll likely add another immunosuppressant to make up for it. Never adjust on your own.
How long does it take for kidney damage from cyclosporine to become permanent?
If caught within three months of early signs, damage is often reversible. After six months, recovery becomes unlikely in most cases. Beyond one year, scarring is typically permanent. That’s why monthly monitoring isn’t optional-it’s your best defense against losing your transplant.
What to Do Next
If you’re on cyclosporine, here’s your action plan:- Confirm your lab uses LC-MS/MS, not immunoassay.
- Ask if you’re being tested for C2 levels, not just troughs.
- Make sure they’re using EDTA tubes.
- Keep a log of your creatinine, blood pressure, and magnesium levels.
- Never start a new medication without checking with your transplant team.
- Set phone reminders for your blood draws. Missing one could cost you your transplant.




Kshitij Shah
So let me get this straight - we’re giving people a drug that’s basically a slow-motion kidney assassin, and the only thing keeping them alive is remembering to take their blood tests like it’s a damn job? 🤦♂️
Sean McCarthy
Cyclosporine levels must be monitored. Trough is not enough. C2 is better. LC-MS/MS is required. EDTA tubes only. No other options. Failure to follow this leads to graft loss.
Jaswinder Singh
You people are still using immunoassays? Bro. I had my transplant in Mumbai and they switched to LC-MS/MS in 2020. If your lab is still giving you false highs, you’re not being cared for - you’re being experimented on. Get a new center. Now.
Bee Floyd
It’s wild how something so life-saving can also be so quietly destructive. Like, you’re not supposed to feel anything until it’s too late. That’s the real horror. Not the drug - the silence. I keep a little notebook. Creatinine. BP. Magnesium. Just so I can see the patterns. It’s not just medicine. It’s archaeology of your own body.
Jeremy Butler
The ontological implications of pharmacological monitoring in post-transplant immunosuppression are profoundly existential. One is compelled to confront the paradox of agency: the self is both the subject of intervention and the object of surveillance. The therapeutic window, in this context, becomes a metaphysical liminal space - a razor’s edge between life and annihilation.
Courtney Co
I just read this whole thing and now I’m crying. I’m so scared. I take cyclosporine and I forgot to check my magnesium last week. Is it too late? Do I already have kidney damage? I’m 28. I have a dog. I don’t want to die. Can you tell me I’m not going to die? Please? I’ll do anything.
Shashank Vira
Ah yes. The classic transplant narrative: ‘It’s preventable if you know how.’ As if ignorance is the only barrier to survival. Meanwhile, I’m paying $800 for a single blood test and my insurance denies C2 monitoring because it’s ‘not medically necessary’ in my state. The real toxicity isn’t the drug - it’s the healthcare industrial complex.
Jack Arscott
C2 monitoring changed my life. 🙌 I used to get random creatinine spikes and my doc would panic. Then we switched to C2 - boom. Stable. No more dose rollercoaster. Also, use purple tops. Seriously. Don’t be that guy with the red tube.
Matt Dean
You’re all overreacting. If you can’t follow basic monitoring protocols, you don’t deserve a transplant. It’s not complicated. Test. Log. Don’t take random pills. Done. Stop making it a drama.
Walker Alvey
So let me get this straight - we’re turning transplant recipients into lab rats on a schedule because the pharmaceutical industry can’t make a drug that doesn’t require a PhD to manage? Brilliant. Just brilliant. We’re not curing disease. We’re outsourcing survival to blood tubes and spreadsheets.
Adrian Barnes
The data is unequivocal. C2 monitoring reduces nephrotoxicity by 22.4%. LC-MS/MS reduces dosing errors by 92%. EDTA tubes are non-negotiable. Any deviation constitutes negligence. If your provider is not adhering to these standards, you are at unacceptable risk. Legal liability is imminent.
Declan Flynn Fitness
Mate, I’ve been doing this for 15 years. C2 is king. Purple top is law. And if your doc says ‘we’ll just check troughs’ - walk out. Go to a transplant center that treats this like the life-or-death thing it is. You’re not just a patient. You’re a survivor. Act like it. 💪
Michelle Smyth
The entire paradigm of cyclosporine monitoring is a postmodern epistemic failure. The reliance on pharmacokinetic metrics over phenomenological patient experience reflects a systemic dehumanization of care. One wonders whether the C2 protocol is merely a technocratic illusion masking deeper structural failures in transplant ethics.