Imagine getting sick every few weeks-not just a cold, but pneumonia, sinus infections, or stomach bugs that won’t quit. For people with Common Variable Immunodeficiency (CVID), this isn’t rare. It’s everyday life. CVID is one of the most common serious antibody deficiencies in adults, yet most people have never heard of it. And because it’s so hidden, many wait years before getting the right diagnosis.
What Is CVID, Really?
CVID is a genetic immune disorder where your body doesn’t make enough antibodies-specifically IgG, IgA, and sometimes IgM. These are the proteins your immune system uses to recognize and kill bacteria and viruses. Without them, you’re defenseless against common germs. Unlike allergies, where your immune system overreacts, CVID means it underperforms. You’re not allergic to pollen or peanuts; you’re allergic to life because your body can’t fight off the basics.
It’s not something you catch. It’s something you’re born with, but symptoms often don’t show up until your 20s or 30s. That’s why it’s often mistaken for chronic bronchitis, asthma, or even just bad luck with infections. The average person with CVID sees three or more doctors before getting diagnosed. And on average, they wait over eight years.
How Do You Know You Have It?
Doctors don’t diagnose CVID by symptoms alone. They need lab tests. The key markers are:
- IgG levels below 500 mg/dL (normal is 700-1600)
- IgA levels below 7 mg/dL (normal is 70-400)
- Poor response to vaccines like pneumococcus or tetanus
Even if your B cells (the immune cells that make antibodies) look normal under a microscope, they’re not doing their job. That’s the core problem: defective B cell function. You have the soldiers, but they don’t know how to fight.
One telltale sign? Recurrent lung infections. About 35% of CVID-related pneumonia cases are caused by Haemophilus influenzae, 28% by Streptococcus pneumoniae. These are the same bugs that cause ear infections in kids-but in CVID patients, they keep coming back, year after year.
Why Is CVID So Different From Other Immune Disorders?
CVID isn’t like X-linked agammaglobulinemia (XLA), where kids are born with almost no B cells at all. CVID patients usually have normal or even high B cell counts-they just can’t turn them into antibody factories. It’s not a shortage of parts; it’s a broken assembly line.
It’s also not the same as Selective IgA Deficiency, the most common primary immunodeficiency. People with that condition only lack IgA. Their IgG and IgM are fine. They might have mild allergies or digestive issues, but they rarely get life-threatening infections. CVID patients? They’re at risk for pneumonia, sepsis, and even cancer.
And here’s the scary part: 25% of CVID patients develop autoimmune diseases. That means their immune system starts attacking their own body-low platelets, anemia, arthritis. It’s like the immune system is confused. It can’t tell friend from foe.
What Happens If You Don’t Treat It?
Without treatment, CVID leads to permanent damage. About 65% of patients develop chronic lung disease by age 50. That’s not just bronchitis-it’s scarring, collapsed airways, and irreversible breathing problems. Some develop granulomas-clumps of immune cells that form in the lungs, liver, or skin-and these can mimic tuberculosis or cancer.
Then there’s the cancer risk. People with CVID are 20 to 50 times more likely to get lymphoma than the general population. That’s not a small increase. It’s a red flag. That’s why regular check-ups and scans are part of long-term care.
Before immunoglobulin therapy became standard in the 1980s, the average life expectancy for someone with CVID was just 33 years. Today? It’s 59. That’s the power of treatment.
How Is CVID Treated?
The only proven treatment is immunoglobulin replacement therapy. That means giving patients purified antibodies from donated human plasma. Think of it like a monthly blood transfusion-but instead of red blood cells, you’re getting protective proteins.
There are two main ways to get it:
- IVIG (intravenous): Delivered through a vein, usually every 3-4 weeks. Takes 2-4 hours per session.
- SCIG (subcutaneous): Injected under the skin, often weekly. Can be done at home after training.
Most patients get 400-600 mg per kg of body weight monthly for IVIG. For SCIG, it’s 100-150 mg per kg weekly. The goal? Keep IgG levels above 800 mg/dL. That’s the sweet spot where infections drop off sharply.
Patients on SCIG report fewer side effects. But it’s not perfect. About 25-40% get redness or swelling at injection sites. That’s why rotating spots and using smaller, more frequent doses helps.
IVIG has its own issues. About 32% of patients get infusion reactions: headaches (68%), chills (42%), nausea (37%). Some need to slow down the drip rate or take antihistamines beforehand.
It’s expensive. In the U.S., IVIG costs $65,000-$95,000 a year. SCIG runs $70,000-$100,000. Insurance covers most of it, but co-pays and out-of-pocket costs still hurt. And there’s a global plasma shortage-supply is 12% behind demand. Prices are expected to climb 15-20% yearly through 2028.
What’s New in CVID Treatment?
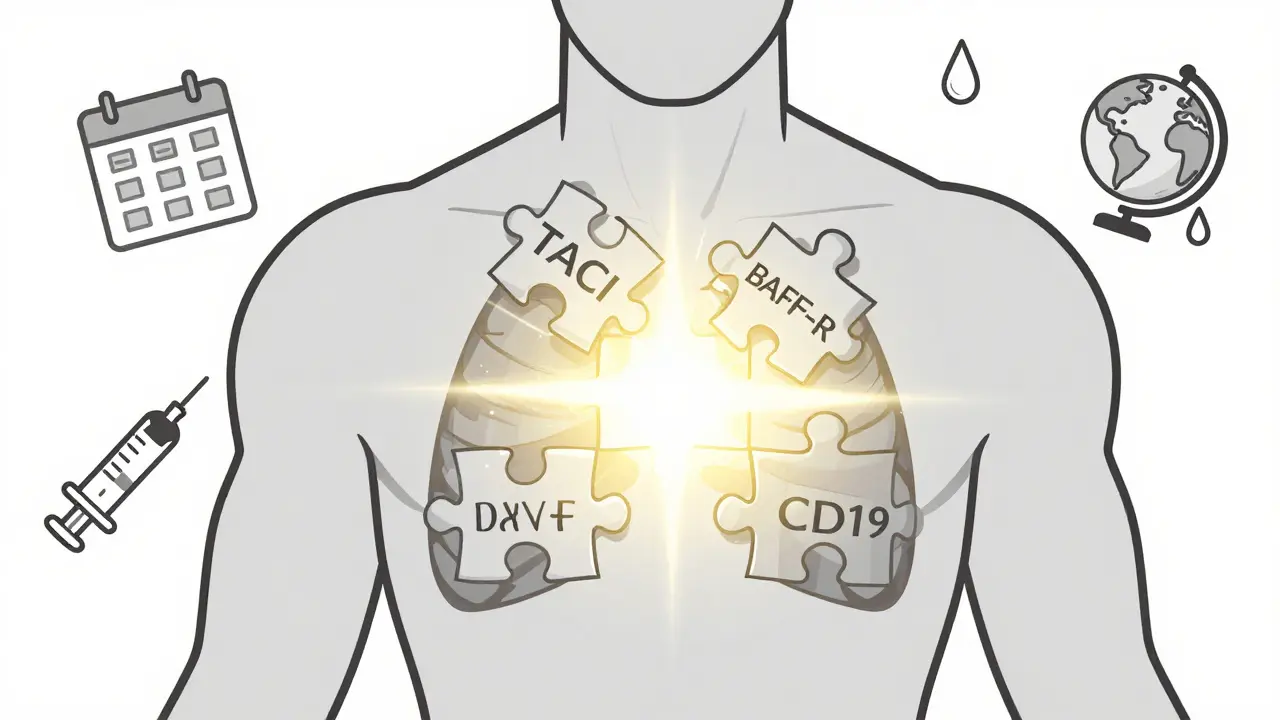
There’s hope beyond plasma. Researchers are working on targeted therapies. One drug, atacicept, blocks two proteins (BAFF and APRIL) that mess up B cell signaling. In a 2023 trial, it cut severe infections by 37% compared to standard therapy alone. It’s not a cure, but it could mean less frequent infusions or lower doses.
Genetic testing is also improving. Only 15-20% of CVID cases have known gene mutations today-like TACI, BAFF-R, or CD19. But scientists believe CVID isn’t one disease. It’s a group of similar disorders with different causes. That’s why some patients respond better to certain treatments than others.
Dr. Sergio Rosenzweig of the NIH predicts that within five years, we’ll classify CVID into subtypes based on genetics. That means personalized treatment: not just “antibodies for everyone,” but “this drug for your specific mutation.”
Life With CVID: Real Stories
People with CVID aren’t just patients-they’re people. On Reddit, one user said they lost 20 pounds in a year because their gut couldn’t absorb nutrients. Another said they had to quit their job because they were sick every six weeks. Fatigue? 74% report it. Weight loss? 48%.
But there’s also hope. A 2023 survey showed that 85% of people on SCIG saw their infections drop from over 10 a year to fewer than 3. Energy levels improved in 78% within three months.
Support matters. The Immune Deficiency Foundation runs over 200 local groups and hosts a 2,500-person annual conference. For many, it’s the first time they meet someone who gets it.
What You Should Do If You Suspect CVID
If you’ve had:
- Four or more ear or sinus infections in a year
- Two or more pneumonia cases
- Chronic diarrhea or weight loss with no clear cause
- Autoimmune disease like low platelets or anemia
-ask your doctor for an immunoglobulin panel. Don’t wait. The longer you go untreated, the more damage builds up.
Don’t settle for “you’re just prone to infections.” That’s not normal. It’s a red flag.
Final Thoughts
CVID isn’t curable. But it’s manageable. With the right treatment, most people live full, active lives. They work. They travel. They raise families. The key is early diagnosis and consistent therapy.
The science is moving fast. New drugs are coming. Plasma shortages are being addressed. And awareness is growing.
If you or someone you know is stuck in a cycle of infections that won’t go away, don’t ignore it. Get tested. Ask the right questions. You might be one blood test away from turning your life around.
Can CVID be cured?
No, CVID cannot be cured. It’s a lifelong condition caused by genetic defects in B cell function. But it can be effectively managed with regular immunoglobulin replacement therapy, which restores antibody levels and prevents serious infections. Most patients live normal lifespans with consistent treatment.
Is CVID the same as having low immunity from stress or poor diet?
No. CVID is a genetic disorder affecting antibody production. It’s not caused by lifestyle, stress, or nutrition. People with CVID have normal or high numbers of B cells, but those cells can’t produce functional antibodies. You can’t fix it with vitamins or sleep-it requires medical treatment.
Can children get CVID?
Yes, but it’s rare. Most cases are diagnosed in adults between ages 20 and 40. When it does appear in children, symptoms often start after age 5. Early-onset CVID tends to be more severe and may involve more autoimmune or gastrointestinal complications.
What are the side effects of immunoglobulin therapy?
IVIG can cause headaches, chills, nausea, or fever during infusion. SCIG often causes redness or swelling at injection sites. Both are usually mild and manageable. Serious reactions like anaphylaxis are rare. Most patients adapt over time, and dosing adjustments can reduce side effects.
Can I get vaccinated if I have CVID?
You can get inactivated vaccines (like flu shot, tetanus, hepatitis B), but live vaccines (like MMR or chickenpox) are dangerous because your immune system can’t control them. Always check with your immunologist before any vaccination. Your response to vaccines will also help confirm the diagnosis.
Is CVID hereditary?
Most cases are not inherited in a clear pattern. Only about 10-15% of CVID cases have a family history. Many cases result from new (de novo) gene mutations. However, if you have CVID, your siblings or children may have a slightly higher risk of immune disorders and should be monitored.
How often do I need to get immunoglobulin infusions?
IVIG is typically given every 3-4 weeks. SCIG is given weekly or every other week, often at home. The schedule depends on your weight, IgG levels, and how quickly your body clears the antibodies. Your doctor will adjust your dose based on your infection rate and trough IgG levels.
Can I travel with CVID?
Yes, many patients travel regularly. Plan ahead: carry a letter from your doctor, bring extra infusions on flights, and know where to get treatment abroad. Some patients use portable SCIG pumps for travel. Avoid areas with poor sanitation if you have GI complications. Always consult your immunologist before long trips.






Kiran Plaha
I never knew CVID was so common but so underdiagnosed. My cousin had constant pneumonia as a kid and they called it just bad luck. Turns out she had it. Early testing saved her lungs.
Wesley Pereira
So let me get this straight - you’re telling me people are paying $100k a year to get blood plasma because Big Pharma doesn’t want to cure it? 🤔
Meanwhile, I’m over here eating turmeric and doing breathwork and still catching colds. Coincidence? I think not.
Amy Le
USA needs to nationalize plasma collection. This isn’t healthcare - it’s a hostage situation. People are dying because billionaires own the supply chain. #CVIDisACrime
Saylor Frye
Interesting how they mention ‘genetic defects’ but never acknowledge the possibility of epigenetic triggers from environmental toxins. The real science is being buried under plasma profit margins.
Stuart Shield
I’ve seen this in rural India - folks with chronic infections dismissed as ‘weak constitution’. No labs, no diagnosis, just folk remedies and resignation. This post is a lifeline for people who’ve been told they’re just unlucky.
Venkataramanan Viswanathan
As someone from India where immunoglobulin therapy is nearly unaffordable, I can say this: awareness is the first step. But access? That’s the real battle. We need global equity in plasma distribution, not just American blog posts.
Pavan Vora
It’s fascinating… that CVID isn’t one disease, but many… and yet, we treat it as one… with plasma… which is… expensive… and… scarce… and… why… are we not… investing more… in… gene therapy…?
Susan Arlene
my friend got diagnosed last year after 7 years of being told she was just tired
now she’s hiking again
it’s wild how one blood test changes everything
Vinayak Naik
Man, this hits different. I used to think my chronic sinusitis was just allergies - turns out my B cells are like a team of ninjas who forgot their weapons. SCIG saved my job, my marriage, my sanity. I’m not just surviving - I’m living. And yeah, the injections suck, but they’re cheaper than funeral costs.
Some folks say ‘just boost your immune system’ - bro, I’ve tried garlic, zinc, acupuncture, sauna baths, and a 30-day juice cleanse. Nothing worked. Only the plasma did. Don’t let anyone gaslight you into thinking it’s all in your head.
I used to cry in the bathroom before work because I was too wiped to even brush my teeth. Now I take my SCIG on Tuesday nights, watch Netflix, and laugh at how much I used to stress over colds. It’s not a cure, but it’s a second chance.
And the cost? Yeah, it’s insane. But imagine if your kid couldn’t go to school because they got pneumonia every October. That’s the real cost. The price tag is just the invoice - the real bill is the years lost.
Doctors need to stop treating CVID like it’s a rare myth. It’s not. It’s hiding in plain sight. If you’ve had four ear infections in a year? Go get tested. Don’t wait eight years like I did.
And if you’re on IVIG and getting headaches? You’re not weak. You’re human. Adjust the drip rate. Take the Benadryl. Talk to your nurse. This isn’t weakness - it’s adaptation.
I’ve met people who’ve gone 20 years without diagnosis. Some lost their lungs. Some got lymphoma. Some gave up. I didn’t. Because I found this community. And now I’m telling you - don’t be silent. Ask for the test. Demand the panel. Your life depends on it.
Melanie Clark
So you're telling me the government allows private companies to hoard plasma while people die? That's not healthcare, that's eugenics by proxy. People with CVID are being punished for their biology and the system is complicit. This isn't science - it's capitalism with a stethoscope
Dana Termini
There’s so much pain hidden in this post. I’m glad someone’s talking about it without sugarcoating. I’ve watched my sister go from full-time worker to barely leaving the house - and then she got SCIG. She started cooking again. She laughed. That’s not just medicine - that’s love in vial form.
Ryan Barr
Plasma shortage. Price hikes. Corporate greed. All true. But stop blaming the system. Fix your own health. Get tested. Don’t wait for a savior.
Melanie Clark
Fix your own health? That’s what you say when you’ve never been too weak to stand up. My sister couldn’t even hold a spoon for six months. You think she chose this? You think she didn’t beg for help? You’re not helping. You’re silencing.